Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 2 - November 2018
A comparative study of pre-incisional and post-incisional wound infiltration of bupivacaine for post-operative pain relief in abdominal surgeries
Sheetal S Jayakar1, Surekha S Shinde2*
1Assistant Professor, Department of Anaesthesiology, D Y Patil Medical College, Pimpri, Pune-411018, Maharashtra, INDIA. 2Associate Professor, Department of Anaesthesiology, B J Government Medical College, Pune-411001 Maharashtra INDIA. Email: sheetaljayakar6@gmail.com
Abstract Background: Topical infiltration of local anaesthetic in the surgical site is a simple, easy and attractive technique recommended for providing a longer post-operative pain free period and decreased opioid requirements. Materials and Methods: 50 adults (20-50yrs) scheduled for lower abdominal surgeries under general anaesthesia, were enrolled into 2 equal groups in this prospective, randomized and double-blind study. Group-I received in filtration of 20 ml of 0.25% Bupivacaine before skin incision while Group-II received the same as wound infiltration before skin closure. Post-operatively patients were assessed for severity of pain at 2, 4, 6, 8, 10, 16, 20and 24 hours according to Visual Analogue Scale (VAS). Also patients were observed for duration of analgesia, total no. of doses of Diclofenac sodium required for 24 hours, vital parameters and any complications. Data was analyzed using Chi-square and unpaired t-test. Results: Up to 6 hours all the patients in Group-I and Group-II had no pain to mild pain but after 8 hours all patients in Group-I while only 6 patients in Group-II had mild pain which was statistically significant. After 10 hours statistically, significant no. of Group-II patients had moderate to severe pain compared to Group-I. The mean duration of analgesia in Group I was 9.6± 1.1 hours while it was 8 ±0.8 hours in Group-II which was statistically significant. Total no. of analgesic doses required post-operatively was 1.5 ± 0.34 in Group – I while it was 2.4 ± 0.3 in Group – II which was again statistically significant. There was a significant increase in the vital parameters at 10 hours in group I patients. There was significant increase in vital parameters at 8, 16 and 24 hrs in group II patients. Conclusion: Our study confirms the belief that pre-incisional surgical wound infiltration facilitates a smooth and pain-free transition into post-operative period. Key Word: wound infiltration, Bupivacaine, post-operative pain relief
INTRODUCTION The word ‘PAIN’ which causes majority of us shudder with fear is derived from a Greek word ‘Poine’ which means penalty or punishment. Pain is a subjective sensation and protective mechanism of body (Casey, 1973).1 It occurs whenever tissues are being damaged and it causes withdrawal reflex. Pain can be described as the psychical adjunct to imperative reflex (Sherrington, 1906).2 In 1979, the International Association for the Study of Pain defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damages”. Post-operative pain is associated with adverse psychological and physiological effects. The adverse physiologic effects of post-operative pain includes respiratory compromise from reflex splinting of respiratory and abdominal muscles, increased myocardial work and oxygen consumption, peripheral vasoconstriction, gastrointestinal and urinary dysfunction, impairment of muscle metabolism and decreased physical activity. Any type of surgery is associated with inherent tissue damage. This leads to a series of noxious stimuli, which are transmitted to central nervous system. Pain experienced in the post-operative period is due to pain arising from various structures like skin muscles, bones and viscera organs (Pflung and Bonica, 1977).3 Post-operative pain is maximum in the first 48 hours (Parkhause and Co-workers).4 Various methods like systemic narcotics, non-steroidal anti-inflammatory drugs (NSAIDS), regional anaesthetic techniques like nerve blocks, local anaesthetics, epidural narcotics and psychological methods are employed to relieve pain during this period. Surgical wound infiltration of local anaesthetics for post-operative analgesia was used by Crile in 1918 (Bomca. 1953)5. Topical infiltration of local anaesthetic in the surgical site is a simple, easy and attractive technique recommended for providing a longer post-operative pain free period and decreased opioid requirements. Surgical incision initiates an outflow of nociceptive impulses from wound to spinal cord. This results in NMDA receptor mediated activity dependent alteration in dorsal horn neuronal function called as central sensitization. This central sensitisation leads to amplification and prolongation of post-operative pain. Infiltration of local anaesthetic in the area of skin before surgical incision blocks the sensitising effects of nociceptive outflow resulting in decreasing post-operative pain and analgesic requirement Hence, a prospective study was undertaken to compare the efficacy of pre-incisional and post-incisional wound infiltration of Bupivacaine hydrochloride for postoperative pain relief in lower abdominal surgeries. The study compares the degree, duration of pain relief and demand for additional analgesics required for the first 24 hours after surgery in the above groups.
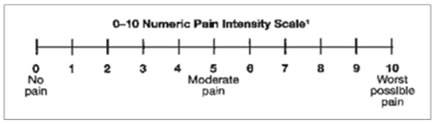
MATERIALS AND METHODS After obtaining approval from the Hospital Ethics Committee along with written and informed consent from patients,50 adults(20-50yrs) of either sex belonging to American society of Anaesthesiology (ASA) physical status class I and II and scheduled for lower abdominal surgeries under general anesthesia, were enrolled in this prospective, randomized and double-blind study. We excluded patients with organ dysfunction, allergy to any drug used, coagulation disorder, local infection at the site of infiltration. All patients were admitted prior to the day of surgery and investigated for haemoglobin, bleeding and clotting time, urine examination, electrocardiogram (ECG). On arrival to the operation theatre, fasting of eight hours was confirmed. Written informed consent for surgery and anesthesia was taken. The technique of anaesthesia and visual analogue scale was explained to all the patients and then a written informed consent was taken. On the day of surgery, Intravenous (iv) line was secured by 18/20G cannula and ringer lactate solution was used as maintenance fluid. Baseline systemic blood pressure (BP), heart rate (HR), Respiratory rate, peripheral oxygen saturation (SpO2) and ECG were recorded using Philips MP 40 monitor. Induction of anesthesia was done with injthiopentone sodium 5mg/kg iv. Tracheal intubation with proper size endotracheal tube was facilitated with inj succinylcholine 2mg/kg iv under direct laryngoscopy. Anesthesia was maintained with 60% nitrous oxide in oxygen and isoflurane. Patients were ventilated manually with Bains circuit to maintain end tidal concentration of CO2 (EtCO2) between 30-35 mm Hg. Inj fentanyl 2µgm/kg was given for intraoperative analgesia. After surgery the residual neuromuscular blockade was antagonised with neostigmine 0.05mg/kg and glycopyrrolate 0.01mg/kg iv. 50 patients were divided randomly in two equal groups. Group-I: Pre incisional Infiltration Group: Infiltration of the proposed skin incision was given with 20 ml of 0.25% Bupivacaine after general anaesthesia. Subcutaneous tissue and skin of the proposed area of skin incision infiltrated with 23 G 1 ½ disposable needle and 20cc disposable syringe. Needle was inserted in the centre of the area with medial and lateral parts of the proposed skin incision infiltrated. Surgery was started 10 min after skin infiltration. Group-II: Post-incisional Infiltration Group: 20 ml. of 0.25% Bupivacaine infiltrated in the skin before skin closure. Subcutaneous tissue of the incised skin infiltrated with 23 G 1 ½ disposable needle and 20cc disposable syringe. Medial and lateral parts of the skin incision were infiltrated. The time of skin incision was taken as zero time in both the groups. Patients were monitored for vital parameters throughout the surgery and post-operative period. Post-operatively, pain relief was assessed at 2, 4, 6, 8, 10, 16, 20and 24 hours. Pain intensity was graded according to the Visual Analoque Scale (VAS). Visual Analogue Scale is a scale having one end indicating no pain whiles other end indicating maximum imaginable pain. Patients were taught to grade their pain on the scale.
Patients responses were scored as 0 to 10 according to severity. VAS was graded as
Patients if developed intolerable pain were given Inj. Diclofenac sodium 75 mg intramuscularly. Patients VAS and time for the first analgesic requirement were noted. The time of the first analgesic requirement was taken as duration of infiltration analgesia Total analgesic requirement in first 24 hours were noted. Post-operatively patients were observed for severity of pain, duration of analgesia, total analgesic required for 24 hours, vital parameters and any complications. Statistical methods: The recorded data were tabulated and expressed in mean ± standard deviation (SD). Statistical analysis was performed using SPSS for Windows software package. The demographic data for categorical variables were compared using Chi-square test. Unpaired Student’s t-test was used for analysing statistical significance in time related variables. P ˂ 0.05 was considered as statistically significant.
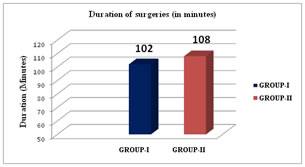
RESULTS The study was completed successfully in 50 patients. The demographic data of Patients i.e. age, Sex, weight and surgical duration were comparable between the groups.(Table No.1) The baseline Heart Rate, Systolic blood Pressures and Respiratory rate were comparable between two groups. Comparing the post-operative pain score by Chi-square test (Table No.2) it was seen that the severity of pain was much less in pre-incisional infiltration group (Group I) as compared to the post-incisional infiltration group (Group-II). There was significant difference in group I and group II (P <0 05). The mean duration of analgesia (Table No.3) in Group I was 9.6± 1.1 hours while it was 8 ±0.8 hours in Group-II which was statistically significant. Total no. of analgesic doses required (Table No.3) post-operatively was 1.5 ± 0.34 in Group – I while it was 2.4 ± 0.3 in Group – II which was again statistically significant. There was a significant increase in the vital parameters at 10 and 24 hours in group I patients (P <0 05). Significant increase in vital parameters was seen at 8, 16 and 24 hrs in group II patients. (P <0.05) (Table No.4)
DISCUSSION The pains of mankind are always with us and there is no greater service to humanity than providing pain relief. To quote Hippocrates “Divine is the task to relieve pain.” The word ‘pain’ is derived from the Latin word Poine which means penalty or punishment that itself is self-explanatory to the nature of pain and need for pain relief. Pain is an unpleasant sensation which only the individual himself can appreciate. It frequently exceeds its protective nature and make the post-operative period a suffering. Post-operative pain needs relief not only on humanitarian grounds, but also to reduce physical morbidity following the operation In the post-operative period the effect of anaesthesia disappears and the tissue injury persists. The cut ends of the axons and the pain producing substances which are liberated during surgery greatly reduce the normal threshold of nociceptors. So the innocuous stimulation produces pain. Transitory nature of post-operative pain makes it more amenable to treatment (Graham Smith, 1990)6. Pain relief in the post-operative period has been of a great concern to the anaesthetist. Multisystem disturbances caused by pain includes stimulation of sympathetic nervous system leading to tachycardia, hypertension and increased myocardial oxygen consumption, increase in the catecholamine and catabolic hormones and decreased secretion of anabolic hormones, reduced physical activity causing venous stasis and platelet aggregation which increases risk of deep vein thrombosis and psychological effects like anxiety, fearful anticipaton, fear of the unknown, uneasiness, restlessness and agitation. Post-operative analgesia can eliminate these disturbances. Narcotics form the mainstay of analgesics for acute control of moderate to severe pain. They can be administered by oral, intramuscular, intravenous, intrathecal and epidural route. Though oral route is most acceptable by patient it is not much useful for post-oprative pain relief as the effect is unpredictable. Narcotics produce excellent analgesia but require extensive patient monitoring. In the post-operative period when the patients are experiencing pain and are drowsy, narcotic administration possess a potential risk of respiratory depression. So an analgesic devoid of opioid side effects with effective potency is always looked for. Research for newer methods of providing analgesia made advent of cryoanalgesia, acupuncture, transcutaneous nerve stimulation etc but they are technically difficult and require special equipment’s and results are not very promising. Nerve plexus blocks or individual nerve blockscould be effective and excellent method of providing post-operative analgesia. However, they require technically expert. An alternative may be the use of incisional infiltration of local anaesthetic for post-operative pain relief. This has experienced renewed popularity and has been viewed as a new technique for preemptive analgesia. This was first suggested by Crile (Bonica) in 1950. In 1971 Moore7 showed that bupivacaine hydrochloride as a reliable drug for local infiltration. Recently, peripheral mechanism of nociception are being studied extensively, the centre of attention being afferent nerve terminals and its surroundings. It is interesting to study the modifications of the response of tissue injury at the afferent nerve terminals by locally infiltrated analgesics. There is a possibility that local anaesthetics might have a profound affect if present in high concentration at the site of injury. Local anaesthetic infiltration blocks the transmission by damaged tissue by blocking sodium voltage channels within the nerves. They are involved in the inflammatory responses like lymphocyte and granulocyte function, platelet aggregation, release of histamine, phospholipase A2 and superoxide. Local anaesthetic interferes with these changes and has effects on hyperalgesia and post-operative pain. Studies by Partridge etal8, Tverskoy et al9, Chester et al10, Patel et al11 have provided substantial data in this regard. Our study was conducted a study in fifty patients of both sexes ranging from twenty to fifty years and belonging to ASA grade I and II undergoing lower abdominal surgeries under general anaesthesia. Patients were randomly divided into two groups: Group I (Pre-incisional infiltraion group) received 20 ml of 0.25% bupivacaine at the proposed site of skin incision Surgery was started 10 minutes after infiltration. And Group - II (Post – incisional infiltration group) received 20 ml of 0.25% bupivacaine before skin closure. The evaluation of pain is frequently complex because pain is a perception rather than a sensation. Hewer and Keel12 in 1948 first described the technique of pain score for assessment of the efficacy of the various forms of analgesia and it has been used extensively since then. As pain is entirely a subjective sensation visual analogue scale has found to be more sensitive, accurate and consistent than fixed interval scale (Joyce 1975).13So we used visual analogue scale. Inj. Diclofenac sodium 75mg was given intramuscularly when patient demanded or developed intolerable pain. His VAS score and time of first analgesic requirement was noted. Thus, the time of analgesic requirement was taken as duration of analgesia. However once the patient received analgesic supplementation, his VAS score was taken only to give subsequent doses of analgesic and not considered for measuring duration of analgesia. Table No.2 shows the severity of pain (VAS) in both the groups. At 6 hours 100% of patients of both group had no pain or mild pain. By 8 hours. 72% of patients of group II had moderate pain, while 100% of patients of group I had mild pain (P <0.05). At 10 hours, 72% of patients of group II had moderate pain, while only 48% of patients of group I had moderate pain (P <0.05). At 20 hours 20% of patients of group-l had mild pain while 20% of group-II had severe pain (P <0.05) and remaining 80% of both groups had moderate pain. At 24 hours, 100% of group-l patients had moderate pain, while in group-II, 52 % of patients had moderate pain and 48% had severe pain (P <0.05). At 8 hours, 72% of patients of group-II had received analgesic supplementation. By 10 hours only, 48% of patients of group-l had received analgesic supplemental. By 16 hours all patients of group-II had received analgesic supplementation. Thus, pre-incisional infiltration of bupivacaine is more effective for post-operative pain relief and the severity of pain is significantly less than that of post-incisional infiltration of bupivacaine. Duration of postoperative analgesia was approximately 9.6 ± 1.1 hours in group-l and 8+08 hours in group-II (Table no.3). By applying unpaired t test, it was found that the difference between the two groups is statistically significant Thus pre-incisional infiltration of bupivacaine prolongs the duration of post-operative analgesia significantly than post- incisional infiltration of bupivacaine. Total amount of analgesic consumption was 1.5 ± 0.34 doses of Diclofenac sodium in group-l and 2.4 + 0.3 in group-II patients (Table No.3) Thus, the difference between the two groups is statistically significant. Thereby we can say that pre-incisional infiltration of bupivacaine decreases total amount of analgesic required for post-operative pain relief as compared to post – incisional infiltration of bupivacaine. Mean vital parameters of both groups were studied in the postoperative period (Table No.4) Statistically significant increase in the vital parameters seen at 8. 16, and 24 hours in group-ll patients while in group- l patients this increase in vital parameters was observed at 10 and 24 hours. This coincides with the onset of pain. No side effects like toxicity, hypersensitivity or wound infiltration were observed in any group. Kingsnoth et al (1979)14 in their study entitled “study of evaluation of dextran with local anaesthetic for short stay inguinal herniorrhaphy showed that preincisional infiltration of 0 25% of bupivacaine produced pain relief for almost 10 hours. Our study had a post-operative analgesia period of 9.6 in pre-incisional infiltration group which is comparable with the results.Wall15 (1988) proposed that pre-emptive pre-incisional analgesia has prolonged effects that outlasts the presence of the drug. According to him, analgesia given before the nociceptive stimulus is more effective than that given after the nociceptive stimulus. Barthody J. et al'"’ (1994)16 showed that pre-incisional infiltration of 0.25% bupivacaine was associated with early mobilization and lower pain scores as compared with no infiltration group in patients posted for inguinal herniorrhaphy Morisaki'- (1996)17 found that wound infiltration with lidocaine prior to surgical incision reduced both post-operative pain and the requirements for supplemental analgesics following haemorrhoidectomy under spinal anaesthesia. Erickson-Mjoberg et al (1997)18, proved that pre-operative subcutaneous infiltration of bupivacaine at the site of incision significantly reduced the post-operative consumption of morphine. Ellen Eglerson(1992)19 compared the efficacy of pre-incisional wound infiltration with 1% of 40ml of lignocaine with post-incisional infiltration in cases of elective herniotomy. Demand for additional post-operative analgesic occurred earlier in the post-incisional group (165 minutes) than in the pre-incisional group (225 minutes). Fewer patients in the pre-incisional group received morphine than in the post- incisional group. Thus he concluded that pre-incisional infiltration is more effective method of providing post-operative analgesia than post-incisional infiltration. He concluded that it could be due to better local absorption of local anaesthetic after injection into the intact tissue rather than into the incised wound and prevention of peripheral hypersensitivity and/or central nervous system hyper excitability. In our study also we found similar results. But as compared to the above study we had prolonged duration of post-operative analgesia (around 9.6 hours). This might be because we used bupivacaine infiltration and the action of bupivacaine is longer than lignocaine. Thus, from one study we conclude that pre-incisional infiltration of bupivacaine is an effective method of providing post-operative analgesia, and it decreases the total analgesic requirement in the first 24 hours of post-operative period as compared to post-incisional infiltration of bupivacaine. Pre-incisional infiltration is a method of choice as it is easy, safe and effective requiring less monitoring. It helps to maintain the normal physiology, since good pain relief allows early ambulation. So, we strongly advocate use of pre-incisional infiltration of bupivacaine for post-operative pain relief. Table-1: Demographic Characteristics
Using Chi-square test we found no significant difference (P >0.05).
Table 2: comparison of severity of pain in pre-incisional (group i) and post-incisional (group-ii) infiltration group at different time interval
This table shows the comparison of severity of pain in both the groups at different time interval. Using Chi-square test, we found a significant difference in group I and group II (P <0 05). It can be seen that the severity of pain was much less in pre-incisional infiltration group. (Group I) as compared to the post-incisional infiltration group (Group-II) Table-3: Duration of Analgesia and Total analgesic requirement in post-operative period
Using unpaired ‘t’ test, the difference between two groups is statistically significant (P <0.05).
Table 4: Mean vital parameter of patients in the post-operative period
This table shows that using unpaired ‘t’ test, there is a significant increase in the vital parameters after 10 & 24 hours in group I patient (P <0 05) Significant increase in vital parameters at 8, 16 and 24 hrs. in group II patients. (P <0.05).
Figure-1: Comparison of duration of surgeries
CONCLUSION We can say that pre-incisional infiltration as well as post- incisional infiltration of bupivacaine is a safe, easy and effective method of post-operative analgesia. But the duration of analgesia and the requirements of supplemental analgesic in the post-operative period is significantly lower in the pre-incisional infiltration group. Our study confirms the belief that pre-incisional surgical wound infiltration facilitates a smooth and pain-free transition into post-operative period.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home