Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 1 -July2017
Comparative study of dexmedetomidine and clonidine along with ropivacaine in epidural anaesthesia for vaginal hysterectomy
Jadhav Shashikant Abhimanyu1, Kore Rahul Dharma2*
1,2Assistant Professor, Department of Anaesthesiology, Dr. V. M. Government Medical College, Solapur, Maharashtra, INDIA. Email: rahuldkorefb@yahoo.com
Abstract Background: The present randomized double blind prospective study was carried out for Comparison of Dexmedetomidine and Clonidine along with Ropivacaine in epidural anaesthesia for vaginal hysterectomy. Methods: 60 female patients of ASA grade I and II, between the age group of 45 - 60 years were randomly assigned to 2 groups. Group RD: received 17 ml of 0.75% Ropivacaine Hcl and 1µg/kg of Dexmedetomidine Hcl, Group RC: received 17 ml of 0.75% Ropivacaine Hcl and 2µg/kg of Clonidine Hcl in supine position via epidural catheter. Onset, quality, duration of sensory and motor block and hemodynamic parameters evaluated. Results: Patients from Group RD have fast sensory block onset (i.e. 9.96±0.61min), prolonged two seg. regression time (138.93±4.48) and prolonged Analgesia time ((i.e 353.9±4.03min) as compared to Group RC i.e. (12.4±0.77), (128.8±3.46),(308.06±5.47) respectively. The duration of motor blockade was prolonged in patients of group RD (242.23±5.72min) as compared to the patients in group RC (230.66±5.20min). Patients in group RD were more sedated as compared to the patients in group RC. Initial fall in heart rate was more in patients of RD group as compared to the patients of group RC but later on both the groups showed stable heart rate. Fall in systolic, diastolic and mean arterial blood pressure was more in patients of RD group (during 5 to 50- 55 min of epidural injection) as compared to the patients of group RC. Later on both the groups showed stable systolic blood pressure. Conclusion: Dexmedetomidine is better adjuvant as compared to Clonidine for providing early onset and prolonged intraoperative as well as postoperative analgesia, better sedative property Both the drugs showed bradycardia and hypotension which was clinically insignificant. Key Words: Dexmedetomidine, Ropivacaine.
INTRODUCTION Alpha-2 agonists like Clonidine and Dexmedetomidine have been recently added to armamentarium of the anaesthesiologists as additives in regional blocks. Analgesic and anaesthetic drug requirements get reduced to a large extent by use of Clonidine and Dexmedetomidine as adjuvants because of their analgesic properties. The affinity of Dexmedetomidine towards alpha-2 adrenoreceptors is eight times more compared to Clonidine1 with ratio of (alpha-1: alpha-2) 1:1600.2,3,4 They also augment local anaesthetic effect leading to stable haemodynamics and decreased oxygen demand during surgery1. Ropivacaine, a new long-acting local anesthetic shows the differentiation between sensory and motor blocks. This differentiation is particularly useful when early mobilization is important to accelerate postoperative recovery. Addition of alpha-2 agonists to Ropivacaine improves the quality of epidural anaesthesia and postoperative analgesia2,5,6,7. There are very few clinical trials in India which compare the effects of addition of Dexmedetomidine/Clonidine with Ropivacaine in epidural anaesthesia1. So this prospective double blind randomized study was carried out to compare effect of Dexmedetomidine or Clonidine, as an adjuvant to Ropivacaine for epidural anaesthesia in patients undergoing vaginal hysterectomy.
MATERIAL AND METHODS The present randomized double blind prospective comparative study was carried out in 60 female patients of ASA grade I and II, between the age group of 45 - 60 years scheduled electively for vaginal hysterectomy at S.R.T.R Govt. Medical College, Ambajogai, Maharashtra. After approval from the institutional ethical committee we have selected 30 patients in each group for the study. The patients were randomly allocated into two groups i.e. RD and RC. Intravenous administration of Ringer’s lactate solution was started at the rate of 8ml/kg1. All monitors applied and basal readings noted. All patients were premedicated with IV inj. Ranitidine 1 mg/kg IV, inj, Ondansetron 0.08 mg/kg. Under all aseptic precautions, epidural catheter was inserted in L2-3 or L1-2 intervertebral space using 18 G Touhy needle and 5cm of the catheter length was kept in epidural space and after 3 - 5 minutes of administering test dose and confirming its correct placement, epidural administration of drugs was done in supine position as follows. Group RD: received 17 ml of 0.75% Ropivacaine HCL and 1µg/kg of Dexmedetomidine HCL Group RC: received 17 ml of 0.75% Ropivacaine HCL and 2µg/kg of Clonidine HCL All the data was recorded in proforma. Decoding of drugs was done at the end of study. The data was analysed statistically. In this study, for quantitative data of both the groups, mean and standard deviation were calculated. To find out the significant difference between two groups unpaired t- test was used and P value calculated with 95% confidence interval (P value <0.05) using Open Epi version 2.3.1. Paired t-test was used for intra group comparison. For qualitative data, Chi square test was used and difference was considered statistically significant if P value is <0.05.
Sensory block characteristics There is no such study which has compared the dose equivalence of Dexmedetomidine and Clonidine but the observations of various studies reveal that the dose of Clonidine is 1.5−2 times higher than Dexmedetomidine when used in epidural route1,9,15,16. So based on these studies we used 1µg/kg of Dexmedetomidine or 2µg/kg of Clonidine as adjuvant to Ropivacaine in epidural anaesthesia as also used by Saravana Babu MS et al.13 Demographic profile Table 1
P<0.05 is Significant (unpaired t-test), SD - Standard deviation, NS- Not Significant The demographic profile of our patients was comparable with respect to mean age, body weight and duration of surgery and was statistically insignificant.
Sensory block characteristics Table 2
s- Significant Reduction in time required to achieve maximum sensory dermatomal level in patients of group RD (20.9±0.8min) as compared to the patients in group RC (24.3±0.66min).The maximum sensory dermatomal level achieved and quality of sensory and motor block were same in both the groups. The time required for two segment regression of sensory dermatomal level was more in patients of group RD (138.93±4.48min) as compared to the patients in group RC (128.8±3.46min). Bajwa SJS et al1 observed that the onset time of sensory block in patients of group RD was 8.52 ± 2.36 minutes and it was 9.72 ± 3.44 minutes in patients of group RC. The time required to achieve maximum sensory dermatomal level in patients of group RD was 13.14 ± 3.96 minutes and it was15.80 ± 4.86 minutes in patients of group RC. They have used 1.5µg/kg of Dexmedetomidine which was more than the dose used by us (1µg/kg), so the time required for onset of sensory block and time required to achieve maximum sensory dermatomal level in patients of Bajwa’s study was earlier than observed in our study. Saravana Babu MS et al13 found that the time of onset of sensory block in patients of group RD was 7.33 ± 1.76 min and in patients of group RC was 8.40 ± 1.61min. The time required to achieve highest sensory dermatomal level in patients of group RD was 11.6 ± 2.05 min and in patients of group RC was 13.20 ± 2.90 min. The patients in group RD required less time to achieve maximum sensory block than patients of group RC. They have administered epidural analgesia for postoperative pain relief in patients undergoing spinal surgery under General anaesthesia. The residual effect of anaesthetic agents might be responsible for earlier onset and earlier maximum level achieved in their study as compared to our study. In our study, 26 patients in the group RD had highest dermatomal level of blockade at T6 and in group RC 23 patients achieved highest dermatomal level of blockade of T6, and the difference was statistically insignificant. None of the patient in either group showed inadequate level of sensory analgesia requiring supplementation of analgesic drugs. The present study is in accordance with observations of Bajwa SJS et al.1 They found that the maximum sensory dermatomal level achieved in all the patients of group RD was T5-6 and that of the in group RC was T6-7. The quality of sensory block assessed in patients of both groups showed grade-4 sensory block in 26 patients and grade-3 sensory block in 4 patients of group RD. While in group RC 23 patients showed sensory block of grade-4 and 7 patients showed sensory block of grade-3. The result of the our study can be explained on the basis of observation that addition of alpha-2 agonists to local anaesthetics potentiates their action by causing hyperpolarisation of nerve tissues3,4, giving good quality of analgesia. Bajwa SJS et al1 observed similar results in their study. Verma J et al12 observed that the addition of Clonidine to bupivacaine in epidural has improved the quality of sensory block with 54% of patient had sensory block of grade-3 and 35% of patient had sensory block of grade-4. Our observations are similar to above studies. Bajwa SJS et al1 observed that the time required for two segment regression of sensory dermatomal level in patients of group RD was 136.46 ± 8.12 min and it was 128.44 ± 27.18 min in patients of group RC. The difference in two was found to be statistically significant. Thus the patients in group RC had regression of sensory dermatomal level earlier than patients of group RD. Motor block characteristics Table 3
The duration of motor blockade was prolonged in patients of group RD (242.23±5.72min) as compared to the patients in group RC (230.66±5.20min). Bajwa SJS et al,1 Salgado PFS et al,10 Verma JH et al12 not studied the time for onset of motor block. Saravana Babu MS et al13 did not find any motor blockade in their study due to use of lesser concentration of Ropivacaine (0.2%). The present study showed that time required to achieve the complete motor blockade (modified Bromage scale grade-3) in patients of group RD was 20 ± 0.98 min and in patients of group RC was 26.6 ± 0.93 min. (Table no. 3) The difference between the two groups was statistically significant. Thus addition of Dexmedetomidine in Ropivacaine was associated with rapid onset of complete motor block. Bajwa SJS et al1 studied the effect of addition of Dexmedetomidine and Clonidine in epidural anaesthesia as an adjuvant to Ropivacaine and found that time required to achieve complete motor blockade in patients of group RD was 17.24 ± 5.16 min and in patients of group RC was 19.52 ± 4.06 min. The difference was found to be statistically significant. Thus our study is in concurrence with this study. Bajwa et al1 found complete motor block in all the patients when Clonidine or Dexmedetomidine was used. The use of higher dose of Dexmedetomidine (1.5µg/kg) may be responsible for complete blockade in all the patients. Salgado PFS et al10 observed that quality of motor block was more pronounced in the patients of Dexmedetomidine group with 32% of the patients had motor block of grade-3 and 68% of the patients had motor block of grade-2.Our study showed that time for regression of motor blockade in patients of group RD was 242.23 ± 5.72 min and in group RC was 230.66 ± 5.20 min. (table no.3).The difference was statistically significant. Thus Dexmedetomidine group was associated with prolonged motor blockade as compared to the Clonidine. Bajwa SJS et al1 studied the effect of addition of Dexmedetomidine and Clonidine in epidural anaesthesia as an adjuvant to Ropivacaine and found that time required for regression of motor blockade in patients of group RD was 246.72 ± 30.46 min and in patients of group RC was 228.44 ± 27.18 min. The difference was found to be statistically significant. Thus our study is in concurrence with this study.
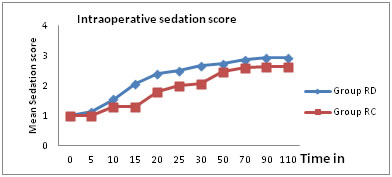
Changes in Mean sedation score in Intraoperative period
Figure 1
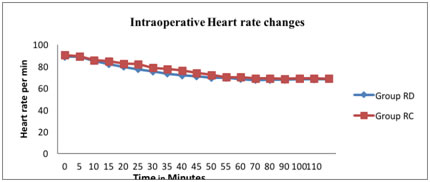
Patients in group RD were more sedated as compared to the patients in group RC. All patients in both the groups were responding to verbal or gentle tactile stimulation and all patients were wide awake after 6 hours of postoperative period. Bajwa SJS et al1 observed that mean sedation scores were significantly higher in RD group compared to RC group. Epidural Dexmedetomidine produced sedation in 36% of the patients, who were arousable by gentle tactile stimulation compared to achievement of similar sedation level in just 16% of the patients in Clonidine group. Overall, the sedation scores were highly significant statistically with administration of Dexmedetomidine. Saravana Babu MS et al13 and Verma J et al12 had similar observations. They observed light sedation (sedation score<3) in both the group RD and RC in almost equal proportion, but none of the patients had profound deep sedation (sedation score>3) in both groups. Preoperative respiratory rate and SPO2 in patients of both the groups were comparable and statistically insignificant. There was no change in respiratory rate and SPO2 in patients of both the groups inspite of sedation observed in both the groups. None of the patients in either group showed respiratory depression. (RR<10) or required oxygen supplementation. The results of our study are in accordance with the Bajwa SJS et al,1 Saravana Babu MS et al,13 Verma J et al,12 Bajwa SJS et al.11. No postop. neurological deficit observed in patients of either group in follow up period of 24 hours. Hemodynamic Parameters Initial fall in heart rate was more in patients of RD group (during 10 to 45 min of epidural injection) as compared to the patients of group RC (fig.2). Later on both the groups showed stable heart rate which remained on lower side as compared to their preoperative values till 6 hours of postoperative period. None of the patient in either group required treatment of bradycardia. The results of the present study are in concurrence with Bajwa SJS et al1 who observed decrease in heart rate in both groups but it never decreased more than 15% of the baseline values and none of the patient required treatment of bradycardia. Saravana Babu MS et al13 observed that heart rate started to decrease in both the groups as compared to their preoperative value from 30 min post epidural injection of drugs but none of the patient showed bradycardia (heart rate<60/min).
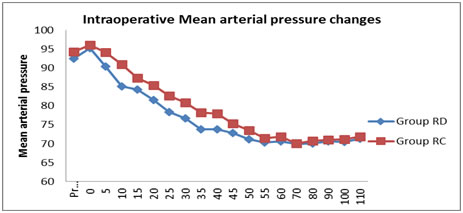
Figure 2 Fall in systolic, diastolic and mean arterial blood pressure was more in patients of RD group (during 5 to 50- 55 min of epidural injection) as compared to the patients of group RC (fig.3). Later on both the groups showed stable systolic blood pressure which remained on lower side as compared to their preoperative values up to 6 hours of postoperative period. None of the patients in either group required treatment of hypotension as the fall in Blood pressure was <30% of basal value.
Figure 3
Observations of our study are in accordance with Bajwa SJS et al1 observed decrease in mean arterial pressure in both groups but it never fell down to more than 15% of the baseline values and none of the patient required treatment of hypotension. Saravana Babu MS et al13 observed that mean arterial pressure started to decrease in both the groups as compared to their preoperative value from 30 min post epidural injection of drugs but none of the patient required treatment of hypotension. Verma J et al12 observed Significant decrease in the systolic blood pressure at 15min. However, clinically significant hypotension was not noticed in either group. At 15 min no significant difference was noticed in diastolic blood pressure between the two groups. Highly significant decrease in the diastolic blood pressure was observed at 30 min and significant decrease in diastolic blood pressure was seen from 45 min until 2 hrs in between the two groups. Bajwa SJS et al11 observed decrease in mean arterial pressure in both groups and none of the patient required treatment of hypotension. None of the patient in either group showed respiratory depression or desaturation requiring supplementation of oxygen, nausea, vomiting, pruritus, dry mouth.
Time of first analgesic administration and VAS score Table 4
The time for administration of first analgesic in patients of group RD was 353.9 ± 4.03 minutes while in group RC was 308.06 ± 5.47 minutes (table no.5). The difference was statistically significant. Duration of analgesia was Table 5
Saravana Babu MS et al13 observed that mean VAS scores were higher in RC group in comparison to RD group at different time intervals, although statistically insignificant. Duration of analgesia in patients of group RD was 407 ± 47.06 minutes and in patients of group RC was 345 ±35.02 minutes. The difference between two was found to be statistically significant. There were no postoperative complications like nausea, vomiting, respiratory depression (RR<10), hypotension, bradycardia, tachycardia, pruritus, dry mouth, drowsiness found in both the groups in recovery room.
CONCLUSION We concluded that Dexmedetomidine and Clonidine both are safe and effective adjuvants to epidural Ropivacaine. Dexmedetomidine is better adjuvant as compared to Clonidine for providing early onset and prolonged intraoperative as well as postoperative analgesia, better sedative property Both the drugs showed bradycardia and hypotension which was clinically insignificant.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home