Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
Efficacy and safety of bupivacaine instillation through surgical drain in modified radical mastectomy
Vinutha M1, Rashmi N R2*, VB Gowda3
1,2,3Department of anaesthesiology and pain relief, Kidwai memorial institute of oncology, Bangalore – 560029, Karnataka, INDIA. Email: vinutha881988@gmail.com
Abstract Background and Aims: modified radical mastectomy (MRM) is the commonly used surgical procedure for operable breast cancer.it involve extensive tissue dissection and infiltration may not have adequate post-operative analgesia. As there is increase in the percentage of women undergoing MRM for cancer breast it is essential to give effective postoperative pain control in these patients. This study has been designed to determine analgesic efficacy and side effects of instillation of bupivacaine in surgical drain for postoperative pain relief in patients undergoing MRM for cancer breast. Method: In this comparative prospective randomized clinical study 60 patients aged 20–65years were divided into three groups A, B and C. All patients were administered general anaesthesia. axillary and chest wall drains were placed at the end of the surgery. Group A received 40ml of 0.25% bupivacaine 20ml through each drain. Group B received 40ml of normal saline 20ml through each drain. Group C was the control with no installation. After instillation of study drug, the drains were clamped for period of 10mins. After extubation, pain score for pain was evaluated using visual analog scale and then 4th hourly till 24 hrs. Rescue analgesia was injection tramadol, if the VAS ≥4. Statistical analysis was performed using software SPSS 18.0, and R environment ver.3.2.2 Results: The mean VAS score was never ≥4 in bupivacaine 0.25% group. There was prolonged duration of analgesia bupivacaine 0.25% group with mean duration of action17.64±2.36hrs compared to saline group 6.55±1.97hrs and control 0.55±1.41hrs. There was a significant difference in the total analgesic requirement and the number of analgesic demands between the groups (P<0.001). Conclusion: The instillation of bupivacaine into surgical drain in modified radical mastectomy is a simpler, cheaper and effective method in providing post-operative analgesia with reduced adverse effect related to the drug and minimal or no complication associated with instillation of the drug. Key Word: Local anaesthesia, bupivacaine, postoperative pain, modified radical mastectomy
INTRODUCTION One of the most common malignancies in women is breast cancer and it is a leading cause of cancer death among women. Worldwide each year more than a million are diagnosed with breast cancer. With the increase in the average life span, lifestyle changes and due to improved survival from other diseases, there is overall increase in the incidence of breast cancer.1 It accounts for 33% of all female cancers and is responsible for 20% of the cancer related deaths in women.2The treatment of breast cancer has evolved over the years which includes both surgical resection for local disease and medical therapy for systemic disease. The Consensus Development Conference on the treatment of breast cancer in 1979 stated that the modified radical mastectomy was the standard of treatment forstages I and II breast cancer.3Modified Radical Mastectomy (MRM) is the most common surgery done for operable breast malignancies Although postoperative pain after modified radical mastectomy is comparatively less, many patients may still require potent analgesics, subjecting the patients to the side effects of those drugs. Adequate postoperative analgesia with minimal side effect is major aim of post anaesthesia care.Anti-inflammatory drugs, opioids, wound infiltration with local anaesthetics, have been used but they have limited success rate. Methods like paravertebral blocks3-6 and brachial plexus blocks7require greater skills and are cumbersome compared to instillation in terms of providing analgesia.
MATERIALS AND METHODS After obtaining institutional ethical committee approval a comparative prospective randomized clinical study was done. A total 66 patients posted for modified radical mastectomy were evaluated and those who fulfil the inclusion and exclusion criteria and willing to participate in the study were enrolled for the study Sample Size: Based on F-tests –ANOVA: Fixed effects, omnibus, one-way analysis. According to this we need minimum 63 samples to test the difference. considering the drop out, 66 patients will be included in total sample size with 22 samples in each group. Our study includes patients aged between 20 to 65 years with weight 40-70 kg belonging to ASA physical status Grade I and Grade II consenting for study. Patients with ASA physical status III and IV, or with h/o chronic analgesic drug usage (on oral analgesic >1 month). or those with intraoperative major blood loss, continued excessive blood collection in drain were excluded from the study. A pre-anaesthetic evaluation was done prior to the surgery with all the necessary investigations carried out and documented. The patients then were randomly allocated to one of the three groups (A, B, C) 22 patients in each based on the computer-generated randomization table. Patients are familiarized with pain intensity assessment device visual analogue scale (VAS) and are instructed to request for supplementary analgesic if needed. On the night before the surgery, tab alprazolam 0.5 mg and tab pantoprazole 40 mg oral was given to allay anxiety and apprehension. Nil per oral for solids for 6 hours is advised. On the day of surgery NPO status of the patient was confirmed and shifted to the operation theatre and intravenous access will be secured and iv fluids is started preferably ringer lactate. Standard monitors (pulses oximetry, ECG, Non-invasive blood pressure, end tidal carbon dioxide) were attached and baseline vital parameters were noted. Premedication, Induction and maintenance of anaesthesia was standardized. premedication with Inj. Midazolam (0.05mg/kg), Inj. Glycopyrrolate (0.01mg/kg), Inj. Ondansetron (0.05mg/kg) and Inj. Fentanyl (1.5mcg/kg). After preoxygenation with 100% oxygen for 3 mins, General Anaesthesia was induced with Inj. Propofol (2mg/kg) and Inj. Succinylcholine (1.5mg/kg). Patient was intubated with appropriate cuffed endotracheal tube and tube position will be confirmed and connected to volume-controlled mode of mechanical ventilation. Anaesthesia was maintained with Nitrous oxide 50%, O2 50% and Isoflurane. Muscle relaxant Inj. Vecuronium bromide was given, an initial loading dose of (0.08 mg/kg) followed by intermittent doses of Inj. Vecuronium (0.01mg/kg). NIBP, continuous ECG, EtCO2 and SpO2 will be monitored intraoperatively. At the end of surgery two drains one in chest wall below skin flap (over the pectoral muscle) and other in axillary near the axillary vessel will be placed before closing the surgical incision by the surgeon. As per the randomisation the study drug was given through each drain. Group A received(40ml of 0.25% bupivacaine) 20ml through each drain, Group B received (40ml of normal saline) 20ml through each drain, Group C will not receive any instillation and will be considered as control group. After instillation of study drug, the drain was clamped for period of 10mins then clamp was released to allow the test solution in the negative pressure suction drain. Anaesthesia was reversed with Inj. Neostigmine (0.05mg/kg) and Inj. Glycopyrrolate (0.01mg/kg) and extubated after complete neuromuscular recovery in deep inspiration after thorough suctioning in fully awake state. Patients was shifted to postoperative ICU; standard monitors will be connected. patient will be asked to rate her pain over the VAS scale, pain score at 0 hour is noted and every 4th hourly subsequently for 24hrs. Only resting pain was assessed i.e., static pain score defined as pain experienced by the patient while lying down. If VAS score exceeds 4 at any point of time rescue analgesia with inj. Tramadol (1mg/kg) IV was administered. The total number of rescue analgesic required was noted for 24hrs. The duration of analgesic was calculated from the time of intra-drain instillation of study drug to the first demand of analgesia. Untoward events related to surgical site like hematoma, infection, wound dehiscence was observed. Patient was also assessed for postoperative nausea and vomiting (PONV) whether it is present or absent. Rescue antiemetic Inj. ondansetron 4mg IV will be given.
OBSERVATION AND RESULTS The three groups were comparable with respect to demographic data (age, sex, weight), ASA grade, procedure and duration of surgery.
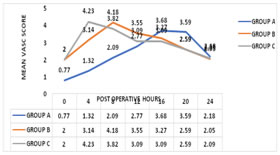
VAS score was significantly lower in group A compared to group B and C (p<0.001). Group A mean VAS score was 3.68±0.65 and 3.59±0.96 during the period of 16th and 20th hour versus 3.27±0.55, 2.59±0.73 and 3.09±075, 2.59±0.50 in group B and C respectively. Group B the mean VAS score was 4.18±0.66 during 8th hour compared to 2.09±0.53 and 3.82 ±0.50 in group A and C respectively. Group C mean VAS score was 4.32±0.72 during 0-hour compared to 2.00±0.69 and 0.77±0.61 in group B and group A respectively.
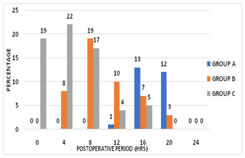
Figure 1: Mean VAS score distribution Figure 2: Total number of subjects who required rescue analgesia
The mean duration of analgesia in the bupivacaine group was 17.64±2.36 hrs, 6.55±1.97 hrs in the saline group, and 0.55±1.41 hrs in the control group. It showed significant difference between the groups. The percentage of subjects who required rescue analgesia in bupivacaine group were 54.5%-63.6% during the period from 16 to 20 hours, that of saline group were 81.8% of subjects during the period of 8 hours, and in the control group 86.4%-100% subjects required analgesia during the period 0-4 hours. There was a significant difference, the total number of rescue analgesic consumption by all the patients in a group during the first 24hours of postoperative period was measured. Group A, group B, group C had 26, 47 and 67 total number of recue analgesia consumption respectively. The total consumption was higher in group C which was statistically significant with p value <0. 001. There was total 0 (0%) event of nausea and vomiting in group A as compared to 2(33%) in group B and 4 (67%) events in group C.
DISCUSSION This study was based on the hypothesis that instillation of bupivacaine 0.25% through surgical drain produces good postoperative analgesia in modified radical mastectomy. The purpose of the study was to provide a better postoperative pain relief to patients undergoing modified radical mastectomy in our institute. The study was purely meant for assessing the pain score and the duration of analgesia of bupivacaine and compare it with saline and control group. Also, to compare any side effect associated with the drug. In group A, bupivacaine 0.25% 40ml was used 20 ml in each drain, 40ml of saline 20ml in each drain was used in group B, group C was treated as a control group and did not receive any drug instillation. The maximum dose of bupivacaine injected was 100mg in any patient. Analgesia relies on the local anaesthesia spread rather than the concentration and therefore its more volume dependent. Hence, we choose the above concentration, volume and dosage. Thus, the dose is well within the recommended maximum safe dose range for bupivacaine i.e.,3mg/kg. Nevertheless, the potential for systemic toxicity must be borne in mind in the setting of inadvertent intravenous injection. In group A mean VAS score was never ≥4, lower mean VAS score was noted in group A compared to group B and group C indicating that bupivacaine instillation provided better postoperative analgesia. The mean duration of analgesia in group A was 17.64±2.36 hours compared to 6.55±1.97 and 0.55±1.41in group B and group C. Thus, the mean duration of analgesia was higher in group A compared to group B and C with p valve <0.001 which was statistically significant. This clearly indicate that instillation of bupivacaine has a prolonged duration of analgesia. In the study conducted by Culleford et al, 37 patients were randomly divided into two group,20 patients were treated with intraoperative topical bupivacaine and 17 patients received placebo. It was observed that that single dose of tropical intraoperative bupivacaine significantly decreased postoperative opioid analgesic requirement compared to control group patient undergoing ambulatory reductive mammoplasty. (p=0.001). There were no complications resulting from Bupivacaine usage.10This study was consistent with our study which showed instillation of bupivacaine through surgical drain in modified radical mastectomy had lower VAS score compared to saline and control group with increase in the mean duration of analgesia. However, normal saline is known to produce some amount of analgesia though it was inconsistent. Pressure over the nerve ending leading to blocking the conduction of nerve impulse is the probable mechanism by which it produces analgesia. It also causes dilution of or washing away of the inflammatory mediators and pain producing substance post operatively there by reduces pain. This was seen in study conducted by Chanrachakul B et al, for paracervical pain relief during fractional curettage where lidocaine was compared with normal saline, though lidocaine provided better pain relief saline also provide some amount of pain relief.11In our present study, the subjects who received saline through the drain had lower pain scores with a mean duration of analgesia of 6.55±1.97 hrs compared to 0.55±1.41 hrs in the control group, with reduced requirement of rescue analgesia compared to control group. In the study conducted by Manaa E et al, to determine if the irrigation of the breast cavity with local anaesthetic in patients undergoing bilateral breast augmentation surgery reduces the rescue analgesia requirement and postoperative pain intensity level measured with VAS score, it was observed that there was significant difference in number of patients who required opioid rescue analgesia with morphine (p<0.01) with 10% in (group I) intervention group where the breast cavity was irrigated with 1% lidocaine with epinephrine (7 mg/kg), 0.5% bupivacaine (3 mg/kg) and normal saline solution versus 50% in the (group O) control group where breast cavity were irrigated with saline solution. He concluded that local anaesthetic irrigation in patients who underwent breast augmentation surgery reduces opioid rescue analgesia requirement and postoperative pain intensity level.9 This was consistent with our study where we observed that total consumption of rescue analgesic was reduced in the patients receiving bupivacaine. In study conducted byAjum.S. Khan Joad et al, to compare efficacy of intravenous tramadol versus bupivacaine irrigation through surgical drain, pain score, nausea, vomiting, sedation, urinary retention, hemodynamic changes were monitored for 24 hours. Both groups had good pain relief. Nausea was more (p<0.007) in group T with more vomiting, bladder catherization, delay in the oral intake was noted in group T but was not statistically significant. He concluded that bupivacaine administered through surgical drain offered equivalent postoperative pain relief to intravenous tramadol with significant less nausea and ¼th reduction in dose of tramadol.8 This study was consistent with our study where instillation of bupivacaine substantially reduced the postoperative pain and opioid consumption and decreased incidence of postoperative nausea and vomiting. This is a comparative prospective randomized clinical study. The result showed that wound instillation of 0.25% bupivacaine through surgical drain had better postoperative analgesia compared to that of the subjects who received saline or no instillation (control) and the duration of analgesia was prolonged in the subjects receiving bupivacaine 0.25% with mean duration of action17.64±2.36 hrs compared to saline group 6.55±1.97 hrs and control 0.55±1.41 hrs, and the total requirement of rescue analgesic which was instituted when VAS score was ≥4 was also reduced in bupivacaine group compared to the subjects who received saline, or no instillation (control). CONCLUSION The instillation of bupivacaine into surgical drain in modified radical mastectomy is a simpler, cheaper and effective method in providing post-operative analgesia with reduced adverse effect related to the drug and minimal or no complication associated with instillation of the drug. With reduction in the need for opioids for providing post-operative analgesia it reduces complications associated with it and is also cost effective. Hence, we conclude that instillation of bupivacaine through the surgical drain in modified radical mastectomy
REFERENCES
|
|
 Home
Home