|
Table of Content - Volume 15 Issue 2 - August 2020
A study of association of urinary retention with level of spinal blockade
Jasa Ram Thakur1*, Vijay Kumar Sauhta2, Tsering Yougyal3, Dara Singh4, Kartic Syal5
1,2,3MD Anaesthesia, Department of Health and Family Welfare Hp Government, Operation Theatre Incharge Zonal Hospital Mandi District Mandi Himachal Pradesh, INDIA. 4,5Associate Professor Department of Anaesthesia Indira Gandhi Medical College Shimla, Himachal Pradesh, INDIA. Email: jassathakur821@gmail.com, d.sauhta@gmail.com, yougyal1001@gmail.com
Abstract Background: Post-operative urinary retention is a well-established and commonly encountered problem across all surgical specialties with an incidence ranging from 5% to 75%, in patients undergoing spinal anaesthesia. Aim and objective: To study the association of urinary retention with level of spinal blockade Methodology: Present study was a prospective study carried out in patients posted for lower limb /lower abdominal surgeries under spinal anaesthesia. Data was collected with pretested questionnaire. Data included demographic data like age, sex, socioeconomic status etc. detailed history of the patients was taken. A through clinical examination was done. Spinal anaesthesia was given to all patients. Patients were monitored throughout intraoperative period. Vital parameters like pulse, blood pressure, oxygen saturation and respiratory rate were measured. Level of sensory block was assessed and noted 10 minutes after giving the drug block in all the patients. All patients were closely followed for 24 hours post operatively for voiding and were graded into various voiding difficulty grades. Data was analysed with appropriate statistical tests. Results and discussion: Mean age of the patients was 49.3± 3.1 years. Male to female ratio was 4:1. Diabetes milletus and hypertension are risk factors for development of post operative urinary retention. There was no significant variation in post operative urinary retention in relation to height of sensory block level. Key Word: spinal blockade.
INTRODUCTION The control of micturition is a complex process involving multiple afferent and efferent neural pathways, reflexes and central and peripheral neurotransmitters. The perioperative period includes myriad insults that may interrupt this process and promote the development of urinary retention. There is a high incidence of micturition difficulties postoperatively. Acute post-operative urinary retention can occur following all types of anaesthesia and operative procedures. The etiology of postoperative urinary retention involves a combination of many factors, including surgical trauma to the pelvic nerves or to the bladder, over distention of the bladder by large quantities of fluids given intravenously, postoperative oedema around the bladder neck, and pain- or anxiety-induced reflex spasm of the internal and external urethral sphincters. Urinary retention is more likely to occur after major surgery and with elderly male patients. Opioids and confinement to bed may also be likely explanations for the development of urinary retention after surgery. Urinary retention, along with distress it causes, is an independent risk factor for increasing mortality due to high incidence of nosocomial UTI. There is 50% chance of patients getting UTI if patients are catheterized for more than 2 days8. Catheterization can cause significant pain, bladder discomfort, anxiety, and increased cost, resulting in prolonged hospital stays.1-3 Disturbances of micturition are common in the first 24 hours after spinal anaesthesia. There is a higher frequency of these disturbances after bupivacaine than lidocaine spinal anaesthesia. 4 After administration of spinal anaesthesia with bupivacaine or tetracaine, the micturition reflex is very rapidly eliminated. Detrusor muscle contraction is restored to normal 7–8 hours after the spinal injection. On average, patients recover enough motor function to be mobilized 1–2 hours before the micturition reflex returns. Full skin sensation is usually restored at the same time or slightly before patients are able to micturate. To avoid protracted postoperative bladder symptoms, careful supervision of bladder function is of great importance in patients receiving spinal anesthesia with long-acting anaesthetics. 4 Very few studies were carried out to find any association of urinary retention with level of blockade, so present study was conducted to find association between level of blockade and urinary retention.
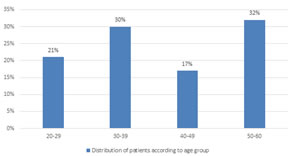
MATERIAL AND METHODS Present study was a prospective study carried out in patients posted for lower limb /lower abdominal surgeries under spinal anaesthesia. Study was carried out in 100 patients at Study population was 100 patients of ASA1 and ASA2 aged 20-60 years of either sex posted for lower limb /lower abdominal surgery under spinal anaesthesia. Inclusion Criteria: 1. Patients posted for lower limb/lower abdominal surgery under spinal anaesthesia 2. Patients of ASA 1 and ASA 2 3. Patients in age group of 20-60 years 4.Patients willing to participate in the study. Exclusion criteria: 1. Patients with urinary tract disease 2. Catherised patients. 3. Patients with warfarin 4. Patients with sitting systolic blood pressure in the upper extremity of less than 100 mmHg at the time of eligibility screening 5. Patients with Intra operative IV fluid more than 1500 ml 6. Patients with intraoperative blood loss more than 750 ml. Study was approved by ethical committee of the institute. A valid written consent was taken after explaining study to them. Data was collected with pretested questionnaire. Data included demographic data like age, sex, socioeconomic status etc. detailed history of the patients was taken. A through clinical examination was done. All patients underwent per operative assessment one day prior to surgery. Necessary investigations were done. Patients were catherized. All vital parameters were noted. With all aseptic precautions, intrathecal injection Bupivacaine (heavy) was given. Depending on the requirement of surgery drug was given. Patients were monitored throughout intraoperative period. Vital parameters like pulse, blood pressure, oxygen saturation and respiratory rate were measured. Level of sensory block was assessed and noted 10 minutes after giving the drug block in all the patients. All patients were closely followed for 24 hours post operatively for voiding and were graded into various voiding difficulty grades as given: Grade 0: Spontaneous voiding without difficulty. Grade 1: Voiding with difficulty. Grade 2: Intermittent single evacuation of bladder. Grade 3: Intermittent repeated evacuation of bladder Grade 4: Continuous catheterization. Data was entered in the excel sheet. Data was analysed with appropriate statistical tests. RESULTS In our study we studied 100 patients undergoing spinal anaesthesia. Out of total 100 patients 59 patients underwent lower limb surgeries and 41 patients underwent lower abdomen surgeries. Mean age of the patients was 49.3± 3.1 years. Majority of the patients were from the age group of 50-60 years (32%) followed by 30-39 years (30%). Patients in the age group of 20-29 years and 40-49 years were 21% and 17% respectively. In our study, 80% of the patients were male and 20 % patients were female. Male to female ratio was 4:1. Table 1 shows voiding difficulty in patients after spinal anaesthesia. Majority of the patients had spontaneous Voiding without difficulty G0 (60%). Voiding with difficulty (G1) was observed in 17% patients. Intermittent single evacuation of bladder (G2) was seen in 7% patients. Intermittent repeated evacuation of bladder (G3) was observed in 8% patients. Continuous catherization was seen in 8% patients. Thus in our study incidence of post operative urinary retention was 40%. Table 2 shows Voiding difficulty in patients according to sex. Out of total 100 patients 80 were male and 20 were female. Among male majority 47(58.75%)were not having any difficulty in voiding urine. 14 patients had grade 1 voiding difficulty and 4 patients had grade 2 voiding difficulty. In females 65% females did not have any difficulty in voiding urine after spinal anaesthesia. Males show higher difficulty in voiding urine than females but the difference was not statistically significant (p>0.05). In our study, 75 patients were without any associated co morbidity. 10% patients had Diabetes milletus. Hypertension and respiratory diseases were seen in 7% and 6% patients respectively. One patient had both diabetes and hypertension. Table 3 shows voiding difficulty in relation to co morbidities. In patients with diabetes milletus 7/10 (70%) patients required catherization. In respiratory diseases 2/6(33.33%) patients required catherization. In hypertensive patients 6/7 (85.71%) patients required catherization. The patient with both DM and hypertension required catherization. Thus we can say that Diabetes milletus and hypertension are risk factors for development of post operative urinary retention. able 4 shows voiding difficulty in relation to sensory block. In our study, out 100 patients, majority of the patients had T6 blockade (53%) followed by T5 (31%). We found that maximum height of sensory level was T4 and minimum being T8 sensory level. T 7 blockade was observed in 12% patients. T4 and T8 level blockade was observed in 2% patients each. In T6 level blockade 8/53 (15.09%) patients required catherization. In T5 level blockade 13/31(41.93%) patients required catherization. At T 7 blockade level 1/12 (8.33%) patients required catherization. At T8 level blockade no one required catherization. In our study there was no significant variation in post operative urinary retention in relation to height of sensory block level. Figure 1: Distribution of patients according to age group
Table 1: Voiding difficulty in patients after spinal anaesthesia
Table 2: Voiding difficulty in relation to sex
Table 3: Voiding difficulty in relation to co morbidity
Table 4: Voiding difficulty in relation to sensory block
DISCUSSION In our study we studied 100 patients undergoing spinal anaesthesia. Out of total 100 patients 59 patients underwent lower limb surgeries and 41 patients underwent lower abdomen surgeries. Mean age of the patients was 49.3± 3.1 years. Majority of the patients were from the age group of 50-60 years (32%) followed by 30-39 years (30%). Similarly, In a study undertaken by Hollma et al. 376 men undergoing hip arthroplasty were assessed for post operative urinary retention (defined in their study as inability to void after surgery for which single or indwelling catheter is required) it was demonstrated that that increasing age was an independent risk factor for POUR. 5 In our study, 80% of the patients were male and 20 % patients were female. Male to female ratio was 4:1. Table 1 shows voiding difficulty in patients after spinal anaesthesia. Majority of the patients had spontaneous Voiding without difficulty G0 (60%). Voiding with difficulty (G1) was observed in 17% patients. Intermittent single evacuation of bladder (G2) was seen in 7% patients. Intermittent repeated evacuation of bladder (G3) was observed in 8% patients. Continuous catherization was seen in 8% patients. Thus in our study incidence of post operative urinary retention was 40%. Table 2 shows Voiding difficulty in patients according to sex. Out of total 100 patients 80 were male and 20 were female. Among male majority 47(58.75%)were not having any difficulty in voiding urine. 14 patients had grade 1 voiding difficulty and 4 patients had grade 2 voiding difficulty. In females 65% females did not have any difficulty in voiding urine after spinal anaesthesia. Males show higher difficulty in voiding urine than females but the difference was not statistically significant (p>0.05). Similar to our study, higher incidence of post operative urinary retention has been reported in males as compared to women in previous studies.6-8 The difference thus found has already been found probably due to factors like Male urethra is longerand more tortuous than female urethra. There is also a presence of prostate in male which may enlarge in benign prostatic hypertrophy, thus obstructing to flow of urine.9,10 In our study, 75 patients were without any associated co morbidity. 10% patients had Diabetes milletus. Hypertension and respiratory diseases were seen in 7% and 6% patients respectively. One patient had both diabetes and hypertension. Table 3 shows voiding difficulty in relation to co morbidities. In patients with diabetes milletus 7/10 (70%) patients required catherization. In respiratory diseases 2/6(33.33%) patients required catherization. In hypertensive patients 6/7 (85.71%) patients required catherization. The patient with both DM and hypertension required catherization. Thus we can say that Diabetes milletus and hypertension are risk factors for development of post operative urinary retention. In a study conducted by Dreijer et al. (2011) demonstrated diabetes mellitus as independent risk factors for development of post operative urinary retention after spinal anaesthesia. 11 Also in another study conducted by Petros et al. (1991) they found that diabetes mellitus as independent risk factor for development of POUR. 9 Table 4 shows voiding difficulty in relation to sensory block. In our study, out 100 patients, majority of the patients had T6 blockade (53%) followed by T5 (31%). We found that maximum height of sensory level was T4 and minimum being T8 sensory level. T 7 blockade was observed in 12% patients. T4 and T8 level blockade was observed in 2% patients each. In T6 level blockade 8/53 (15.09%) patients required catherization. In T5 level blockade 13/31(41.93%) patients required catherization. At T 7 blockade level 1/12 (8.33%) patients required catherization. At T8 level blockade no one required catherization. In our study there was no significant variation in post operative urinary retention in relation to height of sensory block level. Detrusor muscle is completely relaxed after 2-5 minutes of spinal anaesthesia and its recovery depends on the duration of sensory block above the S2 and S3 sacral segments. Sensory block is regressed to S3 level after 7-8 hours post spinal anaesthesia. After the regression of sensory block to S3 level it further takes approximately 15 minutes for detrusor muscles functions to start, it may take 1-3 hours post sensory regression for normal function of detrusor to start (Axelsson et al.). 12 Thus it has been found in literature that detrusor activity normalises after S3 segment becomes free of effects of local anaesthetic agents. Thus theoretically higher the level of block, bladder function should take more time to normalise, but in studies it has been found that level of spinal blockade from short and intermediate acting drugs don’t have any effect on bladder dysfunction.13 Also in other study conducted by Keutziger et al. 2010 they found that level of blockade after spinal local anaesthetic agents is not an aggravating risk factor for post operative urinary retention.14
CONCLUSION No effect was seen on incidence of POUR with high level of sensory blockade.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home