Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 2 - November 2018
Regional anesthesia in patients with scoliosis - A single centre clinical experience in India
Koramutla Pradeep Kumar1*, G Jagadesh2
1Associate Professor, Department of Anesthesiology, Balaji Institute of Surgery Research and Rehabilitation for Disabled, Tirupati, (A.P), INDIA. 2Director, Department of Orthopaedics, Balaji Institute of Surgery Research and Rehabilitation for Disabled, Tirupati, (A.P), INDIA. Email: drpradeep9@gmail.com
Abstract Background of the study: Anesthesia in scoliotic spine is challenging because of the rotation of the vertebrae and indifferent spread of the drug following spinal blockade. The present prospective study was taken up to assess the safety of regional anesthesia and to assess the spread of 0.5% bupivacaine in moderate to severe kyphoscoliotic patients. Material and Methods: This study included 90 patients posted for lower limb orthopaedic soft tissue release procedures and divided into two groups i.e Group 1 with patients having Cobb’s angle<40 (n=52) while group 2 included patients with Cobb’s angle>40(n=38). Spinal anesthesia [Bupivacaine 2.5 ml(12.5mg)] was given with the patients positioned in the lateral with convexity of the spine to the lower side. After spinal anaesthesia, the patient was made supine with both the knees and hip flexed to correct the spinal curvature. Sensory level, motor blockade, onset of anaesthesia, duration and regression of sensory and motor blockade were assessed along with the spread of anaesthesia and achievement of spinal blockade. Results: The onset of sensory block was delayed(9.6 mins) in group 2 (Cobb’s angle>40) i.e when the curvature is more compared to group 1(7.2 mins) (Cobb’s angle<40) while the motor block was achieved earlier (5.6 mins) in group 2 patients (p<0.05) compared to group (6.4 mins). Time for 2 segment regression was faster (48 ± 28 min) in group 2 patients (p<0.05) compared to group 1 (52 ± 19 min). The quality of anesthesia, need for intra-operative sedation and satisfaction of the patients were adequate in both groups. Conclusion: Bilateral effective spinal blockade was achieved with flexion at the hips after giving spinal anesthesia thereby obliterating the spine curvature. With our experience of 90 cases, regional anesthesia can be safely given in moderate to severe scoliosis. Key words: Cobb’s angle; Scoliosis; Spinal anaesthesia; Regional anaesthesi
INTRODUCTION Kyphoscoliosis is a deformity of the costovertebral skeletal structures arising as a result of disruption of balance between structural and dynamic components of the vertebral column1. There is axial rotation of the vertebral bodies and spinous processes. Causes of scoliosis include congenital, neuromuscular, idiopathic, associated with syndromes like Marfan’s syndrome and secondary to poliomyelitis, tumours etc.2. The severity of the scoliosis is assessed by the Cobb’s method as recommended by the Terminology Committee of the Scoliosis Research Society. This involves three steps; first locating the superior end of vertebra, then the inferior end vertebra and finally drawing intersecting perpendicular lines from the superior surface of the superior end vertebra and from the inferior surface of the inferior end vertebra. The angle of deviation of these perpendicular lines from straight line is the angle of the curve. Anesthesia in the presence of spinal deformity such as scoliotic spine is challenging for many anesthesiologists because of the rotation of the vertebrae. Airway management is challenging in cases with involvement of the upper thoracic and cervical spine3. A defective gas exchange with or without decrease in oxygen diffusing capacity have been reported5,6. Scoliotic deformity significantly affects the respiratory mechanics with an early reduction in lung volume as a result of restrictive airway4. This can lead to respiratory failure, pulmonary hypertension and corpulmonale. Also, the severity of pulmonary and cardiovascular involvement increases with the increase in the Cobb’s angle. A study has shown an association of scoliosis with malignant hyperthermia in a patient who underwent a surgery for idiopathic scoliosis under general anaesthesia7. In our institute, the patients present for surgical correction of lower limb orthopaedic procedures for hip flexion contracture release (Soutters and knee release) and hamstring contracture release. Due to curvature of the spine, administering spinal anesthesia is very difficult in such cases. Also, there is indifferent spread of the drug following spinal blockade. With this background, the present prospective case-series analysis was taken up to identify the safety of regional anesthesia and assess the spread of 0.5% bupivacaine in moderate to severe kyphoscoliotic patients.
MATERIAL AND METHODS This prospective study was conducted on 90 patients of either gender or age group between 20-60 years belonging to ASA-I and II patients. All the patients were posted for lower limb orthopaedic soft tissue release procedures. Patients were divided into two groups based on the measurement of Cobb’s angle .Figure 1a Group 1 included patients with Cobb’s angle less than 40 (n=52) while group 2 included patients with Cobb’s angle more than 40 (n=38). Anaesthesia protocol Spinal anesthesia was planned for all the patients. Patients were positioned in the lateral with convexity of the spine to the lower side as shown in Figure 1b. L3-L4 space was palpated and with a 25 G spinal needle, Bupivacaine 2.5 ml(12.5mg) fixed dose is given to all the patients. After spinal anaesthesia, the patient was made supine with both the knees and hip flexed to correct the spinal curvature as shown in Figure 1d. This maneuver was done to partially counter the deformity of the spine thereby preventing the inadequate spread of the administered drug. Monitoring included electrocardiogram, pulse oximetry and non‑invasive blood pressure. Sensory level and motor blockade was assessed. Onset of anaesthesia (defined as the time between injection and achievement of the highest level of sensory blockade) was assessed. Duration and regression of sensory and motor blockade at5,10,15,30 minutes was also assessed. Sensory level was assessed by pinprick method while the motor blockade was assessed by reversed bromage score (3=complete paralysis, 2=movements of the foot only, 1=small motor block movement of the knee, 0=no paralysis). The spread of anaesthesia and achievement of spinal blockade [complete/partial] was assessed on both lower limbs. If the anaesthesia was inadequate, on either of the lower limbs, then sedation was given using ketamine 2 mg/Kg. All the surgical procedures were completed within 90-120 minutes. Statistical Analysis Data is expressed as mean ± standard deviation for continuous variables and as frequency (number [%]) for categorical variables. Independent samples T test was used to assess the difference between the two groups for continuous variables and chi square test for categorical variables. All statistical analysis were performed using Microsoft excel spreadsheets (Microsoft, Redmond, WA USA) and Statistical package for social sciences for windows version 16.0 (SPSS Inc., Chicago IL, USA). A ‘p’ value <0.05 was considered as statistically significant.
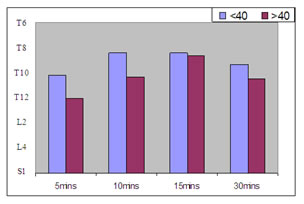
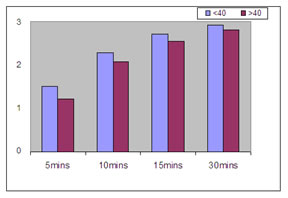
RESULTS The demographic characteristics of the subjects is shown in Table 1. There were no difference between groups in age, gender, weight, height or in the type and duration of surgery (p>0.05). Onset of sensory block is assessed by the time between the injection and achievement of the highest level of sensory blockade. This was achieved by pin prick method. In group 1 i.e. patients of Cobb’s angle < 40 the highest sensory level (T4-T6) was reached in 7.2 minutes compared to 9.6 minutes in group 2 patients (Cobb’s angle >40). This shows that the onset of sensory block is delayed when the curvature is more (Table 2, Figure 2). The onset of motor blockade was 6.4 minutes in case of group 1 patients (Cobb’s angle <40) compared to 5.6 minutes in group 2 patients (Cobb’s angle >40) (Table 2, Figure 3). This shows that the motor block is achieved earlier in group 2 patients (p<0.05). Time for 2 segment regression is defined as time elapsed from spinal injection to regression of sensory level by two dermatomes. In group 1 patients it was 52 ± 19 min and in group 2 patients it was 48 ± 28 min. This shows that regression is faster in Cobb’s>40 patients (p<0.05). Two patients in group 1 patients required ephedrine use after spinal induced hypotension, whereas five patients in group 2 patients required vasopressor ephedrine. The quality of anesthesia, need for intraoperative sedation and satisfaction of the patients were adequate in both groups (Table 3). Forty three patients (83%) in group 1 achieved complete bilateral equal spread of anesthesia whereas 25 patients (66%) in group 2 achieved equal spread of spinal anesthetic bupivacaine.
Table 1: Demographic and surgical data of the subjects
Table 2: Characteristics of spinal blockade
Figure 1: Positioning of the patient Legend Figure a: cobbs angle measurement; Figure b: curvature of spinous process after lateral positioning; Figure c: spinal needle position; Figure d: Hip flexion maneuver after spinal block Figure 2: Sensory level at different time intervals Figure 3: Motor block at different time intervals DISCUSSION Administration of anaesthesia in a patient with scoliosis is challenging. Moderately severe scoliosis may be associated with persistent unilateral analgesia and kyphosis frequently predisposes to an excessively high level of sensory block. These patients are unable to flex their spines making any approach technically more difficult. The presence of abnormal spinal curves makes the effect of posture on the distribution of a spinally administered drug difficult to predict8. Caution is required because excessively high levels of block, with respiratory insufficiency, have been reported. Other problems are of unsuccessful insertions and multiple attempts before successful insertion9. Lower doses of local anaesthetics may achieve higher than expected level of block with more incidence of hypotension. Patients with severe curves hyperbaric solution may pool in the dependent portion of the spine and results in inadequate block9. Since studies comparing the effectiveness of spinal anesthesia and dose requirements of local anaesthetics in severe kyphoscoliotic patients are lacking, we took up this study to assess the safety of regional anesthesia and also assess the spread of 0.5% bupivacaine in moderate to severe kyphoscoliotic patients posted for lower limb orthopaedic soft tissue release procedures. Patients were divided into two groups based on the measurement of Cobb’s angle. Group 1 included patients with Cobb’s angle (a measure of severity of kyphoscoliosis) less than 40 while group 2 included patients with Cobb’s angle more than 40. The Cobb’s angle is a radiological measurement made on an AP view x-ray of the spine to evaluate the severity of scoliosis. Surgical correction of scoliosis is indicated when the Cobb’s angle exceeds 50° in the thoracic spine and 40° in the lumbar spine. The rate of successful epidural placement varies depending on the level of fusion of the vertebrae10. In the present study the drug volume was fixed at 2.5ml (12.5) mg because CSF volumes are affected in severe scoliosis11. Onset of spinal block is more rapid in patients with Cobb’s angle <40. Level of anesthesia in our cases was 7.2. Kim et al.,7 observed the level of anesthesia to reach T6 after intrathecal injection after 7 minutes. In another study, Martin R et al.,12 observed the spread to reach a maximum upto T7 ± 2 upper levels with both isobaric as well as hyperbaric bupivacaine. The authors administered the drug to the patient placed supine with the operating table in a neutral position. The patients also received a subsequent injection of lidocaine 2% into the epidural space following spinal anaesthesia. However, the epidural effects of 2% lidocaine were found to be minimal. In scoliotic patients secondary to poliomyelitis, patients will have weakness of the paraspinal muscles and hence the patients were anesthesized in the lateral position with convexity towards the operating table. Time for 2 segment regression defined as time elapsed from spinal injection to regression of sensory level by two dermatomes was 52 ± 19 mins in group 1 patients compared to 48 ± 28 min group 2 patients. This difference was not found to be statistically significant. However, the regression was faster in patients with cobs angle >40. Martin R et al.12 observed similar findings in patients on hyperbaric bupivacine with 2 segment regression of 52 ± 28 mins. Two patients in group 1 patients required ephedrine use after spinal induced hypotension, whereas five patients in group 2 patients required vasopressor ephedrine. This shows that patients with more deviated spines are vulnerable to spinal induced hypotension. The quality of anesthesia, need for intraoperative sedation and satisfaction of the patients were similar in both groups. There was no significant difference in perioperative sedation requirement and patient satisfaction in both. To conclude regional anaesthesia is the safest approach, but technically challenging. This is the largest case series of anesthetic experience with scoliosis patients. Bilateral effective spinal blockade was achieved with flexion at the hips after giving spinal anesthesia thereby obliterating the spine curvature. With our experience of 90 cases regional anesthesia can be safely given in moderate to severe scoliosis.
REFERENCES
|
|
 Home
Home