Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 1 July2018
Low dose hyperbaric bupivacaine and fentanyl for spinal anaesthesia in caesarean section
S J Kulkarni1*, S O Ruhatiya2, V P Kelkar3, P P Nayak4
1Professor, 3Associate Professor & HOD, 4Professor, Department of Anaesthesiology ,MGM Medical college , N-6, CIDCO, Aurangabad 431003 INDIA. 2Senior registrar, Department of Anaesthesia, Fortis Hospital, Mulund, Mumbai. INDIA. Email: drsanhitakulkarni@gmail.com
Abstract Background and Aims: Neuraxial administration of opioids with local anaesthetics improves the quality of intraoperative analgesia and also provides postoperative pain relief for longer duration. The purpose of this study is to examine the effect of two different doses of inj Fentanyl with bupivacaine for caesarean section. Material and Methods A prospective randomized, double-blind study was performed in patients of ASA grade I and II undergoing elective caesarean section. Ninety female patients randomized into three groups. Group A received 0.5% hyperbaric bupivacaine 10 mg, Group B received 0.5% hyperbaric bupivacaine 7.5 mg + 12.5μg of Fentanyl + normal saline and Group C received 0.5% hyperbaric bupivacaine 7.5 mg + 25 μg of fentanyl (total volume 2ml) intrathecally. All the patients were assessed for onset and duration of sensory and motor block, maximum level of sensory block, haemodynamic stability, APGAR score and side effects like nausea, vomiting, respiratory depression, shivering and pruritus. Results The onset of sensory block was earlier and duration was longer in group C as compared to group A and B. (p <0.05). Onset of motor block was earlier and duration longer in group A than group B and group C, the difference being statistically significant (p<0.05). Haemodynamic parameters (PR and MAP) were stable and comparable intraoperatively in all the 3 groups (p>0.05). Quality of intraoperative analgesia was excellent in group B and C than group A. The difference in the three groups was statistically significant (p=0.0097). Pruritus was seen only in group C. The difference in the incidence of pruritus was statistically significant.(p=0.000) Conclusion Addition of 12.5 μg fentanyl to bupivacaine intrathecally causes less side effects as compared to 25 μg and results in early motor recovery hence it is recommended to use safely in caesarean section Key Word: Bupivacaine, caesarean section, fentanyl , spinal anaesthesia
INTRODUCTION Spinal anaesthesia is commonly employed for caesarean delivery. It carries high efficiency, avoids polypharmacy, having minimal neonatal depression, awake mother and lesser incidences of aspiration pneumonitis.1 Caesarean delivery involves traction of peritoneum and handling of intraperitoneal organs, resulting in intraoperative visceral pain. Intrathecal bupivacaine, most commonly used local anaesthetic drug, alone may be insufficient to provide complete analgesia despite the high sensory block. Use of higher doses of intrathecal bupivacaine to overcome this problem are associated with severe hypotension and delayed recovery of motor block2 Therefore smaller doses of bupivacaine supplemented by intrathecal opioids have been recommended for spinal anaesthesia in parturients undergoing caesarean delivery.3,7 Neuraxial administration of opioids along with local anaesthetics improves the quality of intraoperative analgesia and also provide postoperative pain relief for longer duration6,8 Fentanyl, a lipophilic opioid, has rapid onset of action following intrathecal administration. In various studies, spinal doses of 10 μg to 25 μg of fentanyl have been used for anaesthesia in caesarean delivery.4,9 It has been found to have no deleterious effects and appears to be safe for the mother and newborn.13 There are very few studies comparing 12.5 μg and 25 μg doses of fentanyl along with low dose bupivacaine. In this study, we observed the effects of two doses of intrathecal fentanyl 12.5 μg and 25 μg with low dose bupivacaine (7.5mg) compared to intrathecal bupivacaine alone in conventional dose (10 mg) in patients undergoing caesarean section. Our primary objective is to study the intraoperative block characteristic and patient comfort and secondary objective is to observe intraoperative haemodynamic changes and complications like pruritis and nausea.
MATERIAL AND METHODS A prospective randomized, double-blind study was performed in patients of ASA grade I and II within age group of 18 to 35 years of undergoing elective caesarean section after obtaining informed written consent from the patients and permission from institutional ethical committee. Patients in whom regional anaesthesia is contraindicated and patients who had obstetric complications or evidence of foetal compromise were excluded from the study. The study population was randomly divided into three groups group A, group B and group C. using computer-generated random numbers, which were contained in a sealed envelope. Sample size of 25 in each group was calculated, taking power of study as 95% (alpha error of 1.96 and beta error of 1.64).Considering the drop rate of 10%, we fixed the sample size(n) as 30 in each group. 90 Patients were divided into three groups of 30 each. Group A received 0.5% hyperbaric bupivacaine (AnawinTM by Neon laboratories) 10 mg (2ml) intrathecally. Group B received 0.5% hyperbaric bupivacaine 7.5 mg (1.5ml) + 12.5μg of preservative free Fentanyl (Trofentyl TM by Troikaa pharmaceuticals) (0.25ml) + normal saline 0.25 ml (total volume 2ml) intrathecally. Group C received 0.5% hyperbaric bupivacaine 7.5 mg (1.5ml)+ 25 μg of fentanyl (0.5ml) (total volume 2ml) intrathecally . An intravenous line was secured with 20G IV cannula. The patients were prehydrated with 500ml of RL solution. Inj. Ranitidine 50mg and Inj Metoclopramide 10mg IV were given half an hour prior to surgery. Baseline pulse rate, blood pressure, arterial oxygen saturation (SPO2), respiratory rate was noted. The person who injected the drug was different from the person who monitored the patient intra as well as postoperatively. Study drugs were prepared in 2ml syringes and Fentanyl was added to bupivacaine with the help of a tuberculin syringe. Under strict aseptic precautions, Lumbar subarachnoid block was performed in L3 –L4 space using 25 gauge Quinke spinal needle in left lateral position. After the block a wedge was kept under right hip. Oxygen was given through face mask at the rate of 4 litre per min. All the patients were assessed for onset and duration of sensory and motor block, maximum level of sensory block, haemodynamic stability, APGAR score and side effects like nausea, vomiting, respiratory depression, shivering, pruritus, etc. if any. Sensory block was tested by pin prick in midaxillary line every 3 min till peak sensory level i.e. two consecutive reading at the same dermatomal level is achieved. Thereafter sensory block was tested every 20 min till the block regression to L1 level. The time to achieve T6 dermatomal level was taken as onset of sensory block. The time from T-0 to L1 regression was taken as duration of sensory block. Motor block was tested every 5 min using Bromage scale till grade 2 motor block was achieved. Bromage scale 0–no paralysis, 1– inability to raise extended leg, 2– inability to flex the knee, 3– inability to flex the ankle. Onset of motor block was taken as time from T-0 to obtaining a motor block of grade 2. Thereafter motor block was tested in post operative period every 15 min till complete recovery (grade 0) and duration of motor block was noted. Surgery was allowed after achieving sensory block up to T10 and grade 2 motor block. In intraoperative period, if patient complained of pain, inj ketamine 0.25mg/kg was supplemented. If required the same dose was repeated. In spite of two doses of ketamine if the patient still complained of pain, general anesthesia was given. Intra operatively, patient was monitored for pulse rate and blood pressure every 2 min for first 10 min and every 15 min up to one hour and every 30 min thereafter till the sensory block regresses to L1. The quality of intraoperative analgesia was judged as Excellent (no discomfort or pain, not requiring additional analgesics), Good (mild pain not requiring additional analgesics), Fair (pain requiring additional analgesics), Poor (moderate or severe pain requiring general anaesthesia). During the procedure all patients were infused appropriate quantity of intravenous fluid. Episodes of nausea, vomiting, pruritus, shivering were noted. Inj ondansetron 4 mg iv was given for nausea and vomiting, Inj nalbuphine 2.5 to 5 mg iv for disturbing pruritus. APGAR score at 1 and 5 min was noted. A pulse rate of less than 60 beats per minute was considered as bradycardia and was treated with injection atropine 0.6 mg intravenously. A decrease in systolic blood pressure by 20% below the baseline was considered as hypotension. It was corrected with rapid infusion of IV fluids and injection mephenteramine 5 mg IV if required was given. Statistical analysis For statistical analysis the Kruskal Wallis test was used to compare categorical data and Analysis of Variance (ANOVA) was used for variable data. A P-value of <0.05 was considered to be statistically significant
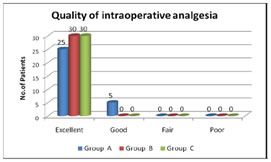
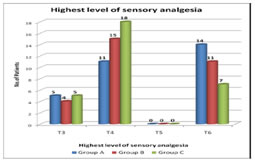
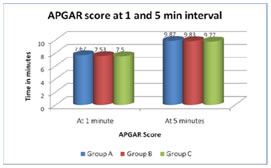
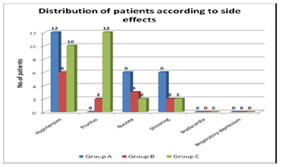
OBSERVATIONS AND RESULTS The demographic data with respect to age, weight, height, and duration of surgery were comparable in three groups.(Table1) The onset of sensory block was 4.66±0.3821min in group A, 4.04±0.7640 min in group B and 3.38±.0.4935 min in group C respectively.(Table2) The difference was statistically significant. (p < 0.05). The median range of highest level of sensory analgesia was T6 (T3-T6) in group A and T4 (T3-T6) in groups B and C where the difference was statistically significant (p < 0.05).(Figure2) Duration of sensory block was significantly longer in group C (202.13±7.52 min) than group A (126.13±6.59 min) and group B (171.76±7.846 min) (p <0.05).(Table2) Onset of motor block was 4.16±0.5888 min in group A, 5.39±0.7205 in group B and 5.57±0.5474 in group C respectively, the difference being statistically significant (p < 0.05). In Group A, duration of motor block was 161.73±12.74 minutes, in Group B 121.36±8.56 minutes. and in Group C138.76±7.51 minutes. The difference was statistically significant (p < 0.05)(Table2). Haemodynamic parameters (PR and MAP) were comparable throughout the surgery in all the 3 groups (p > 0.05). Quality of intraoperative analgesia was excellent in all the patients of group B and group C. In Group-A it was excellent in 83.3%; good in 16.67% The difference in the three groups is statistically significant (p=0.0097) (Figure2). Hypotension was seen in 40%, 20% and 33.3% of patients in Group A, B AND C respectively. The difference was statistically not significant. None of the patients suffered from pruritus in Group A, but 2 patients in Group B and 12 patients in Group C pruritus which subsided without treatment. The difference in the incidence of pruritus was statistically significant. Nausea was seen in 20%, 10% and 6.7% of patients in Group A, B and C respectively, the difference was statistically not significant. Bradycardia and respiratory depression was not found in any of the patients. APGAR score was comparable in all the three groups.(p>0.05)
. Table 1: Demographic data. Results are given as mean ± SD.
NS = Not significant Table 2: Comparison of sensory and motor block parameters
S = Significant, HS = Highly significant, * mean ± SD, † median (range)
Figure 1: Quality of intraoperative Analgesia
DISCUSSION Fentanyl in various doses ranging from 10 µg to 25 µg have been tried in subarachnoid block in caesarean section along with local anaesthetics with the aim of improving the quality of intra operative analgesia and post operative pain relief. Fentanyl is more lipid soluble and is readily eliminated from the CSF making delayed respiratory depression less likely In our study we compared effects of 12.5 µg and 25 µg Fentanyl as an adjuvant to Bupivacaine in spinal anaesthesia in caesarean section. In our study demographic data were comparable in the three groups. (p>0.05). In our study, the mean time of onset of sensory block at T6 in Group A was 4.66±0.3821 minutes, in Group B was 4.04±0.7640 minutes and in group C was 3.38±0.4935 min. The difference in the mean time between Group A, Group B and group C was statistically significant (p < 0.05). This showed addition of fentanyl to bupivacaine hastens the onset of sensory block. Shende D et al[4 ]conducted a study on 40 healthy parturient scheduled for elective caesarean section randomly allocated to receive either 0.3 ml 0.9% normal saline or 15 μg (0.3 ml) Fentanyl added to 2.5 ml of 0.5% hyperbaric Bupivacaine given intrathecally. They observed that sensory block to T4 was achieved after 6.5 min in those who received Fentanyl compared to 8.0 min in the control group. The results of this study are in accordance with our study. In our study, majority of the patients in group A (46.7%) achieved the highest sensory level of T6 where as in group B (50%) and group C (60%) the highest sensory level achieved was T4. Our result concurs with the following study. In study conducted by B N Biswas et al[11], highest sensory level (range) in Group A, (10 mg bupivacaine alone) was T7 (T6-T8) and in Group B (10 mg bupivacaine with 12.5 μg fentanyl) it was T5 (T4-T6) which is almost similar to our study. According to Hunt CO et al[ 6] the onset time to T4 in Group O i.e. bupivacaine alone is 4.571 ± 2.76minutes and in Group with 12.5μg Fentanyl the mean time of onset was 4.222 ± 2.108minutes and with 25μg Fentanyl the time of onset 3.5 ±1 min. The results of our study concur with the findings of the above authors. It was found that patients receiving a combination of fentanyl and bupivacaine had a statistically significant faster onset of action. In our study time for sensory regression to L1 in Group A, (10 mg bupivacaine alone), was 126.13±6.59 minutes, in Group B (bupivacaine 7.5 mg + 12.5 μg fentanyl) 171.76 ± 7.846 minutes and in Group C (bupivacaine 7.5 mg + 25 μg fentanyl) 202.13 ± 7.52 minutes. The difference in the mean time between Group A, Group B and group C was statistically significant (P=0.000).This shows that addition of Fentanyl to intrathecal bupivacaine increases duration of sensory block. Similar results were noticed with Biswas BN et al11, Singh H et al12, Harsoor SS13. Biswas BN et al11 observed that sensory regression to L1 in Group I, i.e. bupivacaine alone was 116 ± 14.39 minutes and in Group II, i.e. with fentanyl combination it was 151 ± 7.33 minutes and it was statistically significant. Singh H et al12 observed time for sensory regression to L1 in group I (13.5 mg bupivacaine) was 110 ± 33 min and in group II (13.5mg bupivacaine + 25 μg fentanyl) was 141 ± 37 min and the difference was statistically significant. Harsoor SS et al[3] observed time for sensory regression to L1 in group B (8 mg bupivacaine) was 100 min as compared to 167 min in group BF (8 mg bupivacaine + 12.5 μg fentanyl) which was statistically highly significant (p<0.001). It was found that time for sensory regression to L1 was prolonged with increasing doses of fentanyl. In our study quality of intraoperative analgesia was excellent in 100% of the patients of group B and group C i.e. both the fentanyl groups and in group A i.e. plain bupivacaine group, it was excellent in 83.3%; good in 16.67%. Result of our study concur with study done by Harsoor SS et al[13] where they found excellent intraoperative analgesia in 100% patients in bupivacaine fentanyl group as compared to 86% patients in plain bupivacaine group . The difference was highly significant. Motor blockade characteristics In our study the mean time of onset of grade III motor block in Group A i.e. bupivacaine alone (10 mg) was 4.16±0.5888minutes and in Group B, i.e. with 12.5 μg fentanyl it was 5.39 ± 0.7205 minutes and in group C i.e. with 25 μg fentanyl it was 5.7 ± 0.5474 The addition of fentanyl to low dose bupivacaine (7.5 mg) delayed the onset of motor block in group B and group C. The difference in the time of onset of motor blockade between group A and group B and between group A and group C are statistically significant. But the difference in the time of onset of motor blockade between group B and group C was statistically non significant. The onset of motor blockade was not significantly affected by addition of two different doses of Fentanyl with same low dose of bupivacaine. In the study conducted by Biswas BN et al11, Singh H et al12 and Hunt CO et al6, Harsoor SS et al13 the authors did not find significant difference in the onset of motor block where same dose of bupivacaine was used in their different study groups. In our study onset of motor block was earlier where dose of bupivacaine used was higher .This shows that onset of motor block mainly depends on dose of bupivacaine rather than dose of fentanyl. In the present study, the mean time for complete motor recovery was 161.73 ± 12.74 minutes in Group A, i.e. bupivacaine alone and 121.36 ± 8.56 minutes in Group B, i.e.12.5 μg fentanyl group and 138.76 ± 7.51 minutes in Group C, i.e. 25 μg fentanyl group. The difference in the mean time of total duration of motor block in Group A and Group B and group C was statistically significant (p < 0.05). B N Biswas et al11 observed complete motor recovery of 125 ± 6.7 minutes in Group I, i.e. bupivacaine alone and 127 ± 7.1 minutes in fentanyl with bupivacaine group. The difference between the time for complete motor recovery was statistically not significant. Similar results were noticed in the study conducted by Singh H et al.12 Patients received 1.8 ml (13.5mg) bupivacaine 0.75% + 0.5 ml CSF (Group I) and 1.8 ml (13.5mg) bupivacaine 0.75% + 0.5 ml (25 μg) fentanyl (Group II). Time taken for complete motor recovery was 151± 46 minutes in Group I and 169 ± 37 minutes in Group II which was statistically not significant. The results of our study where low dose of bupivacaine (7.5 mg) was used in group B and group C, mean time for complete motor recovery was less as compared to plain bupivacaine group (10 mg). This again shows that duration of motor block depends on dose of bupivacaine. Hypotension was observed in 40% of the patients in Group A and 20% of the patients in Group B and 33.3% the patients in Group C. The difference between the three groups is statistically not significant. All patients responded to rapid infusion of intravenous fluid and 5 mg incremental dosage of mephentermine injection IV. Similar results were obtained in the study done by Biswas BN et al.11 In their study 20%of the patients had hypotension in Group I, i.e. 10 mg bupivacaine alone and it was in 30% of the patients in Group II, i.e. 10 mg bupivacaine with fentanyl 12.5 μg .In a study conducted by Harsoor SS et al13, fall in blood pressure was seen in 53%, and 50% patients in groups bupivacaine alone and bupivacaine combined with fentanyl respectively. These results were statistically not significant. The mean values of pulse rate changes per minute recorded in Group A, Group B and Group C were almost similar. This was statistically not significant. Nausea vomiting was seen in 20% in Group A, i.e. bupivacaine alone and 10% patients in Group B bupivacaine with 12.5 μg fentanyl, 6.7% in group C i.e. bupivacaine with 25 μg fentanyl. In our study this was treated by inj Ondansetron 4 mg IV. Our results showed addition of fentanyl to local anaesthetics reduces the perioperative nausea-vomiting. Our results concurs with the study done by Manullang et al7 They concluded that 20 μg intrathecal fentanyl is superior to 4 mg IV Ondansetron for the prevention of perioperative nausea during caesarean delivery performed with bupivacaine spinal anaesthesia. In 2005 Bogra J et al14 also found incidence of vomiting was more in intrathecal Bupivacaine alone than Bupivacaine and Fentanyl combination group. Our results concur with the results of the metanalysis done by Arzola C et al15 where they observed that dose of bupivacaine less than 8 mg was associated with fewer adverse effects such as hypotension, nausea and vomiting as compared to patients in whom more than 8 mg bupivacaine was used intrathecally for caesarean section. Shivering was observed in 20% of the patients in Group A i.e. bupivacaine alone and 6.7% in Group B, i.e. bupivacaine with 12.5 μg fentanyl group, and 6.7% in Group C, i.e. bupivacaine with 25 μg Fentanyl group These patients were treated with inj tramadol 25 mg. Our results concur with the study conducted by Sadegh A et al16 in eighty healthy women scheduled for elective caesarean section under spinal anaesthesia. The patients received 12.5 mg (2.5ml) of 0.5% hyperbaric bupivacaine combined with 25 μg (0.5 ml) fentanyl in Group F as a study group and 12.5 mg (2.5ml) of 0.5% hyperbaric bupivacaine combined with 0.5 ml normal saline in Group S as a control group. The total incidence of shivering in Group F was significantly lower than Group S (10% in group F; 75% in group S, p< 0.0001). Similar results were found in the study conducted by Techanivate A et al21 in 60 patients scheduled for caesarean section under spinal anaesthesia using 2.2 ml of 0.5% hyperbaric Bupivacaine with 0.2 ml of morphine 0.2 mg received additional 0.4 ml of Fentanyl 20 μg (Group F) or Normal saline 0.4 ml (Group S). They observed that group F had significantly less shivering than group S, 20% in Group F and 50% of group S (P<0.05). Pruritus was observed in 6.7% of patients in Group B and 40% patients in group C and not observed in any patients in Group A, i.e. bupivacaine alone. But it was well tolerated and did not require any treatment our results concur with the results of following authors. Siddik SM et al3 also observed pruritus in 26% of patients in intrathecal fentanyl group. Buvanendran A et al18 in their study noticed pruritus in 95% of patients in fentanyl (25μg) alone group, 36.4% of patients in fentanyl with bupivacaine group and 0% in bupivacaine alone group. One patient in the fentanyl alone group received IV naloxone 0.20.2 mg at 45 min for severe pruritus. The occurrence of pruritus in patients who received fentanyl was dose dependent. In the present study we did not notice any incidence of respiratory depression (respiratory rate<9/min). Similarly no incidence of respiratory depression was noticed in the studies conducted by Biswas BN et al11 Hunt CO et al6 and Singh H et al12 Belzarena S et al19 however noticed a significant low respiratory rate in the initial 40 minutes when dose of intrathecal fentanyl was more than 0.5 μg/kg. But there was no respiratory depression. . There were no differences in neonatal APGAR scores among the groups. Shrivastava U et al20 conducted a study on 60 women undergoing caesarean section who were randomized to receive 10 mg (2ml) of bupivacaine as hyperbaric or plain solutions both with 25 micrograms of preservative free fentanyl for spinal anaesthesia. The neonatal outcome as monitored by APGAR score at 1 and 5 min was unaffected. Similar observations were observed in the studies conducted by Biswas BN et al11, Hunt CO et al4 and Shende D et al6 study. Limitation of our study was that the clinical effects of fentanyl on the neonate could be assessed by only apgar score as facilities to monitor umbilical blood gases and neurobehavioral tests were not available at our centre.
CONCLUSION Combination of fentanyl with bupivacaine for spinal anaesthesia can be safely employed for patients who undergo caesarean section without significant haemodynamic changes, excellent quality of intraoperative analgesia with good maternal satisfaction and foetal well being.Addition of 25 μg of fentanyl to 7.5mg of hyperbaric bupivacaine significantly prolonged the duration of spinal anaesthesia more than 12.5 μg fentanyl bupivacaine group .This in turn was significantly more than the duration of spinal anaesthesia in bupivacaine alone group.Combination of fentanyl with bupivacaine for spinal anaesthesia can be safely employed for patients who undergo caesarean section without significant haemodynamic changes, excellent quality of intraoperative analgesia with good maternal satisfaction and foetal well being. Addition of 12.5 μg fentanyl to bupivacaine intrathecally causes less side effects as compared to 25 μg. Also 12.5 μg fentanyl with bupivacaine results in early motor recovery Hence it is recommended to add 12.5 μg of fentanyl to hyperbaric 0.5% bupivacaine1.5 ml (7.5 mg) for spinal anaesthesia in caesarean section.
REFERENCES
|
|
 Home
Home