Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 1 -July2017
Comparison of levobupivacaine and clonidine with plain levobupivacaine in spinal anaesthesia in lower limb surgeries
Sudeep1, N Gopal Reddy2*
1Associate Professor, 2Professor, Department of Anaesthesiology, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda, Telangana
Abstract Background: Intrathecal Levobupivacaine is having similar clinical profile with less cardio-toxicity than Bupivacaine is used commonly in lower limb surgeries. Clonidine as an additive to LA provides effective prolongation and dose dependent analgesia. Aim: To compare effect of intrathecal 0.5% Levobupivacaine heavy 10 mg with Clonidine 30 µg with 0.5% levobupivacaine 10mg for lower limb surgeries. Material and Method: In this study we compared onset, degree, maximum sensory level achieved, time required to achieve the maximum level of sensory blockade, duration of effective sensory blockade and onset and degree of effective motor blockade and post-operative analgesia. Results: The onset of Analgesia and motor block started at 2.25±0.19 and 8.51± 0.18 minutes in group I and slightly delayed 2.48±0.18 and 9.33±0.14 minutes in control group mean duration of two segment regression in clonidine group was 210.51±6.99 minutes and in control group was 124.83±5.098 minutes, duration of motor blockade in clonidine group is 220.17±9.68 minutes and in control group is 155.34±6.262 minutes. The mean duration of analgesia in clonidine group is 650.17±9.26 minutes and in control group is 230.86±26.22 minute. The prolongation in duration of analgesia in clonidine group was statistically more significant (p<0.05). Conclusion: We observed that that isobaric Levobupivacaine with Clonidine has got comparable pharmacokinetic in onset of sensory and motor block, good intraoperative and postoperative prolonged analgesia. Key Words: Levobupivacaine, Clonidine, Lower-limb surgeries.
INTRODUCTION Central neuraxial blockade is the most popular technique of anaesthesia for lower limb surgeries. It is having several advantages like easy technique, economic and provides good quality of anesthesia. It decreases blood loss, avoid risk of intubation and aspiration, provides early ambulation. Bupivacaine is most commonly used local anaesthetic drug for spinal anaesthesia but cardio-toxicity is the limiting factor. Levobupivacaine is having similar clinical profile with less cardio-toxicity than Bupivacaine is gaining popularity.1,2 It has demonstrated less affinity and strength of inhibitory effect on the inactivated state of cardiac sodium channels than the Bupivacaine and faster protein binding rate.2. To provide good quality of intra-operative anesthesia with post-operative analgesia different additives like Opioids, Ketamine, Midazolam, Neostigmine and α 2 adrenergic agonist are used.3 Opioids may cause pruritus, nausea, vomiting, urinary retention and respiratory depression. Midazolam causes neurotoxicity4. Clonidine is a selective partial α- 2 adrenergic agonist provides effective, prolonged and dose dependent analgesia with a consequently decreased requirement of supplemental analgesics.5
MATERIAL AND METHOD After approval from hospital ethics committee, detail clinical examination, investigations and written informed valid consent, ASA grade I and II, both male and female patients were posted for lower limb surgery. This study was conducted in patients undergoing lower limb surgeries to evaluate and compare the effect of Clonidine 30 µg as an adjuvant to intrathecal 0.5% isobaric Levobupivacaine 10 mg as group-1 and 0.5% levobupivacaine10 mg without additives as group-2. Our primary aim was to compare onset, degree, maximum level achieved, time required to achieve the maximum level of sensory blockade, duration of effective sensory blockade and onset and degree of effective motor blockade after intrathecal Clonidine 30 µg as an adjuvant to intrathecal 0.5% isobaric Levobupivacaine 10 mg and levobupivacaine without clonidine. Our secondary aim was to compare effect of Clonidine 30 µg as an adjuvant to intrathecal 0.5% isobaric Levobupivacaine 10 mg and only 0.5% hyperbaric levo bupivacaine 10 mg. on vital parameters like pulse rate, mean arterial pressure, SpO2 respiratory rate, intraoperative side effects like nausea, vomiting, bradycardia, hypotension, sedation, respiratory depression, dry mouth, and time required for request of first rescue analgesic.
OBSERVATIONS AND RESULTS This prospective study was carried out on sixty patients of ASA grade I - grade II, undergoing lower limb surgeries under spinal anaesthesia. There was no statistical significant difference among both the groups as far as age, height and weight.
Table 1: Comparison of age, weight and height (mean±sd) in both groups (N=60)
Table 2: Comparison of time of onset and duration of sensory and motor effects (mean± sd) in both groups (n=60)
p-value <0.05 is taken as significant. Onset of sensory and motor effects are faster in group 1 (clonidine group) as well as duration of blocks when compared to group-2.
Table 3: Comparison of occurrence of post operative complications in both groups (n=60)
Post operative nausea, sedation and dry mouth are more in group 1 (clonidine group).
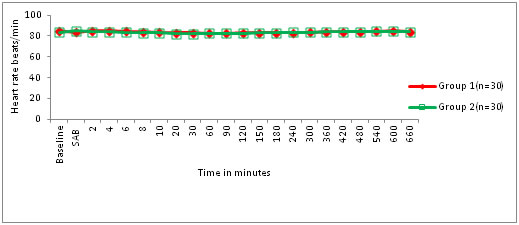
Figure 1: Comparison of heart rates in both groups (n=60) Mean heart rates are comparable between both the groups.
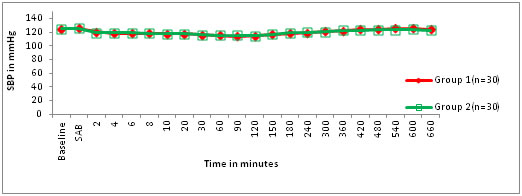
Figure 2: Comparison of systolic blood pressures in both groups (n=60)
Results are comparable between the groups.
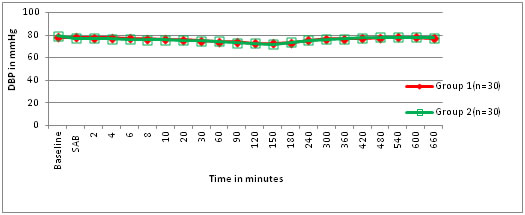
Mean diastolic blood pressures are comparable between both the groups. The mean time for the onset of sensory blockade in patients in group -1 was 2.25±0.19 min and in group -2 was 2.48 ± 0.18 min with p=0.00013. It indicates that the difference was statistically significant. Mean time required for maximum motor blockade was8.51 ± 0.8 min for group -1 and 9.33 ± 0.14 min for group -2 with P=0.00001. The difference between both the groups was statistically significant. None of the patients from both the groups required general anaesthesia. The difference between the two groups was statistically significant. We observed that after 15 minutes of block 4 patients in group -1 and zero patients in group-2 were mildly sedated after 15 minutes while after 45minutes 6 patients in group -1 and nil patients in group -2 were moderately sedated.1 patient from group -1was difficult to arouse. None had respiratory rate less than12 and SPO2 less than 95%. The difference between the two groups was statistically not significant. Bradycardia was statistically significant in patients of group -1 as compared to that in group-2.Basal mean arterial pressure was comparable in both the groups (p>0.05). Hypotension was statistically significant in group-1 compared to group -2. The difference between the two groups was statistically not significant. Mean basal respiratory rate was 14.53 ± 1.36 per min in group-1B and 14.93 ± 1.04 per min in group-2. The difference between the two groups was statistically not significant. Mean minimal respiratory rate was 12.10 ± 1.12 per min in group -1 and 13.47 ± 1.4 per min in group -2. The difference between the two groups was statistically significant. Two dermatome regressions in group -1 was at 210.51 ± 6.99 min and in group-2 it was at 124.83 ± 5.09 min. The difference between the two groups was statistically not significant. The first rescue analgesic required in group-1 was at 650.17 ± 9.22 min and in group -2 was at 230.86 ±26.22 min. The difference between the two groups was statistically significant. Incidence of nausea and vomiting were same in the groups. Patient had dry mouth more in group-1, sedation nil in group-2 and they are comparable. V.
DISCUSSION Spinal anesthesia is most preferred technique of anesthesia for lower limb surgeries Levobupivacaine is said to be less cardio-toxic and having more specific effects on sensory rather than motor nerve with shorter duration of analgesia and motor blockade.6,7,8 Misirliogulu et al and Feroz et al noted that there was no significant difference in the quality of anesthesia and intraoperative side effects but time to complete regression of motor blockade was statistically lower in group levobupivacaine.8,9 Clonidine blocks the conduction of C and A δ fibers and acts synergistically with local anaesthetics by its action of opening potassium channels.10 Intrathecal clonidine prolongs sensory as well as motor block of spinal anesthesia by activation of post synaptic α-2 receptor in substantia geletinosa of spinal cord.11 It decreases local anesthetic requirements and provides prolonged postoperative analgesia. Also it acts as antiemetic, anxiolytic, reduces post spinal shivering and provides sedation without respiratory depression.11 This decreased dose of LA Reduction in spinal anaesthesia can decrease incidence of hypotension, high spinal block, and prolonged motor block. Due to good postoperative analgesia after surgery with intrathecal Clonidine, the pt has better pain control. This indicates that Levobupivacaine with clonidine a better agent.12,13 We noted that onset of motor blockade was comparable in both the groups. Same findings were noted in previous studies by A.Mehta13 et al and Feroj Dar9 et al while Gulen Guler12 et al differed. In our study sedation was significant in the group-1. Sedation with Clonidine is due to central action produced due to hyper-polarization of excitatory neurons localized in the nucleus coereleus.14 Respiratory rate and SpO2 was well maintained. None of the patients in both the groups required treatment. Our findings are similar with that of Bajwa2 et al observed earlier requirement of rescue analgesic plain levobupivacaine and an additive indicates that Clonidine as an adjuvant provides prolonged postoperative analgesia than other additives. From all our observation we can conclude that intrathecal isobaric Levobupivacaine with Clonidine is better alternative to plain levobupivacaine for lower limb surgeries as it provides good quality of sensory and motor blockade, better cardiac stability without sedation.
CONCLUSION We observed that that isobaric Levobupivacaine has got better pharmacokinetic in onset and offset of sensory and motor block, less cardiovascular side effects and comparable postoperative analgesia to plain levobupivacaine. So we conclude that Levobupivacaine with Clonidine is a better choice in lower limb surgeries without Clonidine.
REFERENCES
|
|
 Home
Home