Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 2 -August 2017
Comparative study of 0.5% lignocaine with dexmedetomidine and 0.5% lignocaine in intravenous regional anesthesia
Suhas Jewlikar1, Ashwini Suryawanshi2*
1Associate Professor and HOD, Department of Anaesthesia Government Medical College Aurangabad, Maharashtra, INDIA. 2Fellow Department of Anaesthesia, Fortis Hospital, Mulund, Maharashtra, INDIA. Email: drsuryawanshiashwini@gmail.com, jewalikar@yahoo.co.in Abstract Background: Intravenous regional anaesthesia (IVRA) is a simple and reliable technique, with success rates between 94% to 98%. The local anaesthetic most often used is lignocaine. dexmedetomidine, a potent -2 adrenoceptor agonist is approximately 8 times more selective than clonidine4. Administration of dexmedetomidine as an adjuvant to local anaesthetic has many advantages. In this study we compared lignocaine with lignocaine and dexmedetomidine in IVRA for elective hand and forearm surgeries. Aims and Objectives: To compare onset, quality and duration of sensory and motor block, tourniquet pain, postoperative analgesia, complications and hemodynamic stability after using Dexmedetomidine as an adjuvant. Materials and Methods: 60 Patients undergoing elective hand and forearm surgeries were randomly assigned to Group L (0.5% Lignocaine 200 mg) and Group LD (0.5% Lignocaine 200 mg and 0.5 ug/kg of Dexmedetomidine). Results: Demographic data were comparable. Conclusion: Addition of Dexmedetomidine to lignocaine provides IVRA with quicker onset of sensory and motor block, better quality of anaesthesia, prolonged duration of sensory, motor blockade and postoperative analgesia, delays the onset and severity of tourniquet pain, better hemodynamic stability without any adverse effects. Key Words: IVRA, Dexmedetomidine, lignocaine. Hand and forearm Surgeries.
INTRODUCTION Intravenous regional anesthesia (IVRA) is a simple and reliable technique hence popular, with success rates between 94% to 98%1,2. It is commonly used for forearm surgeries lasting for <90 minutes3. IVRA was originally introduced by the German surgeon August K. G. Bier in 1908; thus the name “Bier’s block”. He described a complete anesthesia and motor paralysis after intravenous injection Prilocaine into a previously exsanguinated limb. IVRA offers advantages like ease of administration, rapid onset and recovery, adequate muscular relaxation and controlled extent of anesthesia with3 good analgesia and bloodless operative field. It is cost effective requiring inexpensive equipments therefore used in day care surgeries. It has disadvantages like tourniquet pain, poor post-operative analgesia, limited time of surgical anesthesia (<90 minutes), difficulty in providing a bloodless field if exsanguination is improper, nerve damage, risk of local anesthetic toxicity if tourniquet is accidentally deflated. Rare complications include development of compartment syndrome and loss of limb3. Various adjuvants have been used to overcome the disadvantages. Recently, -2 adrenergic receptor agonists have been the focus of interest for their sedative, analgesic and perioperative sympatholytic and cardiovascular stabilizing effect with reduced anesthetic requirements. dexmedetomidine, is a potent -2 adrenoceptor agonist approximately 8 times more selective than clonidine4. A comparative study was carried out in our institute using IVRA with Lignocaine and Dexmedetomidine as an adjuvant.
MATERIAL and METHODS Study Design: Prospective, randomized, comparative study. Sample Size: Two groups with 30 subjects in each group. Group L: 30 patients with 200mg of 0.5% Lignocaine diluted with normal saline to a total volume of 41 ml. Group LD: 30 patients with 200mg of 0.5% Lignocaine and 0.5µg/kg Dexmedetomidine diluted with normal saline to a total volume of 41 ml. After approval from the hospital ethical committee, informed consent was taken from patients. Inclusion Criteria patients with ASA grade I and II, age - 15 to 50 years, weight - 40 to 60 kg, undergoing elective hand and forearm surgeries. Exclusion Criteria Patients refusal, history of hypersensitivity to local anesthetics, history of sickle cell disease, peripheral vascular disease5, cardiovascular disease, patients on –blocker therapy, systemic disease like liver and kidney, local infection, skeletal muscle disorders, hypertension, convulsions and pregnant patients6,7,8. A detailed history and systemic examination with routine investigations like hemogram and urine examination was done in all patients. The procedure and use of the visual analogue scale was explained to patients preoperatively. All equipment and drugs necessary for resuscitation and general anesthesia were kept ready. Cardiac monitor, noninvasive blood pressure, and pulse oximeter were used for monitoring. Baseline pulse rate, systolic and diastolic blood pressure, mean arterial pressure (MAP), respiratory rate, SpO2 were noted. We used a “double cuff” tourniquet to increase the reliability of the technique. Intravenous catheter of 20G in the nonoperative hand and 22G in the dorsum of hand of the arm to be anesthetized was introduced. The arm was elevated for 5 minutes to exsanguinate. A pneumatic tourniquet was placed around the upper arm, and the proximal cuff was inflated to 100 mm Hg above systolic blood pressure9. Circulatory isolation of arm was verified by inspection, absence of radial pulse, loss of pulse oximetry reading in ipsilateral index finger. GROUP L received 0.5% Inj. Lignocaine 200mg diluted with normal saline up to 41 ml and GROUP LD received 0.5% Inj. Lignocaine 200mg + Inj. Dexmedetomidine 0.5 ug/kg diluted with normal saline up to 41 ml. The solution was injected at rate of 0.5 ml/sec10 in the hand to be operated with constant monitoring of pulse rate, blood pressure, respiratory rate, SpO2 and signs and symptoms of local anesthetic toxicity, after inflation of proximal tourniquet. Sensory block was assessed by pinprick with 22 G short beveled needle every 30 seconds. Patients’ responses were evaluated in the dermatomal sensory distribution of medial and lateral brachial cutaneous, ulnar (little finger, hypothenar eminence), median (thenar eminence, index finger) and radial (forearm and first web space) nerves11. Sensory block was graded as 4 – Excellent, no pain; 3 – Minor pain, with no need of supplemental analgesics; 2 – Moderate pain, needed supplemental analgesics (Inj. Diclofenac1.5mg/kg IV); 1 – Severe pain, (General anesthesia needed). Patients who required general anesthesia were excluded. Recovery of sensory block was defined as the time elapsed from tourniquet deflation to recovery of sensations in all dermatomes, as determined by pinprick test. Motor function was assessed by asking the patient to flex and extend his fingers, wrist and elbow6. Onset of motor block was defined as the time elapsed from injection of drug to complete motor block up to 15 minutes12. Motor block was graded as Grade 4 – No movement; Grade 3 – Movement only at interphalangeal joint; Grade 2 – Movement at interphalangeal and wrist joint; Grade 1 – Movement at interphalangeal, wrist and elbow joint. Recovery of motor block was defined as the time elapsed from the tourniquet deflation to the movement of fingers, hand and forearm comparable to opposite arm. After sensory and motor blockade, the distal tourniquet was inflated to 100mm Hg above systolic blood pressure, the proximal tourniquet was deflated and surgery was started. MAP, HR, SpO2 were monitored immediately after distal tourniquet inflation and 5, 10, 15, 20, 30, 40, 50…..…90min after injection of anesthetic and post-operatively after release of tourniquet till complete recovery of sensory and motor block. During the procedure, patient was continuously watched for signs and symptoms of local anesthetic toxicity and tourniquet pressure on pressure gauge. Assessment of tourniquet pain was made by visual analogue scale (0 – no pain and 10 – worst pain imaginable) measured before and after tourniquet application and 5, 10, 15, 20, 30, 40 and 50…….90 min after study drug application. Inj. Fentanyl 1 ug/kg was given if VAS for tourniquet pain is more than 4. The tourniquet was not deflated before 25 minutes3 and not kept inflated for more than 90 minutes. At the end of the surgery, the distal tourniquet was deflated by cyclic deflation-inflation technique. Distal tourniquet was deflated for initially 1 min, then reinflated for 1 min, and again deflated and then removed 9. After tourniquet deflation, patients were continuously monitored for arrhythmias and blood pressure changes and CNS side effects like dizziness, tinnitus, lightheadedness or presence of metallic taste. The surgeon who was blinded to the assignment was asked to qualify the operating conditions and dryness of the operative field. Patient’s acceptance was evaluated as good, satisfactory and unsatisfactory. Post-operative analgesia was assessed every 15 minutes as per VAS in the first hour and later every one hour till score was 4 or more. When VAS > 4,IV Inj. Tramadol 1 mg/kg was given. Time elapsed from tourniquet release to administration of first analgesic was considered as ‘duration of post-operative analgesia’. Patients were followed up to 24 hours post-operatively for occurrence of local effects like edema, skin rash, hematoma and neurological injury and are treated as needed. Data analysis is done with the help of SPSS Software ver 15 and Sigma Plot Ver 12. Quantitative data is presented with the help of Mean and Standard Deviation. Comparison done with Unpaired T test or Mann-Whitney test. Qualitative data is presented with Frequency and Percentage tables, association is assessed with the help of Chi-Square test. P value less than 0.05 is taken as significant level.
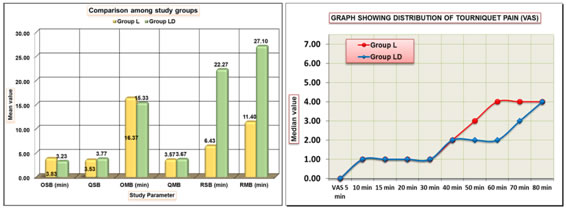
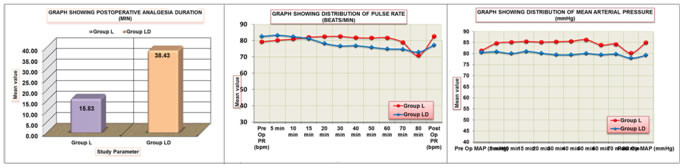
RESULTS Both the groups were comparable as far as age, sex, weight, ASA status, duration and type of surgery. The mean time of onset of sensory block in group L was (3.83 ± 1.88) minutes and in group LD was (3.23 ± 1.85) minutes, (P<0.05). The mean time of onset of motor block was (16.37 ± 2.92) in group L and (15.33 ± 2.25) in group LD (P<0.05). Quality of sensory block (3.57 ± 0.51) in group L and (3.77 ± 0.43) in group LD, (P<0.05). Quality of motor block was (3.57 ± 0.50) and (3.67 ± 0.55) for group L and LD respectively, (P<0.05). The mean time of recovery from sensory block was (6.43 ± 5.54) minutes in group L and (22.27 ± 6.66) minutes in group LD, (P < 0.05). The mean time of recovery from motor block was (11.40 ± 6.41) minutes in group L and (27.10 ± 6.79) minutes in group LD, (P<0.05). The side effects were observed immediately after the release of tourniquet for 2-3 minutes in lidocaine group only. In group L, 2 patients had lightheadedness (6.7%), 1had tinnitus (3.3%), total incidence was 10% and none required any treatment. None of patients in LD group had experienced any side effects. (P>0.05). Pulse rate in Group LD was on lower side than Group L, throughout after 15 mins. But there was no evidence of bradycardia, (P>0.05). In group LD, MAP was on lower side but no evidence of hypotension (P<0.05). Group LD showed better hemodynamic stability. There was statistically significant lower VAS for tourniquet pain in group LD (2.37 ± 1.10) than in group L (4.97 ± 1.13), (P<0.05). 19 patients in group L and 2 patients in group LD required intraoperative supplementation with inj. Fentanyl 1 ug/kg IV. All patients accepted the technique well. The quality of operative field judged by surgeon was better in LD group compared to group L. Post-operative analgesia was assessed every 15 minutes as per VAS in the first hour and later every one hour till score was 4 or more. The mean postoperative analgesia duration was (15.83 ± 7.67) minutes in group L and (38.43 ± 13.85) minutes in group LD, (P < 0.05). Table 1:
Figure 1 Figure 2 Figure 3 Figure 4 Figure 5
DISCUSSION Among various adjuvants, -2 adrenergic receptor agonists have better sedative, analgesic and perioperative sympatholytic and cardiovascular stabilizing effect with reduced anesthetic requirements. DEXMEDETOMIDINE,a potent -2 adrenoceptor agonist is approximately 8 times more selective than clonidine4. Although there is strong evidence that stimulation of α-2 receptors leads to the production of analgesia at the spinal cord level, the analgesic effects of dexmedetomidine in the clinical settings have been investigated primarily in regard to opioid sparing action¹3. It is effective premedication before IVRA because it reduces patient anxiety, sympathoadrenal responses and opioid analgesic requirements but it does not reduce tourniquet pain¹4. α-2 adrenergic receptors located at nerve endings may have a role in the analgesic effect of the drug by preventing norepinephrine release15. However, Dexmedetomidine may cause hemodynamic side effects such as hypotension and bradycardia13,16.Considering the above advantages of dexmedetomidine we compared it with plain Lignocaine having rapid onset of anesthesia, good muscle relaxation and prompt recovery M. R. Fahim et al (2005)17 carried out a study to evaluate the effect of sufentanil 25 ug, tramadol 100 mg, or dexmedetomidine 0.5 ug/kg added to lignocaine for IVRA. Dexmedetomidine was found to be more effective in regarding onset of sensory block time, complete motor block recovery time, duration of post-operative analgesia, amount of post-operative rescue analgesic requirements and the post-operative side effects. Dilek Memis et al (2004)4 carried out a study to evaluate the effect of Dexmedetomidine when added to lidocaine in IVRA. They found shorter onset and delayed recovery of sensory and motor block. There was no statistical difference between groups when compared for MAP, HR, and SPO2. The addition of Dexmedetomidine in IVRA delayed the onset of tourniquet pain and decreased analgesic requirement for tourniquet pain relief when compared with the lidocaine group (P < 0.001). Alok Kumar et al (2012)18 compared the effect of ketamine and Dexmedetomidine as an adjuvant to lignocaine in IVRA. They found better quality of anesthesia and perioperative analgesia with Dexmedetomidine without any side effects. Dexmedetomidine potentiates the effects of all anesthetic agents irrespective of mode of administration (intravenous, inhalational, regional block). Intraoperative administration of dexmedetomidine in lower concentration has reduced requirement of other anesthetic agents; fewer interventions to treat tachycardia and a reduction in the incidence of myocardial ischemia¹⁹. These properties of dexmedetomidine may be responsible for faster onset and prolonged duration of sensory and motor block and better tourniquet pain tolerance. Thus, addition of 0.5 ug/kg of Dexmedetomidine to 200 mg of 0.5 % lignocaine provides IVRA with quicker onset of sensory and motor block, better quality of anesthesia, prolonged duration of sensory, motor blockade and postoperative analgesia with better tourniquet tolerance. Success of intravenous regional anaesthesia needs exsanguination of limb at least for 5 min, use of double bladder cuff tourniquet and tourniquet deflation by intermittent cyclic deflation re-inflation technique. Maximum allowable tourniquet time for upper limb is 90 minutes. Inflation of tourniquet beyond this period results in complications like tourniquet pain, nerve injury, post- operative oedema, pressure sores and thrombosis. General anesthesia was not required for any patient. So, the success rate of our study was 100%.
CONCLUSION From the data and statistical analysis it can be concluded that, 0.5 ug/kg of inj. Dexmedetomidine can be safely used as an adjuvant to 200 mg of 0.5% lignocaine for IVRA which provides quicker onset of sensory and motor block, better quality of anesthesia, prolonged duration of sensory, motor blockade and postoperative analgesia. Dexmedetomidine also delays the onset and severity of tourniquet pain along with better hemodynamic stability and without any adverse side effects.
REFERENCES
|
|
 Home
Home