Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
A comparative study of intrathecal dexmedetomidine and fentanyl as adjuvants to bupivacaine to provide prolonged postoperative analgesia
V Mashalkar Subhash1, B Ramadas2*, Ravi Kumar3, Mohammad Shakeeb Yusufi Attar4
1Associate Professor, 2Professor and HOD, Department of Anaesthesia, Navodaya Medical College, Raichur, Karnataka, INDIA. 3Professor, Department of Anaesthesia, DMWIMS, Meppadi, Kalpetta, Wayanad, Kerala, INDIA. 4Intensivist, United Hospital-Trauma and Critical Care Centre, Gulbarga, Karnataka, INDIA. Email: rknnese@gmail.com
Abstract Background and Objectives: Mixing adjuvants with hyperbaric bupivacaine for intrathecal injection is an practice since long time for reducing dose requirement of bupivacaine and prolongation of duration of action. Short acting liophilic opioid fentanyl and selective apha2 agonist dexmedetomidine is used to reduce dose requirement of bupivacaine and its adverse effects and also to prolong postoperative analgesia. The main objective of the study is to compare efficacy of intrathecal adjuvants i.e., dexmedetomidine and fentanyl with hyperbaric bupivacaine to assess postoperative analgesia and side effects Materials and Methods: This prospective, randomized, double blinded and placebo control study was carried out in a tertiary health care centre on 105 patients by randomly allocated into 3 groups and were assigned to receive one of the three intrathecal drugs i.e., Group D (n=35) received mixture of 0.5% hyperbaric bupivacaine (2.5ml) with Dexmedetomidine (5mcg) intrathecally, Group F(n=35) received mixture of 0.5% hyperbaric bupivacaine (2.5ml) with (25mcg) of fentanyl intrathecally and Group B received 0.5% hyperbaric bupivacaine (2.5ml) and 0.5ml normal saline intrathecally. All the solutions were made up to volume of 3ml in a 5ml syringe. Results: The duration of analgesia was significantly longer in Group D (545±61.94) compare to Group F (437.94±43.32) and Group B (263.97±22.88). Conclusion: Dexmedetomidine an adjuvant to bupivacaine (H) found to be very attractive alternative to fentanyl as it provides excellent postoperative analgesia. Key Word: Dexmedetomidine; Fentanyl; Bupivacaine; spinal anesthesia; postoperative analgesia.
INTRODUCTION Subarachanoid block is widely used method providing a fast onset and effective sensory and motor blockade. Subarachanoid block has definitive advantage that profound analgesia can be produced in large part of the body by relatively simple injection of small amount of local anaesthestic agent. Bupivacaine is the local anaesthetic most commonly used, although lidocaine (lignocaine), tetracaine, procaine, ropivacaine, levobupivicaine and prilocaine may also be used. In order to extend intraoperative analgesia into postoperative period a number of spinal adjuvants like opioids are added to improve the block quality and provide post-operative pain relief, examples include clonidine, morphine, diamorphine or buprenorphine.1 The potentiating effect of short acting lipophilic opioid fentanyl to hyperbaric bupivacaine improves the quality of intraoperative and early postoperative subarachnoid block. The addition of opioids to local anaesthetic solution have disadvantages, such as pruritus and respiratory depression. Dexmedetomidine, a highly selective a2-agonist, is under evaluation as a neuraxial adjuvant as it provides stable hemodynamic conditions, good quality of intraoperative and prolonged postoperative analgesia with minimal side effects. Food and drug administration (FDA) has approved Dexmedetomidine as a short time sedative for mechanically ventilated intensive care unit (ICU) patients. Based on earlier human studies, it is hypothesized that intrathecal 5 mcg dexemedetomidine would produce more postoperative analgesic effect with hyperbaric bupivacaine in spinal anaesthesia with minimal side effects. The disadvantage with spinal anaesthesia using bupivacaine alone is the relatively short duration of action, which means that an early analgesic intervention is needed in the postoperative period. Pedersen et al2, demonstrated that, although the incidence of abdominal pain decreased with increasing doses of bupivacaine (10-12.5 vs. 7.5-10 mg), almost one third of patients experienced pain. A Plethora of studies has shown that spinal opioids can provide profound postoperative analgesia with fewer central and systemic adverse effects than with opioids administered systemically. Segmental analgesia induced by spinal administration of opioids has been used successfully to treat intraoperative pain, postoperative pain, traumatic pain, obstetric pain, chronic pain and cancer pain. The addition of fentanyl to hyperbaric bupivacaine increases the intraoperative and early postoperative quality of subarachnoid block3 Alpha-2 agonists like dexmedetomidine, because of its ability to reduce sympathetic nervous system output from the central nervous system, acts as an antihypertensive drug. Preservative free dexmedetomidine, administered into the subarachnoid space (5mcg), produces dose- dependent analgesia and, unlike opioids, does not produce marked depression of ventilation, pruritus, nausea and vomiting or delayed gastric emptying. Dexmedetomidine exerts action on the descending inhibitory monoaminergic tracts, resulting in an antinociceptive effect. Dexmedetomidine produces analgesia by activating postsynaptic alpha2 receptors in the gelatinous substance of the spinal cord. By addition of lipophilic opioid and alpha-2 agonist to low dose local anaesthetic, it is possible to improve the quality of anaesthesia, increase the success of anaesthesia and better postoperative analgesia4 This study is designed to quantitatively examine the effects and side/ adverse effects of adding intrathecal dexmedetomidine and fentanyl to bupivacaine on the duration of onset, intraoperative haemodynamic stability, prolongation of block and recovery of sensory and motor block and postoperative analgesia.
MATERIALS AND METHODS After obtaining institutional ethical clearance and written informed consent from the patients, a clinical study was conducted on 105 patients of 18-50 years of age with ASA 1 and 2 grade undergoing elective lower limb and lower abdominal surgeries under spinal anaesthesia. Type of study: A Prospective, randomized, double blinded and placebo control study. Patients were randomly allocated into 3 intervention groups of 35 patients each and were assigned to receive one of the three intrathecal drugs i.e. Group D: To receive 0.5% hyperbaric bupivacaine 2.5ml + 5mcg Dexmedetomidine in 0.5ml of normal saline intrathecally.
Group F: To receive 0.5% hyperbaric bupivacaine 2.5ml + 25mcg fentanyl intrathecally. Group B: To receive 0.5% hyperbaric bupivacaine 2.5ml and 0.5ml normal saline intrathecally. All the solutions were made upto volume of 3ml in a 5ml syringe.
Exclusion criteria:
METHOD OF STUDY Pre-anaesthetic check up was carried out pre-operatively with a detailed history, general physical examination and systemic examination. Airway assessment and spinal column examination along with informed written consent were done. The following laboratory investigations were done in selected cases – Routine blood – Hb%, TC, DC, ESR, Bleeding time, Clotting time. Fasting blood sugar, Blood urea, Serum creatinine, Urine analysis, chest x-ray, ECG, HIV and HbsAg. PROCEDURE: After overnight fasting, patient was shifted to operating room; IV access was obtained on the dorsum of non dominant hand, with 18 gauge IV cannula and Ringer's lactate solution 500 mL was infused intravenously before the block. The monitors connected to the patient included non invasive B.P, pulse oximeter and ECG. Baseline PR, BP and RR, SpO2 were recorded. Under strict aseptic precautions, lumbar puncture was performed in left lateral position or sitting position by midline approach by using disposable Quincke spinal needle (26 G) at L3-L4 intervertebral space, after free flow of cerebrospinal fluid the study drugs were injected according to group and patients shifted to surgical position. Patients were monitored continuously using non invasive blood pressure, pulse oximeter and lectrocardiogram. After spinal anaesthesia, Oxygen (4L/min) by venture mask was given. Fluid therapy was maintained with lactated Ringer's solution (10mL/kg/hr). Vital parameters were observed and recorded. Assessment of sensory and motor blockade was done using hypodermic pin prick method along the midaxillary line and modified bromage scale respectively. Patients were observed for sedation and it was recorded by 6 point modified Ramasay sedation scale score.Post operative analgesia assessment was done using VAS every 4 th hourly for 24 hours. Rescue analgesic in the form of inj diclofenac sodium 75mg i.m will be given if VAS score is >4. Total amount of analgesic administered after operation, time to first analgesic dose and the occurrence of any intra or post-operative adverse events such as nausea, vomiting, itching, respiratory depression (RR<12/min), postural puncture headache or any adverse events will be documented. Outcomes: The primary outcome was duration of postoperative analgesia in minutes (time to first analgesic request). (b). postoperative pain scores (c). requirement of analgesia in post operative period and (d). possible dexmedetomidine and fentanyl side-effects STATISTICAL ANALYSIS: Selected data was subjected to analysis. The statistical analysis was done using SPSS (statistical package for social sciences) version 19.0 statistical analysis. Data are expressed as Mean and Median. Variable data (mean +/_sd) and median to be compared using ANOVA (analysis of variance). Where as categorical data to be compared using Chi square X2 analysis and Fishers Exact Test. A probability value (P) <0.05 was considered statistically significant.
RESULTS A population analyzed for study consist of 105 patients of 18-50 years of age with ASA 1 and 2 grade, posted for elective lower limb and lower abdominal surgeries under spinal anaesthesia during a study period of 15 months (1/12/15-28/2/17). as two patients were excluded from the study, one from group F (fentanyl + hyperbaric bupivacaine) and one from group B (only hyperbaric bupivacaine) which were converted into general anaesthesia to proceed for the surgery because of inadeqaute block. In a double blinded and random manner, patients were assigned to receive one of the three intrathecal drugs based on randomly allocated three study group based on random numbers by computer generated table. The comparative study of the three groups is as follows: Table 1: Sex wise distribution of cases in study groups
103 patients of either sex had participated in the study and all the three groups had predominantly male patients as compared to females. The comparison among the three groups revealed no statistically significant gender wise difference as P>0.05. Table 2: ASA grade wise distribution of cases in study groups
84.6% of patients in each of the study groups were accepted in ASA grade I and rest 15.53% of patients in each of the groups were accepted in ASA grade II. There was no statistically significant difference in ASA grades between the three study groups as P>0.05. Post-operative analgesia(number of times Inj Diclofenac sodium 75mg im equired/24hours): In post-operative period, the number of rescue analgesic doses of Inj Voveron 75mg is very less in number in Group D, like 35 patients required only 2 doses as compared to Group B, which required more than 3 doses in 34 patients respectively. Comparison between the three study groups were statistically significant as P<0.000.
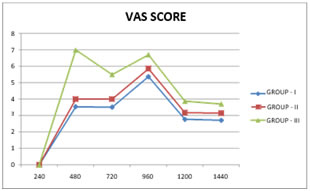
Graph 1: Post-operative parameters (Graph 1) Duration of requirement for first dose of Diclofenac(min): In Group D, mean time of first analgesic request for Inj Diclofenac sodium 75mg was 545±61.94, in Group F it was 437.94±43.32, in Group B it was 263.97±22.88 respectively. Comparison between the three study groups reveals a statistically significant difference as P<0.000. The time duration of total analgesia was highest for Group D followed by Group F and Group B. (graph 1) Comparison of time for voiding urination and by standing and walking: Comparison between the three study groups reveals a statistically significant difference as p<0.000, for time taken for voiding urine, standing and walking among the groups with patients in Group D taking longer time to void urine and for ambulation as compared to Group F and Group B. (graph 1) In present study, no adverse effects seen in Group D and Group F. 1 patient was reported for shivering and 5 patients were reported to have hypotension in Group B and required routine vasopressor and IV fluid intervention. No patient required any additional vasopressor therapy. VAS score was assessed for every 4th hourly interval in the study groups post-operatively. The mean value for VAS score in the post-operative period was statistically significant among the three study groups from 8th hour to 24th hour time interval as P<0.000. The VAS score were lowest for Group D as compared to Group F and Group B at all time in the entire post-operative period. We cannot calculate the P value for 240 min because all the values are zero. (Graph 2) Graph 2: Visual analogue scale
Comparison of sedation in the study groups: In all the three study groups, the modified Ramsay seadation score was found to be 2 and 3. None of the patient complaints excessive sedation or agitated behavior in any of the study groups.
The present study was carried out to study prolonged post operative analgesia effects of Dexmedetomidine with hyperbaric bupivacaine versus fentanyl with hyperbaric bupivacaine undergoing spinal anaesthesia in lower abdominal and lower limb surgeries. Our study designed consisted of 105 patients of 18-50 years of age with ASA 1 and 2 grade, were randomly allocated into 3 groups after informed consent. Group D: To receive 0.5% hyperbaric bupivacaine 2.5ml+5mcg Dexmedetomidine in 0.5ml of normal saline intrathecally. Group F: To receive 0.5% hyperbaric bupivacaine 2.5ml + 25mcg fentanyl intrathecally. Group B: To receive 0.5% hyperbaric bupivacaine 2.5ml and 0.5ml normal saline intrathecally. All the solutions were made upto volume of 3ml in a 5ml syringe The addition of dexmedetomidine as adjuvant to hyperbaric bupivacaine has very potential role in rapid onset of block and prolonging the duration of block. It enhances the duration of block almost doubles the duration as with plain hyperbaric bupivacaine. It also exclusively reduces the post operative requirement of first analgesics and also lesser analgesia is required inpostoperative period In our study, the VAS score in the post-operative period was statistically significant among the three study groups from 8th hour to 24th hour time interval as P<0.000. The VAS score were lowest for Group D as compared to GroupF and Group B at all time in the entire post-operative period. We found that, the duration of effective analgesia defined as the time from intrathecal injection to the time of first analgesic requirement was significantly prolonged in Group D, which was 545±61.94 mins, in Group F it was 437.94±43.32 mins, in Group B it was 263.97±22.88 mins respectively. Santos et al in 20075 conducted a double blind, randomized, prospective study to test the effectiveness of 3 mg isobaric 0.5% bupivacaine with 20pg of fentanyl or 15pg of clonidine as adjuvant drugs to promote good surgical conditions for anorectal surgeries. 40 adults undergoing anorectal surgery under spinal anaesthesia were divided in two groups. Spinal anaesthesia was performed on lateral position, with head-down of 30°, 27 G Quinke needle at L3-L4 level. First group received 3 mg isobaric 0.5% bupivacaine with 20mcg of fentanyl and the second group received 3 mg isobaric 0.5% bupivacaine with 15mcg of clonidine. They observed that both adjuvnants promote satisfactory anaesthesia and good postoperative analgesia. Gupta et al6 observed that 5mcg Dexmedetomidine with ropivacaine provided excellent quality of post-operative analgesia with minimal side effects. In 1992, Filos et al 7 conducted a double blind, placebo-controlled study to evaluate the effect of intrathecal clonidine (a2-adrenoceptor agonists) on pain following caesarean section. Twenty patients undergoing elective caesarean section. Twenty patients undergoing elective caesarean section divided in two groups. One group received 150 pg clonidine intrathecally 45 minutes after general anesthesia and the second group received same volume of saline. Pain score were lower in the Clonidine (a2-adrenoceptor agonists) treated group 20 to 120 minutes after injection as measured by VAS. The pain relief the 1st supplemental analgesic request by patient lasted 414 ± 128 minutes after intrathecal clonidine and 181± 169 minutes (mean± SD p<0.01) after saline. Clonidine decreased systolic, diastolic and mean arterial pressure compared to baseline values (p< 0.05), but heart rate and central venous pressure were unaffected (difference not significant). Maximum reduction of systolic arterial pressure was 15± 9%, of diastolic arterial pressure 22±12% and mean arterial pressure 18±12 %. Clonidine did not affect arterial haemoglobin oxygen saturation or PaCO2. Patients in the clonidine group were significantly more sedated (p< 0.05) and more frequently reported a dry mouth (p<0.01) compared to normal saline group. There results suggested that intrathecal clonidine 150mcg is effective in controlling pain especially in post operative period following caesarean section but was associated with some side effects such as hypotension, sedation and dryness of mouth. Kim et al8 observed that fenatnyl beyond 25mcg intrathec ally produced no benefit in regard to the duration of analgesia. However, fentanyl 25mcg intrathecally with low dose bupivacaine improves post-operative analgesia and hemodynamic stability. Fukushima et al9 administered 2mcg/kg epidural Dexmedetomidine for post-operative analgesia in humans, without any neurologic deficit
CONCLUSION On the basis of the present clinical comparative study, we can conclude that sequential administration of Dexmedetomidine 5mcg with 0.5% hyperbaric bupivacaine 2.5ml undergoing elective lower limb and lower abdominal surgeries under spinal anaesthesia, significantly provides good postoperative analgesia compared to fentanyl with minimal or no side effects.
REFERENCES
|
|
 Home
Home