Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 2 -August 2017
A double blind, randomized, controlled trial to study the effect of dexmedetomidine on hemodynamic and recovery responses during tracheal extubation
Chintala Kishan1, Gopal Reddy Narra2*
1Assistant Professor, 2Professor, AIMS, Mohinabad, Rangareddy, Telangana, INDIA. Email: drgopalreddynarra@yahoo.com
Abstract Background: Extubation is known to produce significant hemodynamic disturbances. Literature claims that dexmedetomidine, provides excellent cardiovascular stability, no respiratory depression and may be a useful adjunct to facilitate smooth tracheal extubation. Aim: To study the effect of Dexmedetomidine on haemodynamics and recovery response during tracheal extubation. Materials and Methods: sixty persons of American Society of Anesthesiologists grade I‑II, aged 20‑45 years, scheduled for elective general surgery and Obstetrics and Gynecology were studied after randomization into two groups. Group D and C received an intravenous infusion of dexmedetomidine 0.5 µg/kg or placebo respectively, over 10 minutes before anticipated time of end of surgery, in a double blind manner. Anesthesia techniques were standardized. Vitals were recorded while starting of the injection, before extubation and at 3 and 10 minutes after extubation. Quality of extubation was evaluated on a 5 point scale and postoperative sedation on a 6 point scale. Adverse events were recorded. Results: Heart rate, systolic, diastolic, mean arterial pressures were significantly higher in group C (P <0.05). Extubation quality score of majority of patients was 2 in group D and 3 in group C. Sedation score of most patients was 3 in group D and 2 in group C. Bradycardia and hypotension incidences were higher in group D. Hypertension, tachycardia and agitations were more in control group. One patient in group D, two patients in group C had vomiting. Complications were also more in control group. Conclusion: Dexmedetomidine 0.5 µg/kg administered 10 minutes before extubation, stabilizes hemodynamics and facilitates smooth extubation. Key Words: General anaesthesia, α2‑adrenoreceptor agonist, dexmedetomidine, extubation quality, hemodynamic responses.
INTRODUCTION Tracheal extubation is the discontinuation of an artificial airway when the indications for its placement are no longer required. For a smooth extubation, there should be no straining, coughing, breath holding or laryngospasm. Extubation at light levels of anesthesia can stimulate reflex responses via tracheal and laryngeal irritation. Various agents like lidocaine, opioids, esmolol, and calcium channel blockers,1,2 magnesium sulphate and propofol have been shown to attenuate these responses, but they all have limitations and side effects. Dexmedetomidine, an α2‑adrenoreceptor agonist with a distribution half‑life of approximately 6 minutes has been successfully used for attenuating the stress response to laryngoscopy.3,4
MATERIALS AND METHODS This study was carried out on 60 patients (30 in each group) between 20 to 45 years of age of either sex belonging to American Society of Anesthesiologists (ASA) physical status I and II and scheduled for elective general surgical surgeries and Obstetrics and Gynecology. Patients with cardiovascular or respiratory disorders, diabetes, hypertension, obesity, difficult airway, on medications that effect heart rate (HR) or blood pressure (BP), pregnant, currently breast feeding women, history of sleep apnea and those for emergency procedures were excluded. Institutional Atheics committee approval was taken and written informed consent was taken from all patients. Pre-anesthetic check up was conducted and a detailed history and complete physical examination recorded. Routine investigations like complete blood picture, blood grouping/typing, blood urea and serum creatinine were done. Using computer generated random allocation; patients were divided into two groups (30 patients in each group). The enrolling investigator prepared the drug solution to be given before extubation and had no role in patient’s assessment. Routine anesthetic technique was used using propofol, fentanyl, vecuronium, nitrous oxide-oxygen and Isoflurane. Standard monitoring with electrocardiography (ECG), pulse oximetry (SpO2) and noninvasive BP was done. About 10 minutes before the estimated time of end of surgery, inhalation agent was cut off and patients in each group received the specified solution intravenously over 10 minutes. Patients in group D received dexmedetomidine 0.50 µg/kg intravenous (IV) in 10 ml normal saline (NS) over 10 minutes while in group C, patients received 10 ml NS over 10 minutes. HR, systolic BP and diastolic BP were recorded at the start of bolus drug injection and thereafter before extubation and 3 and 10 minutes after extubation. Residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg IV. When patients’ spontaneous respirations were considered sufficient and patients were able to obey simple commands, suction of throat was done and trachea was extubated. The anesthesiologist performing the extubation was blinded to the study drugs. HR, systolic BP and diastolic BP were recorded before the time of extubation and thereafter at 3 and 10 minutes after extubation. Occurrence of any event like laryngospasm, bronchospasm, desaturation, respiratory depression, vomiting, hypotension, bradycardia or undue sedation was noted. Hypotension was defined as a decrease in systolic BP of more than 20 mmHg from baseline and was corrected with IV fluids and if required, with small dose of mephentermine 5 mg IV. Bradycardia was defined as a HR of less than 60/minute and was corrected, if associated with hemodynamic instability, with atropine 0.6 mg IV. Quality of extubation was evaluated based on cough immediately after extubation, using a 5 point rating scale(Extubation Quality Score):6 1 = no coughing, 2 = smooth extubation, minimal coughing (1 or 2 times), 3 = moderate coughing (3 or 4 times), 4 = severe coughing (5-10 times) and straining, 5 = poor extubation, very uncomfortable (laryngospasm and coughing >10 times). Postoperative sedation was evaluated on a 6 point scale (Ramsay Scale):7 1 = Anxious or agitated and restless or both, 2 = Cooperative, oriented and tranquil, 3 = Drowsy but responds to commands, 4 = Asleep, brisk response to light glabellar tap or loud auditory stimulus, 5 = Asleep, sluggish response to light glabellar tap or loud auditory stimulus, 6 = Asleep and unarousable. Statistical Analysis The parameters were recorded and data was entered into Statistical Package for Social Sciences (SPSS 15.0). Statistical analysis was done using paired-samples t-test for between-group comparisons. The χ2 test or the Fisher exact test was used to analyze extubation quality, sedation scores, and adverse events. P value 0.05. We observed a statistically significant difference (P<0.05). Table 1: Comparison of demographics and other parameters between the groups
#Results of both the groups were comparable with respect to age, sex, body weight and duration of surgery (Table-1) and are statistically not significant.
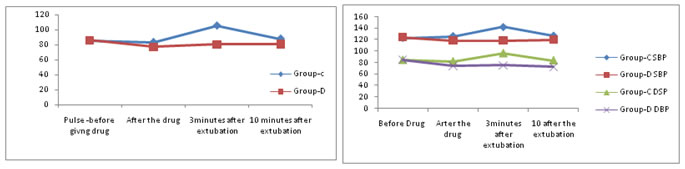
Basal heart rate (HR) was comparable in both the groups. In group D, HR was lower to basal value from 5th minute of the start of drug infusion and at extubation, however it was lower than basal value post extubation till 10 minutes whereas HR in group C showed a rise at and after the extubation when compared to preoperative values which was significant (P 0.05). Table 2: Vitals before and after the extubation at given timings
# Vitals are statistically significant after the drug infusion and post extubation periods.
Table 3: Smooth extubation parameters; Extubation quality score and Ramsay scale in number of persons in each group.
# Extubation quality score of majority of patients was 2 in group D and 3 in group C. Sedation score of most patients was 3 in group D and 2 in group C.
Table 4: Comparison of incidence of complications in the two groups Complications
#Post operative complications are more in control group when compared to group-D. DISCUSSION Currently, dexmedetomidine is indicated for intensive care unit sedation in mechanically ventilated patients and for sedation of non intubated patients before or during surgical and other procedures.5 We hypothesized that dexmedetomidine might be a useful agent to attenuate the response to extubation as it provides sedation, hemodynamic stability and does not depress respiration. easy extubation, provide a more comfortable recovery and allow early neurological examination following intracranial operations.8 Dexmedetomidine 0.5 µg/kg, given 10 minutes before extubation has been found to be more effective than fentanyl 1 µg/kg in attenuating airway reflex responses to tracheal extubation and maintaining hemodynamic stability without prolonging recovery.9 In patients undergoing vascular surgery, dexmedetomidine (plasma concentrations in the range of 0.18 to 0.35 ng/ml) attenuated the increase in HR and plasma norepinephrine concentrations during emergence from anesthesia and did not attenuate postoperative increases in HR or BP after emergence from anesthesia or affect intraoperative anesthetic or postoperative analgesic requirements.10 An infusion of dexmedetomidine started 20 minutes before anesthesia and continued until the start of skin closure in patients undergoing supratentorial brain tumor surgery was found to blunt tachycardia response to intubation and the hypertensive response to extubation.11 In vitro studies indicate that α2 stimulation can cause smooth muscle relaxation thereby preventing bronchoconstriction. In our study, most patients in the study group-D could be extubated smoothly with minimal coughing (Extubation Quality Score 2) when compared to control group-C, where most patients had moderate cough (Extubation Quality Score 3). Dexmedetomidine 0.5 µg/kg given as a single‑dose bolus before tracheal extubation has been shown to attenuate airway-circulatory reflexes during extubation. We observed a statistically significant difference (P – values). Table -3 Adverse effects in Study group-D were less when compared to Control-C.12 Central stimulation of parasympathetic outflow and inhibition of sympathetic outflow from the locus coeruleus in the brainstem plays a prominent role in the sedation and anxiolysis produced by dexmedetomidine. Decreased noradrenergic output from the locus coeruleus allows for increased firing of inhibitory neurons including the g-amino butyric acid system resulting in anxiolysis and sedation.13 We found that most patients in study group were drowsy but responding to verbal commands (Ramsay Sedation Scale 3) after extubation when compared to control group, where most patients belonged to Ramsay Sedation Scale 2. Dexmedetomidine 0.25 µg/kg/hour has been used for sedation during mechanical ventilation in pediatric patients and found to be as effective as midazolam 0.22 mg/kg/hour.14 The quality of sedation is better and the need for rescue sedation is less with dexmedetomidine use as compared with midazolam and there is no significant adverse effect on hemodynamic or respiratory function.15 The activation of α2 adrenoceptors, imidazoline-preferring receptors, or both in the ventrolateral medulla and especially in the solitarius nucleus tract by dexmedetomidine causes bradycardia. In our study, the incidence of bradycardia and hypotension was higher in study group than in control group. Dexmedetomidine 1µg/kg followed by 0.2‑2.5µg/kg/hour has been found to reduce HR in patients.16 A higher frequency of postoperative hypotension has been reported when patient controlled analgesia with dexmedetomidine is administered.17 Our study found insignificant difference in the incidence of vomiting between the two groups. However, others have found a higher, though not statistically significant, prevalence of adverse events (i.e., hypotension, bradycardia, and perioperative nausea and vomiting) with use of dexmedetomidine.18 In our study, none of the patients in either group developed respiratory depression, laryngospasm, bronchospasm, undue sedation or desaturation. Similar findings have been made by Guler et al.19 Dexmedetomidine use in morbidly obese patients has been found not to induce respiratory depression at clinical doses although it improved quality of postoperative analgesia.20 Our result are comparable with that of Aksu R et al,21 Kothari D et al,22 Bindu B et al23 and Erdil F et al24 in all aspects controlling haemodynamic, safe extubation scores and preventing post-op complications.
CONCLUSION Use of dexmedetomidine before extubation attenuates the hemodynamic response to extubation. It enables smooth extubation of the trachea and provides adequate sedation postoperatively. Dexmedetomidine increases the incidence of bradycardia and hypotension, but does not cause side effects like respiratory depression, laryngospasm, bronchospasm, undue sedation and desaturation.
REFERENCES
|
|
 Home
Home