Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 2 -August 2017
Prevalence of acute neuropathic pain after cancer surgery: A prospective study
Surya N1, Vamshi Kiran2*, Murari3
1,2Assistant Professor, 2Associate Professor, Department of Anaesthesia, R.V.M Institute of Medical Sciences and Research Center, Siddipet, Telangana, INDIA. Email: nunavathsurya007@gmail.com
Abstract Aim: The aim of this study was to evaluate the prevalence of neuropathic pain after cancer surgery on the 1st, 2nd and 5th day using visual and verbal analogue scales. Materials and Methods: This study was conducted on all patients were treated for pain. All the patients were given paracetamol round the clock. This is a prospective study which included patients who had major cancer surgery during the defined period. The patients who had a neuropathic pain history before the operation and patients who refused to undergo the survey were excluded from the study. The pain score was calculated using visual and verbal analogue scale (VAS) after 1st, 2nd and 5th day after surgery. Results: This study had 200 patients out of which males were 70 (35%) were males and 130 (65%) were females. Neuropathic pain prevails before surgery and is dependent on gender and anxiety. Before surgery, females tend to have more neuropathic pain as they have more anxiety compared to males. On the first day, Females: Males ratio and anxiety was 10/4, On the second day, it was 10/6 and on the 5th day, it was 10/5. Conclusion: Neuropathic pain is common after any surgery including cancer surgery. This study focuses on the relationship between post operative pain with the occurrence of ANP to assessment of neuropathic pain and that it doesn’t lead to persistent neuropathic pain. Neuropathic pain depends on gender and anxiety before surgery. Key Words: acute neuropathic pain.
INTRODUCTION A disease of the somatosensory nervous system causes neuropathic pain. Consequent to medical disease or surgery or trauma showing pain with sensory dysfunction causes acute neuropathic pain (ANP).1 The presence of symptoms and signs of neuropathic pain distinct from the typical post-operative nociceptive pain which generally is localised to surgical incision and is sharp and self-limiting is the characteristic of acute post-surgical neuropathic pain. ANP is experienced by 1-3% of the population in the developed world, when prevalence estimation was done.2 On further progression, ANP may proceed to persistent post-operative pain and which leads to disability permanently. After surgery, persistent pain may be due to a large component of neuropathy, which is caused from nerve injury during surgery and this pain may persist for months or years after the surgical wound has healed. The severity and persistence of neuropathic pain is often due to psychological, physical, economic, emotional well-being of patients.3 Before neuropathic pain becomes severe and chronic, it is better to prevent after surgery. After operations such as groin hernia repair, thoracic and breast surgery, coronary artery bypass surgery, amputation of leg, persistent pain follows acute post-operative in 10-50% of individuals. Persistent post-surgical pain constitutes a large and major under diagnosed clinical problem, since chronic pain can be severe in about 2-10% of the patients4,5. The most important cause of long-term post-surgical pain is iatrogenic neuropathic pain. Whenever possible, surgical techniques that avoid nerve damage and consequent pain should be avoided. The aim of this study was to evaluate the prevalence of neuropathic pain after cancer surgery on the 1st, 2nd and 5th day using visual and verbal analogue scales.
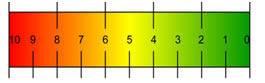
MATERIALS AND METHODS This study was conducted from January 2015 to May 2015. 200 patients were questioned during this period. As per the post-operative pain protocol, all patients were treated for pain. All the patients were given paracetamol round the clock. This is a prospective study which included patients who had major cancer surgery during the defined period. The patients who had a neuropathic pain history before the operation and patients who refused to undergo the survey were excluded from the study. The pain score was calculated using visual and verbal analogue scale (VAS) after 1st, 2nd and 5th day after surgery. Pain was calculated as per the follows: No pain- 0 point, Mild pain-1-3 points, Moderate-4-6 points, Severe-7-8 points and Unbearable pain-9-10. Anxiety and depression were also evaluated accordingly Normal-0-7, Mild-8-10, Moderate-11-14, Severe-15-21. The statistical data analysis was Chi square and correlation coefficient tests were used. p<0.05 was taken as significant.
Figure 1: Shows visual analogue scale Worst imaginable pain No pain
RESULTS This study had 200 patients out of which males were 70 (35%) were males and 130 (65%) were females. Mean ±SD age of the patients in study is 55.96±6.8
Table 1: Risk factors and characteristics of developments of patients with acute neuropathic pain before and after surgical procedure during 1st, 2nd and 5th day
Table 2: Anxiety among genders (F/M)
Table 1 and 2 shows that neuropathic pain prevails before surgery and is dependent on gender and anxiety. Before surgery, females tend to have more neuropathic pain as they have more anxiety compared to males.
Table 3: Surgical procedure and its pain intensity on the first day and second day
Table 4: Shows surgical procedure and its pain intensity on the fifth day
DISCUSSION Many studies have reported the prevalence of neuropathic pain after cancer surgery. PN Jain et al,6 conducted a prospective study on 300 patients to identify the prevalence of ANP in the post-operative period by using a neuropathic pain detection questionnaire tool. This is an open label study in which patients with six different types of cancer surgeries (Thoracic, gastrointestinal, gynae/Urology, bone/soft tissue, head and neck and breast subgroups-50 each) were included for pain Detect questionnaire tool on the 2nd and 7th day surgery. This study found a 10% point prevalence of ANP. Analysis showed that 25 patients had possible ANP, the maximum from urological cancer surgery6 followed by thoracic surgery5. Five patients were found to have positive ANP including 2 groin node dissection, 2 hemipelvectomy and 1 oesophagectomy. Significant relationship between severity of post-operative pain was found with the occurance of ANP in the post-operative period requiring a special attention to neuropathic pain assessment. Liuda Brogiene et al,7 conducted a study in which acute neuropathic pain can be one of the post-surgical pain components, which is often under-recognized and complicated to treat. The pre- valence of pain with neuropathic characteristics in general population is about 6 – 8%. Moreover, it might to progress and become as a persistent pain and cause a disability. This type of study has never been performed in Lithuania. Investigators conducted a survey, which consisted of the following visual and verbal analogue and Dolour Neuropathique 4 scales to identify pain intensity and neuropathic pain after surgery. Risk factors of neuropathic pain were evaluated with Hospital Anxiety and Depression scale, demo- graphic characteristics and data, which represents possible risk factors. The survey included 170 participants: 68 males (40%) and 102 females (60%). Average age of patients was 59.66 years (SD 15.9). During the first day after surgery 7.1% patients felt neuropat- hic pain, on the second day – 8.2%, and the third postoperative day – 7.6% of patients. A prevalence of neuropathic pain depends on gender and anxiety before surgery. A prevalence of acute neuropathic pain after surgery in Hospital of Lithuanian University of Health Sciences is 7 – 8%. The risk factors of neuropathic pain development are patient’s gender and anxiety before surgical procedure. Tasmuth T et al,8 conducted a study which assessed pain, neurological symptoms, oedema of the ipsilateral arm, anxiety and depression occurring in women treated surgically for breast cancer, the impact of these symptoms on daily life and how they evolved during the 1 year follow-up. Ninety-three consecutive patients with non-metastasised breast cancer who were treated during 1993-94 were examined before surgery and after 1, 6 and 12 months. They were asked about pain, neurological symptoms and oedema in the breast scar region and/or ipsilateral arm. Sensory testing was performed, and gripping force and the circumference of the arm were measured. Anxiety and depression were evaluated. One year after surgery, 80% of the women had treatment-related symptoms in the breast scar region and virtually all patients had symptoms in the ipsilateral arm. The incidence of chronic post-treatment pain was higher after conservative surgery than after radical surgery (breast area: 33% vs 17%, NS; ipsilateral arm: 23% vs 13%, NS). Numbness occurred in 75% and oedema of the ipsilateral arm in over 30% of the patients after both radical and conservative surgery. Phantom sensations in the breast were reported by 25% of the patients. No difference in psychic morbidity was detected after the two types of surgery. Both the anxiety and depression scores were highest before surgery, decreasing with time, and were significantly correlated with preoperative stressful events. Maguire MF et al,9 conducted a study to assess the prevalence of chronic pain after thoracic surgery, the contribution of the neuropathic component of chronic pain and the impact of chronic pain on patients' lives. A questionnaire was sent to 1152 patients who had undergone thoracic surgery in our department between 7 months and 7 years ago. The questionnaire was designed specifically for the study and included questions on neuropathic symptoms. Responses were correlated with data from our prospectively entered database for analysis. Nine hundred and forty-eight people were included in the study, of which 600 responded (63%). Prevalence of chronic pain is 57% at 7-12 months, 36% at 4-5 years and 21% at 6-7 years. Patient age, consultant and time since the operation all have significant effects. Surgical approach (video-assisted thoracoscopic surgery, thoracotomy) and diagnosis are not significant. Thirty-nine percent of those with pain take analgesia, 46% felt their pain is their worst medical problem and 40% reported it limits their daily activities. The prevalence of each neuropathic symptom is between 35 and 83%. The presence of a neuropathic symptom is associated with significantly more severe pain, more analgesia use and pain more likely to limit daily activity. Chronic pain has a significant prevalence and impact on patients' lives for several years after thoracic surgery. Nerve dysfunction is associated with more severe pain, a greater impact and tends to persist. The reason for the individual consultant being an important factor in post-thoracotomy pain needs further investigation. Kalso E et al, 10conducted a study to determine the effectiveness of amitriptyline in relieving neuropathic pain following treatment of breast cancer was studied in 15 patients in a randomised, double-blind placebo-controlled crossover study. The dose was escalated from 25 mg to 100 mg per day in 4 weeks. The placebo and amitriptyline phases were separated by a 2-week wash-out period. Visual analogue and verbal rating scales were used for the assessment of pain intensity and pain relief. Other measures included the number of daily activities disturbed by the pain, the Finnish McGill Pain Questionnaire, adverse effects, anxiety, depression, pressure threshold and grip strength. Amitriptyline significantly relieved neuropathic pain both in the arm and around the breast scar. Eight out of 15 patients had a more than 50% decrease in the pain intensity ('good responders') with a median dose of 50 mg of amitriptyline. The 7 patients who had a less than 50% effect had drug concentrations equaling those of the good responders. The 'poor responders' reported significantly more adverse effects with amitriptyline and placebo than the good responders. It is concluded that amitriptyline effectively reduced neuropathic pain following treatment of breast cancer. However, the adverse effects of amitriptyline put most of the patients off from using the drug regularly.
CONCLUSION Neuropathic pain is common after any surgery including cancer surgery. This study focuses on the relationship between post operative pain with the occurence of ANP to assessment of neuropathic pain and that it doesn’t lead to persistent neuropathic pain. Neuropathic pain depends on gender and anxiety before surgery.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home