Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 3 -September 2017
Laryngeal mask airway insertion in pediatric patients: Comparison of Inventor’s technique with laryngoscopic insertion
Varsha Keshavrao Warke1, Ravindra B Jalkote2*
1Assistant Professor, 2Professor, Department of Anesthesiology, Dr Ulhas Patil Medical College, Jalgaon, Maharashtra, INDIA. Email: drvarsha.md@gmail.com
Abstract Background: The Laryngeal mask airway (LMA) is the development of a new concept in upper airway management and its use is becoming increasingly common in children. Insertion of LMA using Inventor’s technique is a blind technique as the airway is not visualized during insertion. This prospective study in paediatric patients was conducted to find out success rate of LMA insertion with Inventor’s technique as compared to laryngoscopic insertion. Material and Methods: A total of 150 patients of both sexes, ranging in age from 2 to 12 years, weighing between 6 to 30 kilograms were included. They were grouped as Group I- Blind insertion of LMA- Insertion of LMA using Inventor’s technique was attempted in 50 patients. Group II-Insertion of LMA with MacIntosh laryngoscope in 50 patients. Group III- Insertion of LMA with MacCoy’s laryngoscope in 50 patients. Results: The success rate of LMA insertion was 94% in group I, 96% in group II and 98% in group III. In group II and group III, the LMA was inserted successfully in I attempt in maximum patients, while group I required subsequent attempts to insert the LMA. The LMA efficacy was perfect in 34 (68%), 46 (92%) and 48 (96%) in group I, II and III respectively. Key Words: Laryngeal mask airway, tracheal intubation, pediatric patients, blind technique, success rate.
INTRODUCTION Laryngeal mask airway (LMA) is a device that is designed to surround the larynx and provide a stable airway without necessity for tracheal intubation. It has been shown to be an effective means of securing a clear airway in the patients posted for elective surgery. The LMA is the development of a new concept in upper airway management. Its inception is the result of the application of bioengineering and the postmortem examination of the adult larynx. This led to the creation of a prototype mask, which has been the subject of independent studies in spontaneously breathing adults1,2. The LMA is now available for use in children in two sizes. They are the scaled-down versions of the adult forms3. Now days, the use of LMA is becoming increasingly common in children. There are chances of upper airway obstruction in paediatric patients because of anatomical variations of airway than adults, so maintenance of airway is important in this group3. The LMA has become more popular as it maintains airway as well as anaesthetists hands are free to perform other work. Tracheal intubation can be associated with postoperative discomfort and subtle changes in laryngeal function in children and there is a possible risk of laryngeal edema and trauma. With facemask airway maintenance is difficult as both hands of the anaesthetists are engaged and cannot be used for longer duration of surgeries. Insertion of LMA using Inventor’s technique is a blind technique as the airway is not visualized during insertion. While even novice user achieves 71-100% success, airway obstruction is encountered in 2-10% of cases. Alternative insertion techniques are useful in these circumstances such as insertion of LMA using laryngoscope. Using the laryngoscope, it helps to open pharynx and elevates the epiglottis, providing a clear path for LMA insertion under direct vision4. So, we decided to conduct a prospective study in paediatric patients to find out success rate of LMA insertion with Inventor’s technique as compared to laryngoscopic insertion.
MATERIAL AND METHODS This prospective study was conducted on 150 paediatric patients. Children were selected randomly and were ASA (American Society of Anaesthesiology) Grade I and II. Patients of both sexes, ranging in age from 2 to 12 years, weighing between 6 to 30 kilograms were included. Patients with systemic diseases or congenital abnormalities were excluded from the study. Patients with pre-existing airway abnormalities and contraindications to LMA insertion were also not considered for the study. The various operations for which the patients were posted included hernia, hydrocele, cystolithotomy, circumcision repair for hypospadias and corrective surgery for congenital talipusequinovarus (CTEV). All procedures followed were in accord with the standards of ethical committee of our institution. Informed formal consent was obtained in each case, after the procedure had been explained to them. Preoperatively, a thorough pre-anaesthetic evaluation was carried out on all the children who were posted for the surgery. After the confirmation that, the patient was adequately deep under anaesthesia as judged by jaw relaxation plus evidence of stage three surgical anaesthesia as verified by eye position and ventilation pattern, the LMA insertion was done by one of the three techniques – a size #2 LMA was used for children between 6 to 20 Kgs and a size #2.5 LMA for children between 20 to 30 kgs. Group I: Blind insertion of LMA- Insertion of LMA using Inventor’s technique was attempted in 50 patients. Group II: Insertion of LMA with MacIntosh laryngoscopein 50 patients Group III: Insertion of LMA with MacCoy’s laryngoscope in 50 patients
RESULTS In present study, number of male children were much more common than female children. 92-94% were male children and female children constituted 6-8% of total operations. Mean age of the children in group I was 6.9 years, in group II 7 years and in group III 6.8 years. The three groups were formed with respect to equal sample size. The three groups were comparable in age, sex, ASA status and weight (Table 1).
Table 1: Demographic data in all groups
Herniotomy and hydrocele repair were the commonly performed surgeries (Table 2). The success rate of LMA insertion was 94% in group I, 96% in group II and 98% in group III. The average success rate of LMA insertion was 96%. The intubation was done in 6 (12%) of patients out of 150 patients.
Table 3: Number of attempts required to insert the LMA in three groups
(***= p< 0.001 highly significant; **= p< 0.05 significant; *= p>0.05 not significant) In group II and group III, the LMA was inserted successfully in I attempt in maximum patients, while group I required subsequent attempts to insert the LMA. The LMA efficacy was perfect in 34 (68%), 46 (92%) and 48 (96%) in group I, II and III respectively (Table 4). Table 4: LMA efficacy
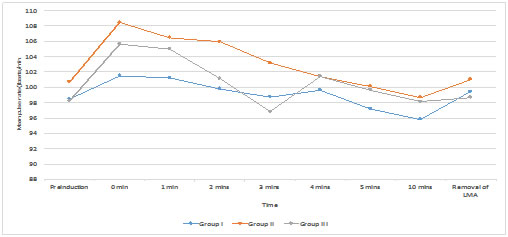
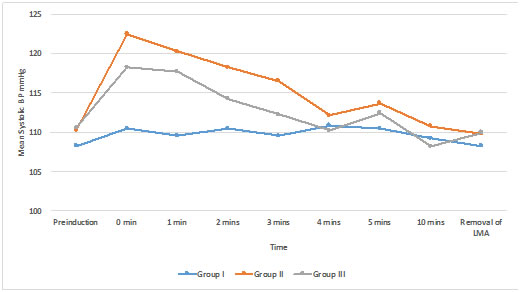
Comparison among all three groups was statistically not significant (p< 0.05). The LMA efficacy was significantly high in group II and group III as compared to group I. Mean time required in seconds for insertion of LMA in three groups was 24.2 secs in group I, 17.2 secs in group II and 16.5 secs in group III. The time required for LMA insertion in group II and group III was less, as compared to group I. Jaw relaxation was good in all patients of three groups. Glottis was visible in 43 (86%) patients in group II and 46 (92%) patients in group III (p>0.05 statistically not significant).Epiglottis and glottis seen in 2 (4%) cases in both groups (p>0.05 statistically not significant). Epiglottis impinging on the grille and glottis seen in 2 (4%) cases in both groups (p>0.05 statistically not significant). Epiglottis down-folded, glottis not seen in 3 (6%) cases in group II (p>0.05 statistically not significant). Comparison between group II and III showed p>0.05, which was statistically not significant. All these conditions while passing LMA were not possible in group I as it was a blind insertion LMA group. There was no significant difference among all the three groups with respect to arterial oxygen saturation and end tidal carbondioxide. Chart A and B: The pressor response during insertion of LMA Figure 1A: Pulse rate - Comparison between three groups
Figure 1 B: Systolic blood pressure – comparison between three groups
The maximum percentage of complications were observed in group I patients in comparison with group II and III patients. Coughing was observed in 2 (4%) in group I and 1 (2%) in group II. Straining was observed in 2 (4%) in group I, 1 (2%) in group II and III. Laryngospasm, breath holding and trauma to uvula occurred in 1 (2%) patient each in group I. Secretions were seen in 2 (4%), 1 (2%) cases in group I and II respectively. Postoperative sore throat was seen in 4 (8%), 2 (4%) and 1 (2%) patients in group I, II and III respectively.
DISCUSSION Induction of anaesthesia in paediatric patients require skill and good amount of experience. Adult patients can undergo surgeries only under regional anaesthesia supported with minimum sedation. But for a child undergoing surgery under regional anaesthesia, it is important to keep the patient quite as well as to maintain the airway only with intravenous or inhalational anaesthetic agents. So, maintenance of airway during regional anaesthesia in pediatrics is an important aspect. The use of laryngeal mask for prolonged “balanced” regional anaesthesia in spontaneously breathing patients has been suggested5. The author claimed that regional anaesthesia can be maintained at light planes and possible complications of tracheal intubation can be avoided. It is not possible to define how long the airway can be safely managed with the LMA but continuous vigilance is required during its use. Airway maintenance can be achieved either with facemask or with endotracheal intubation. But airway maintenance with facemask is difficult for longer duration and tracheal intubation is an invasive procedure, with the possible risk of laryngeal edema and trauma. So, the use of LMA in children is becoming increasingly popular. The blind insertion of the LMA, which is a standard technique described in the manual, is not without hazards. Being a blind technique it can traumatize the oral cavity structures and the LMA may not fit perfectly because of differences in anatomy of pediatric patients than adults. So, there is need for alternative insertion technique such as insertion of LMA with the use of laryngoscope. The McCoy’s laryngoscope has the fulcrum, which is designed to elevate the epiglottis and so expose the larynx, avoiding down-folding of the epiglottis which can cause obstruction. Therefore, this study was conducted to compare the blind insertion technique with insertion of LMA using laryngoscope in pediatric patients. The success rate of LMA insertion at the first attempt was 68%, 98% and 96% in group I, II and III respectively. After second attempt, the success rate in group I increased up to 88% in comparison with 94% and 98% success rate of group II and III respectively. In group I, 3 (6%) patients required third attempt for insertion of the LMA. In group II only 1 (2%) patient required third attempt. But no patient in group III required third attempt. Johnston DF6 also stated the success rate of blind insertion as 67% in first attempt. In our study, group III showed a good success rate of 96%. This was possible with the use of McCoy’s laryngoscope. Tuckey JP7 stated that the levering laryngoscope should be present in the operation theatre. We believe that clinical airway patency does not guarantee ideal positioning of the LMA in children and that care should be taken to ensure continued airway patency because of tendency of the LMA to dislodge in the age group of children. So one should always be vigilant. Mizushima8 also observed the similar findings. In the comparison among three groups, group II and III seem to be more efficacious than group I. It must have been possible because the LMA was inserted under the direct vision in group II and III. Elwood4 studied the LMA insertion in pediatric patients with laryngoscope and found that the best score with fiber optic laryngoscope for epiglottic position was obtained more frequently when the laryngoscope was used to insert the LMA. So, the epiglottis which is large, floppy in pediatric age group, might obstruct the ventilation after the blind LMA insertion and decrease the efficacy of the LMA. But when the best position of epiglottis is obtained by use of laryngoscope it may increase the efficacy of the LMA4. In our study, we have used laryngoscope to insert the LMA in group II and III which shows the high efficacy of the LMA than group I (blind insertion technique). The ease of insertion was assessed by the time taken to complete the LMA insertion. Thus insertion was easy in 96% in group III and 92% in group II which was highly significant difference from group I. We noted the time required for inserting the LMA i.e., from removal of the facemask until confirmation of breath sounds with the LMA taped in place. Barbara O’Neill9 studied the time taken for insertion of the LMA in inflated vs deflated LMA and found 16 secs vs 23 secs (p<0.05). In our study all deflated LMA were inserted. The time required (mean) for group I to insert the LMA was 24.2 secs which is similar to that of 23 secs of deflated LMA group in Barbara O’Neill study. Also, in our study the mean time required in laryngoscopic insertion of LMA group 17.2 secs and 16.5 secs in group II and group III also correlates with the inflated group of his study. The possible explanation for Neill’s study is the partially inflated LMA can smoothly slide over on hard palate because of smooth external surface requiring less time. In or study, in group II and group III the LMA was inserted under vision avoiding the interference during insertion (like large, floppy epiglottis), so it required less time. Therefore, blind insertion of the LMA required more than laryngoscopic insertion of the LMA. With the aid of laryngoscopy, insertion of the LMA is achieved in minimum time, again improving the success rate of insertion of the LMA. The time required to insert the LMA is more important in pediatric age group as children are more prone for hypoxia. Minimum time required to pass the LMA avoids hypoxia. Group II and III required minimum time for insertion of LMA avoiding hypoxic events, in pediatric patients. In our study, the jaw relaxation was adequate in all patients in three groups. Patients were taken adequately deep under anaesthesia, so as to increase the success rate in all age groups. Difference in airway anatomy, make the potential for technical airway difficulties greater in children than in adults. Tuckey7 recommended that the levering laryngoscope should be added to the armamentarium of aids of difficult airway available in the theatre suite. An epiglottis, that is completely folded down does not obstruct the airway per se, as airflow can continue around the lateral margins of epiglottis. This probably accounts for no incidence of desaturation in our study. Brain AIJ10 also stated the same. Braude N11 stated that the experimental and clinical evidence suggests that the pharyngeal wall stimulation associated with laryngoscopy is the major cause of pressor response. However, the blind insertion of the LMA which does not require laryngoscope, introduction of the device and the inflation of cuff stimulates and exerts pressure on anterior pharyngeal wall. This is almost certainly the mechanism by which the increase in pulse rate and blood pressure occurs. The transient nature of response suggests that this is not related to the continuous pressure exerted by the sealing cuff. The reduce response may reflect the lesser stimulus compared to laryngoscopy. Wilson et al12 in a similar study on 40 patients compared increased in heart rate at airway placement, 30 secs after that and at 1 min intervals for 5 mins. At airway placement there was no difference in the mean increase in pulse rate in both groups. But after 30 secs the patient in group II had 6% increase in pulse rate whereas in group I there was no change. The 1 min reading were similar in both the groups. Wilson concluded that the smaller cardiovascular response to the LMA insertion reflects a smaller degree of total afferent stimulation. Griffin et al13 and Aktar et al14 did not find any significant difference in pulse rate in the LMA group and the tracheal tube group. But in both studies pulse rate was monitored intermittently which may have failed to detect transient extremes of changes in pulse rate. In our study, patient in three groups showed increase in systolic blood pressure after induction at 0 min. In group I increase in systolic blood pressure was 2.2±1.18 mm Hg, 12.2±0.76 mm Hg in group II and 7.66±0.80 mm Hg in group III. Wilson et al demonstrated a mean increase in systolic blood pressure in group I of 51.3% and in group II 22.9% after airway placement (p<0.01). It was observed in our study that there was a minimal rise in systolic blood pressure in group I. In group II, the rise was maximum and was maintained for 2 mins which was statistically significant. In group III, the rise was moderate and was sustained for 1 min only. Wilson reported duration of 3 mins in the intubated patients. In group II, the systolic blood pressure had not increased significantly from baseline values at any point during the procedure. Holden et al15 reported mean increase of 7.7 mm Hg after extubation compared with the mean decrease of 0.1 mm Hg in LMA group. As mentioned earlier this could be because patients were extubated in his studies at a deeper plane of anaesthesia, as we did. Therefore, the use of the LMA is associated with significantly smaller increase in systolic blood pressure at insertion and removal in group I. In group II (2 mins) and group III (1 min) systolic blood pressure was maintained for a short period of time. Even though there is minimum rise in heart rate and systolic blood pressure associated with the use of laryngoscopic insertion of LMA in comparison with that of blind insertion, it is transient and sustained for a shorter duration of time. In group I, laryngospasm occurred in one patient, breath holding in another patient. In blind insertion because of secretions which must have irritated the oropharyngeal structures leading to laryngospasm. Coughing, gagging and laryngospasm may occur when the depth of anaesthesia is too light during placement of the LMA, maintenance of anaesthesia or removal. Takashi et al commented that the incidence of complications at induction is less in children and infants. Barbara O’Neill experienced an overallcomplication rate of 26.7% including cough (20.8%), laryngospasm (1.7%) and vomiting (4.2%). Pennant and White16 stated that coughing and laryngospasm occur about as frequently with the LMA as with an oropharyngeal airway and are usually caused by insertion in the presence of inadequate anaesthesia. SarmaVJ17 has also reported one incidence of laryngospasm when the LMA was introduced before the patient was sufficiently anaesthetized. To conclude, LMA insertion with laryngoscope is better than blind insertion in pediatric age group as it improves the success rate, decreases the number of attempts required, requires less time, allows better conditions by visualization of oral cavity structures for insertion. The rise in pulse rate and blood pressure is minimum and of shorter duration and moreover, it reduces the incidence of complications as LMA is passed under vision.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home