Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 3 -September 2017
Efficacy of caudal epidural clonidine against fentanyl in prolonging the post-operative analgesia along with Bupivacaine
Pournima Balajirao Panchal1, Manisha Anilkumar Khamkar2*
1Sr. Resident, Department of Anaesthesia, D Y Patil Medical College Pimpri, Pune, Maharashtra, INDIA. 2Assistant Professor, Department of Anaesthesia, MIMER Medical College, Talegaon Pune, Maharashtra, INDIA. Email: manisurwade@gmail.com
Abstract Background: Aim of study was to evaluate the efficacy of caudal epidural Bupivacaine plusClonidine to that of Bupivacaine plus Fentanyl in prolonging the post-operative analgesia. Materials and Methods: Study was conducted among 60 children and divided in two groups randomly. Patients in group C received 0.75 ml/kg of 0.25% bupivacaine plus clonidine 1mcg/kg and group F received 0.75 ml/kg of 0.25% bupivacaine plus fentanyl 1mcg/kg. Caudal block was performed after induction and before the start of surgery, using standard techniques. Postoperative monitoring was done. The assessment of pain relief was done by using an objective pain score (Hannallah-Broadman). In addition to the duration of surgery, duration of pain free period, time to void and any other complications such as nausea, vomiting, motor weakness, respiratory depression, sedation, hypotension and bradycardia etc were also recorded. At the onset of pain, rescue analgesia was given as appropriate and the total duration of analgesia was noted. Results: Both the groups were comparable with respect to age, weight and duration of surgery. There was significant difference in objective pain score values between the two groups during postoperative period, values were lower in Group C. Sedation score was lower in group F as compare to group C which was statistically significant except at 9th, 12th, 18th and 24th hours. There was significant difference between the two groups with respect to time at which analgesia was required. Conclusion: In prolonging the post-operative analgesia, Bupivacaine plus Clonidine given as caudal epidural analgesia was more effective than Bupivacaine plus Fentanyl. Key Words: Caudal block, clonidine, fentanyl, post-operative analgesia.
Pain is a protective mechanism designed to alert the body to potentially injurious stimuli. The International Association for the Study of Pain has defined pain as ‘an unpleasant sensory and emotional experience, associated with actual or potential tissue damage’.1 The alleviation of pain has been the focus of continuing human effort. However, it has been recognized for some time that the management of acute pain, specially, postoperative pain has been consistently inadequate. The situation in children has been even worse; children have long been under-medicated for acute pain3. The report by the audit commission ‘children first’, outlines the proposals for continuous audit to assess the quality of overall care given to children in hospitals. Pain relief is one of the 10 proposed quality indicators2. Fortunately, attitude to treating pain in infants has changed dramatically during the past 15 years. Nevertheless as recently as 1987, Vaster was prompted to write that it is unacceptable to continue to neglect the safe application of analgesics in our youngest patients.3 Caudal epidural block is one of the most common regional anesthetic techniques in children being used to supplement general anesthesia for a wide variety of surgeries.4-7 The local anaesthetics currently in use are safe and their pharmacological effects have been well evaluated. The use of adjuvant in caudal block has several advantages. Several studies have demonstrated that adjuvant when added to the local anesthetic in caudal block enhances and prolongs the analgesia produced by the block. The study was done to clinically evaluate the efficacy of caudal epidural Bupivacaine plus Clonidine to that of Bupivacaine plus Fentanyl in prolonging the post-operative analgesia.
MATERIALS AND METHODS After receiving the institutional ethical committee approval and informed written consent from parents the study was initiated during June 2011 to June 2014 at tertiary care hospital and teaching institute at Pune. Total 60 children were selected by using following mentioned inclusion and exclusion criteria.
Inclusion Criteria • Children between 1 to 12 years of age. • Children undergoing elective lower abdominal surgeries like hypospadias, inguinal hernia repair, and orchidopexy using single shot caudal epidural block • ASA I and ASA II physical status.
Exclusion Criteria Bleeding disorder Patient with known allergy to local anesthetics Mentally retarded patients Patient refusal for informed consent (consent of next to kin) Infection over the sacral region and those with obvious bony anomalies of the sacrum
The selected children were randomly divided into two equal groups. Group C: received 0.75 ml/kg of 0.25% bupivacaine plus clonidine 1mcg/kg Group F: received 0.75 ml/kg of 0.25% bupivacaine plus fentanyl 1mcg/kg
All the selected cases were undergone thorough preanesthetic assessment, including detailed history, clinical examination and relevant laboratory investigations. The spine was examined for any evidence of sacral anomalies, skin infection, bony landmarks, movements and previous operations. Any child with a suspicion of infection over the sacral region and those with obvious bony anomalies of the sacrum were excluded from the study. NBM period was 6 hours prior for solid food, 4 hours prior for breast milk and 2 hours prior for clear liquids. Premedication was done with inj glycopyrrolate (10 ug/kg) intramuscularly. General anaesthesia was induced with inj thiopentone 5-6 mg / kg intravenously. Inj. Vecuronium 0.1 mg/kg intravenously was used to facilitate endotracheal intubation. Maintainance of anesthesia was done with Oxygen + Nitrous oxide + Isoflurane. Inj Vecuronium was used for muscle relaxation. Caudal block was performed after induction and before the start of surgery, using standard techniques. The patient was monitored using standard monitoring i.e. blood pressure (non invasive), pulse-oximetry, heart rate and ECG during the course of surgery. Intravenous fluids were given as per requirement. The neuromuscular blockade was reversed with inj neostigmine 50µg/kg and inj glycopyrrolate 10µg/kg at the end of surgery. Postoperative monitoring was done in the post-anesthesia care unit (PACU) for 2-3 hours and in the ward using a standard proforma for next 24 hrs. The assessment of pain relief was done by using an objective pain score (Hannallah-Broadman). In addition the duration of surgery, duration of pain free period, time to void and any other complications such as nausea, vomiting, motor weakness, respiratory depression, sedation, hypotension and bradycardia etc were also recorded. At the onset of pain, rescue analgesia was given as appropriate and the total duration of analgesia was noted. The final results of the study were tabulated and analyzed for significance using standard statistical techniques (sample t test). RESULTS
Table 1: Comparison of age, weight and duration of surgery in Group C and Group F
It was observed that the mean age of patients in group C was 2.46 ± 0.92 years whereas in group F was 2.85 ± 1.06years. The mean weight in group C and group F was 12.83±2.09kg and 12.47±2.34kg respectively. The mean duration of surgery was 112.83±14.36min in group C and 110.17±10.54min in group F. When the difference between age, weight and duration of surgery was compared between group C and group F by using unpaired t-test, it was observed that there was no significant difference between the two groups.
Table 2: Comparison of objective pain score in Group F and Group C
*Statistically significant The objective pain score was recorded at fixed interval in both the groups. And it was seen that there was significant difference in objective pain score values between the two groups during postoperative period i.e. after extubation, at 3, 6, 9, 12, 15, 18, 21 hours. Values were lower in Group C and the difference was found to be statistically significant (p <0.05) post operative up to 15 hours. At 15th hour the objective pain score was relatively higher in bupivacaine with clonidine group, which was due to declining action of caudal epidural.
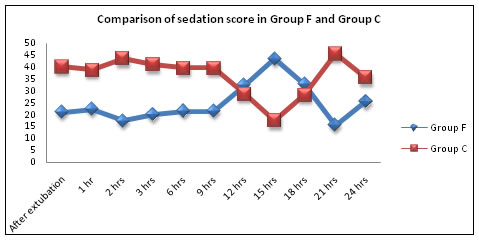
Table 3: Comparison of sedation score in Group F and Group C
* Statistically significant While comparing sedation score in both the groups it was observed that mean rank was lower in group F as compare to group C which is statistically significant except at 9th,12th, 18th and 24th hours.
Figure 1: Comparison of sedation score in Group F and Group C Table 3: Comparison of time at rescue analgesia required (hr) in Group F and Group C
* Statistically significant It was seen that there was significant difference between the two groups with respect to time at which rescue analgesia was required.
DISCUSSION In the present study efficacy of single shot caudal epidural using bupivacaine with fentanyl and bupivacaine with clonidine were compared in 60 ASA grade I and II children undergoing lower abdominal and perineal surgeries under general anesthesia. ECG monitor, peadiatric blood pressure cuff, spo2 probe were used to moniter intraoperative heart rate, systolic and diastolic blood pressure and o2 saturation respectively. The age, weight and duration of surgery were compared between group C and group F and there was no statistically significant difference between both the groups. Thus both the groups were comparable with each other with respect to age, weight of patients and duration of surgery. In the present study, postoperative objective pain score was significantly lower in Group C (bupivacaine with clonidine) at after extubation, 3, 6, 9, 12, 18 and 21 hours as compared to group F. There was no statistical significant difference between Group F and Group C at postoperative 1 and 2 hours (p>0.05). This might be because the analgesic effect of plain bupivacaine in Group F was continuing till postoperative period of 3 to 6 hours. The objective pain score was started increasing in Group F so 29 children received rescue analgesia and the mean duration of analgesia was 6.2 hours. In Group C, 28 children required rescue analgesia and mean duration of analgesia is 15 hours which was statistically significant (p <0.001) when compared to Group F. In our study the sedation score higher in Group C at after extubation and up to 15 hours post-operatively compared to Group F with statistically significant difference (p <0.001). We have not used any intraoperative sedatives in the present study. The mean duration of analgesia in Group C was 15 hrs and was well contributed by sedative and analgesic effect of clonidine. In a study Singh et al8 compared efficacy of clonidine, fentanyl and ketamine in terms of quality and duration of analgesia when added to bupivacaine by single shot caudal in children. They prospectively randomized 80 children undergoing subumbilical surgeries into four groups. Group B received caudal analgesia with 0.75ml/kg of 0.25% bupivacaine in normal saline, Group BC received clonidine 1mcg/kg in addition to 0.75ml/kg of 0.25% bupivacaine, Group BF received fentanyl 1mcg/kg in addition to 0.75ml/kg of 0.25% bupivacaine and Group BK received ketamine 0.5mg/kg with0.75ml/kg of0.25% bupivacaine. In this study duration of post–operative analgesia in Group BC was significantly longer (629.06+-286.32) than other three groups (p<0.05), which was statistically significant. Pain score was lower in group BC. The finding of present study was well compared with the above study. In the present study the efficacy of caudal epidural clonidine with bupivacaine in prolonging post operative analgesia between Group C (bupivacaine with clonidine) and Group F (bupivacaine with fentanyl) were statistically significant at various points. Constant et al9 in their study concluded that addition of clonidine or fentanyl or a mixture of both drugs to local anesthetics prolonged the duration of surgical analgesia after a single shot caudal injection. In our study most of the surgeries were hypospadias so children were catheterized intraoperatively so retention of urine or time of void couldnot be assessed in them. In other surgeries we didn’t find urinary retention. M Gentili et al10 studied incidence of urinary retention after spinal morphine or clonidine. At 12 hr all patient in morphine group but only 5 in clonidine group had bladder distention, and at 24 hrs this was present in 7 patient in morphine group and 1 patient in clonidine group respectively (p<0.001).They conclude that spinal clonidine impaired bladder function to a lesser extent than morphine. Thus in the end we summarize that single shot caudal epidural analgesia was of longer duration in bupivacaine with clonidine group than bupivacaine plus fentanyl group. There were statistically significant lower values of objective pain score at various points in bupivacaine with clonidine group. The sedation score was significantly higher in bupivacaine with clonidine group. This prolonged duration of analgesia was partly due to sedative and partly due to analgesic effect of clonidine when used with bupivacaine.
CONCLUSION Thus we conclude that in prolonging the post-operative analgesia Bupivacaine plus Clonidine given as caudal epidural analgesia was more effective than Bupivacaine plus Fentanyl.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home