Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 2 - November 2018
Uthkala Bhaskar Hegde1, N Gangadharaiah2*, Arjun N R3
1Associate Professor, Department of Anesthesia, MVJ Medical College and Research Centre, Hoskote, Bangalore, Karnataka, INDIA. 2Assistant Professor, Department of Anesthesia, Sapthagiri institute of medical Sciences and Research Centre, Bangalore, Karnataka, INDIA. 3Senior Resident, Department of Neuroanaesthesia and Neurocritical care: National Institute of Mental Health and Neuro-Sciences, Bangalore, INDIA. Email: ngangadharaiah25@yahoo.com
Abstract Background: Spinal anaesthesia is at low cost, a surgery of up to two hours duration can be performed. The greatest challenge of the technique is to control the spread of the local anaesthetic through the cerebrospinal fluid (CSF) in order to produce a block that is adequate for the proposed surgery without producing a needless extensive spread. Aims: The present study was aimed to assess the facilitatory effects of intravenous Dexmedetomidine premedication on spinal anaesthesia and analgesia in patients undergoing lower limb surgeries with 0.5% Hyperbaric Bupivacaine. Materials and methods: A one year prospective, double blind, randomized placebo controlled trial. Patients undergoing elective lower limb orthopaedic surgeries under spinal anaesthesia at tertiary care hospital from January 2014 to December 2015.A total of 60 patients divided into two groups using computer randomization. Results: No biphasic change in heart rate or mean arterial pressure or significant cardiovascular variability was observed after administration of Dexmedetomidine. Patients in Dexmedetomidine group had a significantly faster onset of motorblockade(3.64±0.75) compared to placebo and faster onset of sensory blockade (66±44.14 seconds) compared to placebo(129.6±102.4seconds) and , higher level of highest sensory block level achieved (T4.8±1.52) as compared to placebo group (T5.8±0.96).Total Duration of Motor Block was significantly prolonged in group D (256.44±53.10minutes) compared to group P (231.16±32.2minutes).Total Duration of Sensory Block in Dexmedetomidine group (234.34±47.82minutes) was significantly longer than placebo group (141.66±30.20minutes). Time to first request for post operative analgesia was significantly longer in group D (270.17±41.57) when compared to group P (155.73±23.39). Excessive sedation (Ramsay sedation score > 4) was observed in only one patient in Dexmedetomidine group. Even with excessive sedation (score of more than 4), the oxygen saturation remained comparable to the placebo group. Conclusion: Single dose of intravenous Dexmedetomidine given as premedication, prolongs the duration of sensory and motor blockade of bupivacaine-induced spinal anaesthesia. It also prolongs the time to first request for analgesia and provides conscious sedation without ventilatory depression and maintains good hemodynamic stability. Key Word: dexmedetomidine, spinal anaesthesia.
INTRODUCTION Spinal anaesthesia remains a popular technique used for surgery to the lower limbs, abdomen, pelvis and providing fast onset and effective sensory and motor blockade. The advantages of spinal anaesthesia have been well established and widely accepted. Current usage of this technique is waning in the developed world, with epidural analgesia or combined spinal-epidural anaesthesia emerging as the techniques of choice where the cost of the disposable 'kit' is not an issue. However spinal analgesia is the mainstay of anaesthesia in developing countries, excluding the major centres. At a low cost, a surgery of up to two hours duration can be performed. The greatest challenge of the technique is to control the spread of the local anaesthetic through the cerebrospinal fluid (CSF) in order to produce a block that is adequate for the proposed surgery without producing a needless extensive spread. 1 Administration of a spinal anaesthetic to higher levels may affect the ability to breathe by paralysing the intercostal respiratory muscles, or even the diaphragm in extreme cases (called a "high spinal", with which consciousness is lost), as well as the body's ability to control the heart rate via the cardiac accelerator fibres. Also, injection of spinal anaesthesia higher than the level of L1 can cause damage to the spinal cord, and is therefore usually not done. Subarachnoid block is a safe, inexpensive and ‘easy-to-administer’ technique which also offers a high level of post-anaesthesia satisfaction for patients.1 The risk of general anaesthesia including mishaps due to airway management are avoided in patients having an irritable airway (bronchial asthma or allergic bronchitis), anatomical abnormalities which make endotracheal intubation very difficult (micrognathia), in borderline hypertensives where administration of general anaesthesia or endotracheal intubation can further elevate the blood pressure, and procedures performed in geriatric patients. Bupivacaine, an amino amide group of local anesthesia is most widely used drug for spinal anaesthesia currently. Different agents, like epinephrine, phenylephrine, adenosine, magnesium sulfate and clonidine, have been used as adjuncts to local anaesthesia for prolonging the duration of spinal analgesia via the intrathecal route. Alpha 2 Agonists produce diverse responses, including analgesia, anxiolysis, sedation, and sympatholysis, each of which has been reported in the treatment of surgical and chronic pain patients and in panic disorders as well. Recently, the Food and Drug Administration registered two novel alpha 2- adrenergic agonists Clonidine and Dexmedetomidine.4 Dexmedetomidine is a highly selective and potent alpha 2 agonist (1620 :1 alpha 2: alpha 1), and is seven to ten times more selective for alpha 2 receptors compared to Clonidine, and has a half-life of 2 to 3 hours. Dexmedetomine is known to induce sedation, analgesia, decrease anaesthetic drug requirement and improve perioperative haemodynamics by attenuating blood pressure and heart rate responses to surgical stimulation, and protection against perioperative myocardial ischaemia. It provides sympathoadrenal stability and suppresses renin angiotensin activity. Supplementation of bupivacaine spinal block with a low dose of intrathecal Dexmedetomidine produces a significantly shorter onset of motor and sensory block and a significantly longer sensory and motor block than bupivacaine alone without any significant hemodynamic instability or sedation.2 Although a synergistic interaction between intrathecal Dexmedetomidine and local anesthetics has been observed in previous studies,7there is further need for study on the effects of intravenous Dexmedetomidine premedication on the onset, duration of sensory and motor block, and analgesia during spinal anaesthesia. Hence the present study was conducted to assess the effects of intravenous Dexmedetomidine on spinal anaesthesia and analgesia in patients undergoing elective lower limb orthopaedic surgeries.
MATERIALS AND METHODS A one year prospective, double blind, randomized placebo controlled trial. The present study was conducted in tertiary care hospital attached to PES Institute of medical science and research. during the period of January 2014 to December 2015. Patients undergoing elective lower limb orthopaedic surgeries under spinal anaesthesia at tertiary care hospital attached to PES Institute of medical science and research. A total of 60 patients divided into two groups using computer randomization. Based on the results of previous study and standard statistical formula, time for sensory two dermatome regression for the two drugs was taken to determine the sample size. The values were 261 ± 35 minutes for Dexmedetomidine and 165 ± 31 minutes for control group. However, for the sake of consistent results ‘n’ was taken as 30 that is, a total of 60 patients divided equally into two groups namely group D and P by using computerized randomization. Patients were randomly allocated into one of the two groups by computer generated randomization that is, Group D (n=30) Patients received Dexmedetomidine 0.5 μ g/kg over 15 minutes using infusion pump 20 minutes prior to SAB. Group P (n=30) Patients received 0.1 mL/kg normal saline over 15 minutes using infusion pump 20 minutes prior to SAB. Inclusion Criteria: Patients undergoing elective lower limb orthopaedic surgeries lasting 60 to 240 minutes. Patients with age between 20 to 60 years, Height between 140 to 165 cms, Weight between 40-60 kgs and Patients with ASA Grade I and II. Exclusion: ASA GRADE III and IV, Known allergy to Bupivacaine, History of bleeding diathesis, Infection at the site of spinal needle insertion, Severe spinal abnormalities like spina bifida, meningocele. On treatment with alpha adrenoreceptor antagonists. Use of any opioid or sedative medications in the week prior to surgery, a history of alcohol or drug abuse. Pre-existing neurological deficits in the lower extremities, and cardiovascular, respiratory, neurological, psychological, hepatic, or renal disease. All the patients fulfilling selection criteria were explained about the nature of the study and intervention and a written informed consent was obtained from all the patients before enrollment. After the enrollment, demographic data such as age and sex were recorded and patients were asked for the history. Pre anaesthetic evaluation, General physical examination, systemic examination was carried out. Routine investigations such as haemogram, blood group, bleeding time, clotting time, prothrombin time, activated partial thromboplastin time, International Normalized Ratio (if the patient was on anticoagulant therapy), electrocardiogram, Chest X-ray if required were done and the data was recorded on a predesigned and pretested proforma. Procedure: On the day of surgery Pre anaesthetic evaluation was done to ensure no fresh changes or fresh findings are present compared to last visit, Status of nil by mouth (NBM) was confirmed. Patient was taken in pre anaesthetic room. Monitors like, ECG, NIBP, Pulse oximetry were applied. Two IV lines were secured with appropriate IV canula and 500 ml of crystalloids were started in one line. The other line was used for study drug infusion. Heart rate, MAP, SpO2 using pulse oximeter was monitored before, during and after the surgery. The study drug in the prefilled coded 20 ml syringe was started 20 minutes before administering spinal block, using infusion pump at the rate of 0.1 mL/kg body weight over 15 minutes as a single dose. Dexmedetomidine was prepared in a dilution of 5 μg/ml of NS. The code number of the study drug syringe was noted down in the proforma. Dexmedetomidine was given in a dose of 0.5 μg/kg. After infusion patient shifted to OT with the monitors. Five minutes after the end of the infusion, under strict aseptic precautions a 25G Quinkes spinal needle was inserted in L3-L4 intervertebral space, with patient in sitting position and operation table kept flat. After confirming free flow of CSF, 3 ml of 0.5% Hyperbaric Bupivacaine was injected into the subarachnoid space. Patients received Oxygen 4 L/min via face mask after approximating them to surgical position. The patient and the anesthesiologist were blinded to the treatment group, and all recordings were performed by an anesthesiologist blinded to group allocation. Baseline Haemodynamic parameters was noted, Intraoperatively HR, BP and SpO2 were measured and noted. The vitals were monitored every 15 mins till the end of the surgery. Hypotension was defined as a decrease in systolic blood pressure by 30% from baseline, or a systolic blood pressure lower than 90 mm Hg and was treated with incremental doses of intravenous ephedrine (6 mg) and a bolus administration of 250 ml lactated Ringer’s solution over 10 minutes. Bradycardia was defined as HR < 50 beats/min, and was treated with 0.6 mg of intravenous atropine. Following variables were noted: Onset of sensory blockade. Onset of motor blockade. The highest Level of sensory block achieved. Recovery time for Sensory blockade or Time for two Dermatome regression. Recovery time for motor blockade. Total duration of Motor blockade. Total duration of sensory blockade. Time to request for rescue analgesia Sedation score Statistical analysis Data obtained was coded and entered into Microsoft excel spreadsheet. The categorical data was expressed in terms of rates, ratios and percentage and continuous data was expressed as mean ± standard deviation (SD). The data was analysed by chi-square test, test of proportion, student’s unpaired ‘t’ test and Mann Whitney test. For A probability value (p value) of less than or equal to 0.05 was considered as statistically significant. RESULTS A total of 60 patients undergoing lower limb surgeries under spinal anaesthesia were randomly allocated into one of the two groups by computer generated randomization that is Group D (n=30) Patients received Dexmedetomidine 0.1 mL/kg [0.5 μ g/kg] over 15 minutes using infusion pump 20 minutes prior to SAB. Group P (n=30) Patients received 0.1 mL/kg normal saline over 15 minutes using infusion pump 20 minutes prior to SAB. Table 1: Demographic Distribution
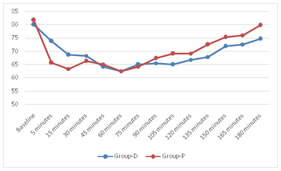
In group D, most of the patients (40%) were aged between 31 to 40 years, The mean age in both the groups had comparable demographic characteristics (p=0.366).Male to female ratio of 0.58:1, suggesting both the groups had comparable demographic characteristics (p=0.405). The mean height (p=0.234) and mean weight in in both the groups were comparable. In group D, 80% patients were ASA Grade I and 20% were ASA Grade II. In group P 86.6% patients were ASA Grade I and 13.33% were ASA Grade II, suggesting that ASA Grades in both groups were comparable (p=0.488). Figure 1: Distribution of heart rate in groups The mean heart rate at 5 minutes was significantly higher (p=0.02) in group-D compared to group P. Similarly, the mean heart rate at 15 minutes in group D which was significantly higher (p=0.04) compared to group P, suggesting a steeper fall from the baseline in group P compared to a gradual fall in group D.The mean heart rate at 105 minutes, 135 minutes and 150 minutes in group P was significantly higher (p=0.02, p=0.02 and p=0.03 respectively) than group D suggesting a steeper rise in heart rate in group P.At the end of 180 minutes, the mean heart rate in group P was significantly higher (p=0.003) than in group D. Thus, both the fall and the subsequent rise in mean heart rate in group D was more gradual as compared to the steep fall and rise in group P, as seen in the graph. Figure 2: Haemodynamic parameters – Mean arterial pressure
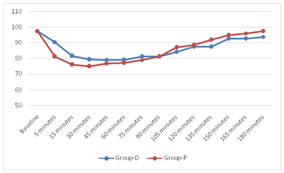
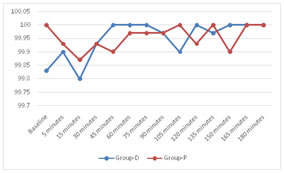
The MAP at 5 minutes was in group D which was significantly higher (p=0.01) compared to in group P, suggesting a greater fall from the baseline in group P compared to group D. The MAP at 135 minutes, 165 minutes and 180 minutes in group D was significantly lower (p=0.01, p=0.05 and p=0.04 respectively) than group P suggesting a steeper rise in MAP in group P. Both the fall and the subsequent rise in mean heart rate in group D was more gradual as compared to the steep fall and rise in group P, as seen in the graph. Figure3: Haemodynamic parameters – Oxygen saturation The oxygen saturation in both the groups was found to be comparable at all time intervals.
Table 2: Use of Atropine and ephedrine
The atropine-requiring bradycardia was more frequent in group D (20%) than in group P (13.33%) but was statistically insignificant (p=0.48).The ephedrine-requiring hypotension was more frequent in group P (23.33%) than in group D ( 6.67%), but was statistically insignificant.
Table 3: Sensory Block variables in study
The duration of onset of sensory blockade (Time taken to reach T10 level) in 53.33% of patients in Group D is between in 1 to 2 minutes (60 to 120 seconds) ,and less than 1 minute (60 seconds) in 46.67% of patients. The average mean time and standard deviation of onset of sensory blockade in Group D is 66±44.14 seconds. Most of the patients (30.00%) in group D had T4 level of the sensory block compared to T6 in group P (46.67%). Highest sensory block level achieved was higher (p=0.003) in group D (4.80 ± 1.52) than in group P (5.80 ± 0.96). The average mean time and standard deviation of onset of sensory blockade in Group P is 129.6±102.4 seconds. P value obtained is statistically significant. Table 4: Motor Block variables in study
The duration of onset of motor blockade(Time taken to achieve Bromage 3) in 56.67% of patients in Group D is between 4 to 5 minutes, and between 3 to 4 minutes in 44.33% patients. The average mean time and standard deviation of onset of motor blockade in Group D is 3.64±0.75. The duration of onset of motor blockade in 60% of patients in Group P is between 5 to 6 minutes, and between 4 to 5 minutes in 40% of patients. The average mean time and standard deviation of onset of motor blockade in Group P is 4.57±0.83 minutes. P value obtained is statistically significant.
Table 5: Recovery time of sensory block and motor block
The time for two segment regression of sensory block in 53.33% of patients from group D was between 121 to 180 minutes, and 60 to 120 minutes in 43.33% patients. The time for two segment regression of sensory block in 96.67% o f patients from group P was between 60 to 120 minutes, and less than 60 minutes in 3.33% patients. The recovery time of motor block in 86.67% of patients from group D was between 121 to 180 minutes, and 181 to 240 minutes in 13.33% patients. The recovery time of motor block in 80.0% of patients from group P was between 121 to 180 minutes, and 60 to 120 minutes in 20.00% patients. P value obtained is statistically significant. Table 6: Showing average mean time in study
Time of onset of sensory block in group D is lesser compared to group P and is statistically significant(P<0.001).The Time of onset of motor block in dexmedetomidine group is lesser compared to placebo group and is statistically significant(P<0.0001). The total duration of sensory and motor block in dexmedetomidine group is prolonged compared to placebo group and is statistically significant (P<0.001). Time to regression to Bromage scale 2, was significantly prolonged (p<0.001) in group D, in comparison with group P. Time for sensory regression of two dermatomes in Dexmedetomidine group, was significantly longer (p<0.001) than placebo group . Time to first request for post operative analgesia was significantly increased (p<0.001) in group D, in comparison to group P.
Table 7: Time at request for first post operative analgesia
P=<0.001 The time to first request for post operative analgesia in 20.0% of patients in group D was between 181 to 240 minutes, and 241 to 300 minutes in 53.33% patients. The time to first request for post operative analgesia in 86.67% of patients from group P was between 121 to 180 minutes, and 181 to 240 minutes in 6.67% patients. All patients in group P required rescue analgesic in less than 240 minutes whereas 20.00% patients in group D requested for rescue analgesia after 300 minutes.
Table 8: Ramsay sedation scores
In the present study more than or equal to four Ramsay sedation scores were noted in 13.33% patients in group D whereas, all the patients (100%) in group P had Ramsay sedation scores of 2.
DISCUSSION Alpha (α)-2-Adrenergic receptor (AR) agonists have been the focus of interest for their sedative, analgesic, perioperative sympatholytic, anesthetic- sparing, and hemodynamic-stabilizing properties. Dexmedetomidine, a highly selective α2AR agonist with a relatively high ratio of α 2 / α 1-activity (1620:1 as compared to 220:1 for clonidine), possesses all these properties but lacks respiratory depression62,63 making it a useful and safe adjunct in diverse clinical applications. In the present study females were more than males in group D (26.67% vs 73.33%) and group P (36.67% vs 63.33%) with male to female ratio of 0.36:1 and 0.58:1 respectively (p=0.405). The mean age in group D was 38.43 ± 10.93 years and in group P was 36.07 ± 9.12 years (p=0.366) suggesting equal distribution of sex and age in both the groups. The mean height in group D was 155.20 ± 6.26 cms and in group P it was 157.00± 5.52 cms (p=0.234 .The mean weight in group D was 52.27 ± 5.06 kgs and in group P it was 53.10 ± 5.23 kgs (p=0.535) In group D, 80% of patients were scheduled for surgery under ASA Grade I and 20% with ASA Grade II. In group P 86.6% patients had ASA Grade I and 13.33% had ASA Grade II status (p=0.488). Hence both the groups were comparable in terms of height, weight and ASA grade. 1. Haemodynamic parameters a. Heart rate Previous studies done by Arain SR et al 3 2002 and Aantaa R et al4, 1991,and meta analysis on intra venous dexmedetomidine on spinal anaesthesia by Abdullah et al52013 found 3.7 fold time increase in incidence of bradycardia support the finding that the bradycardia effect of dexmedetomidine is long lasting when used as a premedication drug. The lower HR could be explained by the decreased sympathetic outflow and circulating levels of catecholamines that are caused by Dexmedetomidine,as mentioned in studies conducted by Virkkila M et al6 1994. In the present study mean heart rate at 5 minutes (73.80 ± 13.38 bpm vs 65.63 ± 12.45 bpm; p=0.02) and at 15 minutes (68.63±10.30 vs 63.47 ±8.70 bpm; p=0.04) was significantly higher in group D compared to group P suggesting a steeper fall from the baseline in group P compared to a gradual fall in group D. The heart rate in both groups was found to be comparable at 30, 45, 60, 75, 90 minutes (p>0.05). In both the groups heart rate reached the lowest value at approximately the same time that is around 60 minutes and comparable in both the groups (p=1.00). The mean heart rate at 105 minutes, 135 minutes and 150 minutes in group P (69.17±7.15, 72.53±8.44, and 75.40±5.83 respectively) was significantly higher (p=0.02, p=0.02 and p=0.03 respectively) than group D (65.03±5.85, 67.93±6.44, and 71.90±6.55 respectively) suggesting a steeper rise in heart rate in group P. At the end of 180 minutes, the mean heart rate in group P was significantly higher than in group D (79.80±7.59 vs. 74.67±5.21; p=0.003). Thus, both the fall and the subsequent rise in mean heart rate in group D was more gradual as compared to the steep fall and rise in group P. Hence our study doesn’t concur with the above mentioned study as the drug dexmedetomidine was given intravenous bolus in the studies done by above authors,where as in our study it was given slow intravenous infusion. b. SBP, DBP and MAP (Intraoperative hypotension and biphasic cardiovascular response i.e. initial increase in MAP and decrease in HR, followed by decrease in MAP and persistent decrease in HR) Previous studies by Aantaa R et al 19914 and Hogue CW et al7 2002 studies have shown that the hypotensive effect of Dexmedetomidine persists in the intraoperative as well as in the postoperative period. In our study the MAP at 5 minutes was significantly higher in group D (90.73±14.65 vs 81.22±11.64; p=0.01) compared to group P, suggesting a greater fall from the baseline in group P compared to group D. The MAP in both groups was found to be comparable at 15, 30, 45, 60, 75, 90, 105, 120 minutes (p>0.05). The MAP in both the groups reached the lowest value at approximately at 45 minutes. The lowest MAP recorded was 79.08±5.34 in group D and 77.08±9.73 in group P and the MAP at 135 minutes, 165 minutes and 180 minutes in group D (87.51±5.58, and 92.78±6.75, and 94.02±7.19 respectively) was significantly lower (p=0.01, p=0.05 and p=0.04 respectively) than group P (91.91±7.11, 96.22±6.49, and 97.56±5.42 respectively) suggesting a steeper rise in MAP in group P. Both the fall and the subsequent rise in MAP in group D was more gradual as compared to the steep fall and rise in group P. At the end of 180 minutes, the mean HR and MAP in group P was significantly higher than in group D, probably due to the prolonged analgesic effect of Dexmedetomidine. Hence our study doesn’t concur with the above mentioned study as the drug dexmedetomidine was given intravenous bolus in the studies done by above authors, where as in our study it was given slow intravenous infusion. c. Oxygen saturation In the present study, oxygen saturation in both the groups was found to be comparable at all time intervals. A study F.N.Kaya et al8 2010 observed no respiratory depression in any patient and respiratory parameters (respiratory rate, SpO2, and Et-CO2) remained within normal limits throughout the procedure. Another studyMahmoud M Al-Mustafa et. Al9 2009, reported that the oxygen saturation was higher than 95% in all patient in the two groups either in the intraoperative or in the PACU time. Previous studies,conducted by Lee et al 102014,Gupta et al11 2014,Abdallah et al 5 2013,Dinesh et al 122014, also show similar results. Hence our study results with respect to oxygen saturation is concurrent with the results of the study mentioned above. 2. Block characteristics. a) Time of Onset of sensory and motor blockade Studies conducted by Dinesh et al 12 2014,F.N.Kaya et al 8 2010, Mahmoud M Al-Mustafa et. al92009, where dexmedetomidine shortened the onset time by 30 to 60 sec which is comparable to the present study. Reddy et al13 2013 study has shown onset of sensory blockade and motor blockade was significantly faster with p value of less than 0.001 for both sensory and motor blockade In the present study time of onset of sensory blockade and motor blockade in dexmedetomidine group is 66±44.14seconds and 3.64±0.75 minutes compared to 129.6±102.4seconds and 4.57±0.83 minutes in placebo group which is statistically significant as the p value obtained is >0.001 for sensory(0.0008) and motor blockade(0.0168).The results of the present study is in concurrence with study conducted by Reddy et al13.The faster onset of sensory block in our study and other studies by above author is probably due to alpha 2 receptor activation induced inhibition of nociceptive impulse transmission. b) Highest level of sensory block achieved Previous studies, conducted by upadhyay et al14 2015, Lee et al 10 2014,Gupta et al 11 2014,Abdallah et al 52013,Reddy et al 132013, Dinesh et al 122014, F.N.Kaya et al 82010,Mahmoud M Al-Mustafa et al 92009 showed that higher level of sensory block was achieved in dexmedetomidine group.The results of the present study is in concurrence with the above studies. Most of the patients (30.00%) in group D had T4 level of the sensory block compared to T6 in group P (46.67%). Sensory block level achieved was higher in group D (4.80 ± 1.52) than in group P (5.80 ± 0.96) with a p value of 0.003 which is statistically significant. c) Mean recovery time of sensory and motor block Previous studies, conducted by Upadhyay et al 142015, Lee et al 102014,Gupta et al 112014,Abdallah et al 52013,Reddy et al 132013, Dinesh et al 122014,F.N.Kaya et al 82010,Mahmoud M Al-Mustafa et al 92009 showed time required for two segment regression is significantly prolonged in dexmedetomidine group. In the present study the mean recovery time for sensory (i.e the time for sensory regression of two dermatomes) block in dexmedetomidine group was 165.67±19.77 compared to 132.33± 9.35 in placebo group , and the p value derived is less than 0.001which is statistically significant .Hence our study results concur with the studies mentioned above. In the studies conducted by F.N.Kaya et al82010, showed that single dose of preoperative dexmedetomidine doesnot prolong the duration of motor regression, Reddy et al 132013,also observed similar findings.our study doesnot concur with the above studies and the possible theory that could explain it was, effect of clonidine on motor blockade was concentration dependant and the same theorey might explain this phenomenon with dexmedetomidine as well . Mahmoud M Al Mustafa et al9 2009, observed an increase in duration of motor regression.In the present study Time to regression to Bromage scale 2, was significantly prolonged in group D compared to group P ((128.00±20.07 vs 79.00±11.55; p<0.001). These results are in concurrence with the results of the studies mentioned above. d) Total Duration of sensory and motor block Previous studies, conducted by upadhyay et al 142015, Lee et al 102014,Gupta et al 112014,Abdallah et al 52013,Reddy et al 132013, Dinesh et al 122014,F.N.Kaya et al 82010,Mahmoud M Al-Mustafa et al 92009 ,shows a significant prolongation in the duration of sensory blockade . In our study the average total duration of sensory blockade in dexmedetomidine group is 234.34±47.82 minutes compared to 141.66±30.20 minutes in placebo group ,the p value obtained in our study is less than 0.0001 which is statistically highly significant .Hence our study results is in concurrence with the above studies with respect to significant prolongation of sensory blockade in dexmedetomidine group. Based on the present and previous studies, the effect of Dexmedetomidine is not dependent on the route of administration. In a study Konakci et al 152008, authors found that Dexmedetomidine may have a harmful effect on myelin sheath when administered epidurally. Hence an intravenous route promises a safer and effective adjunct to spinal anaesthesia. However, a drawback of Dexmedetomidine supplemented spinal block characteristics may be an increase in the duration of motor block, which may not suit ambulatory procedures. In the present study the average total duration of motor block in dexmedetomidine group is 256.44±53.10 minutes, compared to231.16±32.2 minutes in the placebo group, and the P value obtained in our study is less than 0.001 which is highly significant statistically. In the previous studies conducted by Reddy et al13 2013, F.N.Kaya et al 82010 there was no significant increase in total duration of motor blockade with dexmedetomidine as compared to clonidine or placebo group and the probable explaination is the mechanisim of motor block produced by alpha 2 agonist clonidine results in direct inhibition of impulse conduction in the large , myelinated A-alpha fibers. The 50% effective concentration measured to block motor fibers is approximately 4 folds that of small unmyelinated C fibers.This could explain the less prolonged motor block compared with sensory block, as conduction of motor nerve fibers were less inhibited than sensory nerve fibers at the same concentration of clonidine. A similar mechanisim can explain the prolongation of sensory block as compared with motor block in the dexmedetomidine group. 3. Time for request of first post operative analgesia Studies conducted by Upadhyay et al 14 2015, Lee et al 102014, Gupta et al 11 2014, Abdallah et al 5 2013, Reddy et al13 2013, Dinesh et al 122014, F.N.Kaya et al8 2010, Mahmoud M AL-Mustafa et al9 2009 where authors described the time to first request for rescue analgesia was more than 180 minutes in Dexmedetomidine group, which is significantly higher than saline or placebo group. They also observed that Dexmedetomidine reduced the analgesic requirement in the post operative period. The time to first request for post operative analgesia in our study was 20.0% of patients in group D was between 181 to 240 minutes, and 241 to 300 minutes in 53.33% patients. In group P among 86.67% of patients it was between 121 to 180 minutes, and 181 to 240 minutes in 6.67% patients. All patients in group P required rescue analgesic in less than 240 minutes whereas 20.00% patients in group D requested for rescue analgesia after 300 minutes. The mean time to first request for post operative analgesia was significantly increased in group D (270.17±41.57) when compared to group P (155.73±23.39) (p<0.001).Hence our results are consistent with the results obtained by above studies. 4. Sedation Dexmedetomidine was initially approved for short term sedation for patients in critical care. Dexmedetomidine being a sedative provides intra operative analgesia without causing respiratory depression. Adequate sedation intraoperatively can decrease the patients stress related to surgery and cause anxiolysis and provide better comfort for patient and surgeons . In the present study a Ramsay sedation score of more than 4, suggesting excessive sedation was noted in 3.33% patients in group D whereas, all the patients (100%) in group P had Ramsay sedation scores of 2 (p<0.0001). A score of 4 was noted in 10% patients in group D. It is important to note that even with excessive sedation (score of more than 4), the oxygen saturation remained comparable to the placebo group, suggesting Dexmedetomidine produces sleep, without ventilatory depression, making Dexmedetomidine a near ideal sedative. The sedation produced by Dexmedetomidine differs from other sedatives, as patients may be easily aroused and remain cooperative. Intravenous dexmedetomidine given as premedication during spinal surgery provides adequate intraoperative sedation without causing respiratory depression.The results observed in our study with respect to sedation without ventilatory depression is in concurrence with the results obtained by the study conducted by upadhyay et al14, Lee et al10 ,Gupta et al11, Abdallah et al5, Reddy et al13, F.N.Kaya et al8,Mahmoud M Al-Mustafa et al9. CONCLUSION REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home