Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
Effect of oral pregabalin premedication on perioperative haemodynamic response and post operative analgesic requirement for patients undergoing laparoscopic cholecystectomy
A Sandhya1*, H Sahajananda2, Vikyath Jain3
1Senior resident, Department of Anaesthesia and Pain relief, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, INDIA. 2Professor and Head, Department of Anaesthesia, Rajarajeswari medical college and Hospital, Bangalore, Karnataka, INDIA. 3In house Consultant, Department of Neuroanaesthesia and Critical Care, Sparsh Hospital, Bangalore, Karnataka, INDIA. Email: buddsanand90@gmail.com
Abstract Background and Aims: Laparoscopic cholecystectomy was introduced by Phillipe Mouret in 1987. In comparison with open procedures, laparoscopy is characterized by better maintenance of homeostasis and reduced postoperative pain and recovery. The hallmark of laparoscopy is creation of carbon dioxide pneumoperitoneum and change in position from Trendelenburg to reverse Trendelenburg. Hemodynamic changes observed during laparoscopy result from the combined effects of pneumoperitoneum, patient position, anaesthesia and hypercapnia from the absorbed CO2. Transient and variable rise in heart rate and blood pressure may be observed that are well tolerated, in an otherwise healthy individual, reflex increases of vagal tone and arrhythmias can also develop. These effects may however be hazardous to individuals with hypertension, coronary artery disease or cerebrovascular diseases resulting in potentially life-threatening effects like pulmonary edema, myocardial insufficiency, dysrhythmias and cerebrovascular accidents 5 . Laparoscopic surgery is reported to have the significant advantage of reduced post-operative pain and consequently early mobility and reduced duration of hospital stay. In this study, we investigated the efficacy of pregabalin premedication to provide perioperative hemodynamic stability, intra and postoperative analgesia in patients undergoing laparoscopic cholecystectomy. Materials and methods: A prospective randomized double blind placebo controlled clinical study was conducted to study the effect of 150mg oral pregabalin premedication on perioperative haemodynamic response and postoperative analgesic requirement in patients undergoing elective laparoscopic cholecystectomy. Sixty patients of either sex aged 18-65 years undergoing the procedure were randomly allocated to two groups of 30 each after obtaining informed consent. Group I received placebo and Group II received 150 mg of pregabalin with sips of water 75 to 90 minutes before induction of general anesthesia. Fentanyl 0.5mcg/kg i.v was given as supplementary analgesia intraoperatively as needed. Post-operative pain was assessed using visual analog scores and rescue analgesia was given accordingly. Study data was presented in tabulated manner and analyzed using Microsoft Excel and SPSS for windows. Results: Mean arterial pressures (MAP) and heart rate in patients of group II were significantly lower (P and lt; 0.05) after tracheal intubation and pneumoperitoneum and remained lower, as compared to group I, throughout the pneumoperitoneum. Intraoperative and post-operative fentanyl consumption was less in group II compared to group I(Pandlt;0.05). There was no significant difference in the incidence of adverse effects between the two groups. Conclusion: Oral pregabalin attenuates elevation of mean arterial pressure and heart rate during and after pneumoperitoneum thereby providing hemodynamic stability during laparoscopic surgery. Preoperative single dose of pregabalin is effective in reducing perioperative pain and fentanyl consumption in patients undergoing laparoscopic cholecystectomy. Key Word: oral pregabalin premedication.
INTRODUCTION Laryngoscopy and endotracheal intubation are the most important and essential skills for an anesthesiologist to maintain the airway. However, both are noxious stimuli. Haemodynamic responses due to laryngo-sympathetic stimulation after laryngoscopy and intubation may be seen as hypertension, tachycardia, and arrhythmias. Laparoscopic cholecystectomy was introduced by Phillipe Mouret in 1987.1Since then, it quickly became apparent that laparoscopy results in multiple benefits including better maintenance of homeostasis and reduced postoperative pain. The hallmark of laparoscopy is creation of carbon dioxide (CO 2) pneumoperitoneum and change in the patient’s position from Trendelenberg to reverse Trendelenberg. It also results in stress hormone responses (cortisol, epinephrine and nor-epinephrine) especially when CO2 pneumoperitoneum is used concomitantly. 3CO2 gas insufflation is preferred by most laparoscopists because it has a high diffusion coefficient and is a normal metabolic end product rapidly cleared from the body. Also CO2 is highly soluble in blood and tissues and does not support combustion. The risk of gas embolism is lowest with CO2. Hemodynamic changes including increased heart rate and mean arterial pressure obs1erved during laparoscopy result from the combined effects of pneumoperitoneum, patient position, anaesthesia, and hypercapnia from the absorbed CO2. In addition to these pathophysiologic changes, reflex increases of vagal tone and arrhythmias can also develop. 5 This can result in potentially life-threatening effects like pulmonary edema, myocardial insufficiency9, dysrhythmia’s and cerebrovascular accidents 5 especially in individuals with hypertension, coronary artery disease or cerebrovascular diseases4,6,7,8. Many pharmacological methods were evaluated for attenuation of haemodynamic responses of laparoscopy either in premedication or during induction to attenuate the adverse hemodynamic response to laryngoscopy and laparoscopy, such as deepening the anesthesia, pretreatment with vasodilators, adrenoreceptor blockers, calcium channel blocker and opioids, with variable results. Attempts were made as early as in 1950’s by various investigators to reduce the sympathetic response to laryngoscopy and intubation. Use of intravenous anaesthetic induction agents 10 did not adequately or predictably suppress the haemodynamic responses produced by endotracheal intubation11. Additional pharmacological measures like use of volatile anaesthetics10, topical and intravenous lidocaine10,12,13,14, opioids15,16,17 vasodilators – Sodium nitroprusside18, Nitroglycerine19, Calcium channel blockers20,21,22 and β-blockers23,24,25 have been tried by clinicians prior to laryngoscopy. Other drugs especially Alpha-2 agonists like Clonidine, Dexmedetomidine have also been used26,27. All these drugs have been used with varying results and have not been effective in completely suppressing the sympathetic response to intubation. Many of these agents also have various side effects. There is a need for a single drug which can effectively suppress both cardiovascular response to laryngoscopy and intubation with minimal adverse effects. Pregabalin possesses several properties to make it a valuable premedicant to attenuate the hemodynamic response of laryngoscopy and pneumoperitoneum. Pregabalin, an antiepileptic drug, is effective in controlling neuropathic component of acute nociceptive pain of surgery by inhibiting membrane voltage-gated calcium channels. It does not interact with GABA receptors. However, only few data are available in the literature regarding the effect of prebagalin on the cardiovascular system. Its analgesic, anticonvulsant, and anxiolytic activities make it useful oral premedicant. It is well absorbed after oral administration, with peak plasma concentrations occurring within 60 minutes. Pregabalin has been found to suppress the intubation response to laryngoscopy and intubation28,29. Onset of action of oral Pregabalin is one hour 30 and cmax occurs in two hours. It may also be useful in patients undergoing laparoscopy. Pregabalin is available as capsules of 75mg and 150mg. Not many studies have tried to find out the optimal dose of Pregabalin that can be used for suppression of response to intubation and pneumoperitoneum. Hence a study was required to know the effective dose of Pregabalin for the same. METHODS Source of data: Study was conducted on 60 patients undergoing laparoscopic surgery in Rajarajeshwari Medical College and hospital, Bangalore for 18 months. Method of collection of data: (including sampling procedure if any): The data for study was collected from subjects fulfilling inclusion criteria/exclusion criteria and admitted as inpatients in RRMCandamp; H Study design: A hospital based prospective, randomized double blind trial. Study period: October 2014- April 2016 Inclusion criteria:
Exclusion criteria:
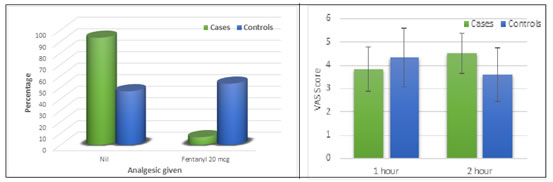
Methodology of Study: -Selection of patients based on those satisfying the inclusion criteria. Group I received placebo preparation of vitamin B12 capsules and Group II received pregabalin (150 mg) given with sips of water about 75 to 90 minutes before induction of general anaesthesia. These doses were considered to provide adequate and comparable preoperative sedation, anxiolysis and perioperative hemodynamic stability. The protocol-defined primary endpoint were preoperative sedation and anxiolysis, hemodynamic responses to laryngoscopy and laparoscopy, intraoperative analgesic requirement, quality of postoperative recovery, and occurrence of premedication induced side effects Before administration of the oral premedication, each patientand#39;s baseline heart rate, mean systemic arterial blood pressure, and pulse oximetry were measured. In addition, ramsay’s scale for sedation were completed for each patient. Anaesthetic management: On arrival to operation theatre, routine monitoring of baseline vital parameters was recorded and a crystalloid intravenous infusion of 6 to 8 ml kg -1 hr -1 was started. All patients were premedicated with inj. glycopyrrolate (0.2 mg), and inj. fentanyl (1 μg kg -1). After preoxygenation for 3 minutes, anaesthesia was induced with inj. propofol 2 mg/kg or till loss of verbal response. The laryngoscopy and intubation were facilitated with inj. rocuronium 1 mg kg-1 with minimum possible duration and were similar for all patients. Following induction, a nasogastric tube was placed. Anaesthesia was maintained with minimum alveolar concentration (MAC) of 0.8% isoflurane, nitrous oxide 60% in oxygen. The patients’ lungs were mechanically ventilated with minute ventilation adjusted to maintain normocapnia (EtCO 2 between 35 to 40 mm Hg). Supplemental neuromuscular blockade was achieved with rocuronium 0.1 mg kg -1. During surgery, the peritoneal cavity was accessed with a blunt-tipped 12-mm trocar after Inj. Ligno-Adr was used for local infiltration and carbon dioxide was insufflated to create pneumoperitoneum at a rate of 2 L/min. After pneumoperitoneum, necessary change in minute ventilation was done to maintain normocapnia. Patients were positioned in a 20 degree reverse Trendelenburg position, and were rotated toward the left side to facilitate exposure of the gall bladder. The intra-abdominal pressure was maintained at 12-14 mm Hg throughout the laparoscopic procedure. Ondansetron 4mg was administered i.v 20 min prior to extubation. At the end of surgery, patients were returned to supine position and residual carbon dioxide was expelled by abdominal compression. The total surgical procedure time was around 75 to 90 minutes. Intraoperatively, patients were observed for any complications like hypotension/hypertension, tachycardia/bradycardia, arrhythmias, hypercapnia, and bronchospasm. Tachycardia, hypertension, and clinically insufficient analgesia were controlled with supplementary doses of intravenous fentanyl (0.5μg/kg). Hypotension primarily was treated by increasing the intravenous infusion rate (15 ml/min) and additionally with vasoactive drugs. Bradycardia, defined as heart rate slower than 50 beats/min, was treated with 0.01 mg/kg i.v. atropine. Isoflurane was discontinued after the last skin suture and residual neuromuscular block was antagonized with appropriate doses of inj. neostigmine (0.05 mg kg-1) and inj. glycopyrrolate (0.01 mg kg-1). The extubation was performed when respiration was spontaneous and adequate. The systemic mean arterial blood pressure, heart rate, pulse oximetry and EtCO 2 were recorded before premedication and induction, at 1 minute, 3 minutes and 5 minutes interval after intubation, and 15 minutes after creation of pneumoperitoneum. Thereafter, these changes were recorded at 15 minutes intervals, followed by 10 minutes after release of pneumoperitoneum and 15 minute, 30 minutes following extubation. All groups were compared for sedation and anxiety level, along with changes of heart rate and mean arterial pressure (MAP), prior to premedication, before induction, after laryngoscopy, pneumoperitoneum, release of carbon dioxide, and extubation. Intraoperative analgesic requirement and effects on postoperative recovery, nausea, vomiting, and shivering were also compared. Postoperative follow-up: Patients were transferred to postanesthesia care unit and monitored for at least 3 hours or until there were no signs of any drug-induced effects. Any hemodynamic abnormalities, need for postoperative opioid analgesic medication, and incidence of nausea and vomiting along with requirement for rescue antiemetic were also noted. Statistical Methods: The sample size was decided in consultation with the statistician. The difference between two means of mean arterial pressure at 1 min of intubation is 10 and mean standard deviation is 9 36. Power of study was conducted with confidence limit of 80% with calculated sample size by allowing an α of 0.001 and β of 0.2 per group is 31. As all the distributions will merge into normal distribution, sample size i.e., 30 is enough because inference that can be drawn based on 30 observations will more or less remain the same, in spite of any increase in the sample size 37. Hence a total of 60 subjects were included in our study and divided into two groups each containing 30 subjects 38. Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean SD (Min-Max) and results on categorical measurements are presented in Number (%). Student t test (two tailed, independent) was used to find the significance of study parameters on continuous scale between two groups (Inter group analysis) on metric parameters. Chi-square/ Fisher Exact test was used to find the significance of study parameters on categorical scale between two or more groups. Statistical software: The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc. RESULTS In our study demographic data was mentioned where the mean age of subjects among cases was 44.4311.37 while that of controls was 41.57 8.43, Intervention group consisted of 37% males and 63% females. The controls group was distributed as 57% males and 43% females. There was no significant difference in distribution in age and gender between the cases and controls. ASA grading in both groups were 73% in intervention group and 80% in control group of ASA1 and rest was ASA2 group in the study. In our study, the baseline hemodynamic parameters between the two groups were similar (no significance, Pandgt;0.05). There was no difference in the heart rate between the 2 groups pre operatively, prior to premedication and induction. However, a rise in heart of 15 beats was noted 1 min following intubation in the control group I with a p value of 0.072. The heart rate increased by ~12beats in 1 st minute after intubation in the intervention group. The heart rate remained relatively stable in both groups at 3 and 5 minutes following intubation. The heart rate remained stable in both groups during pneumoperitoneum. + Suggestive significance (P value: 0.05andlt;Pandlt;0.10). At 1 st minute after laryngoscopy and intubation there was an increase in the MAP of 14mmhg in control group I which did not reach basal value at the 5 th minute. In contrast, a fall in MAP following intubation was noted in the intervention group II. An elevation in MAP of ~10mmhg was noted 15 minutes following pneumoperitoneum which persisted at the 30 min interval too and returned to baseline values at 45 min interval in the control group. The MAP did not vary significantly in the intervention group II. A significant rise in MAP was noted following intubation in the control group I. MAP was also elevated following creation of pneumoperitoneum that persisted up to 30min in the controls group I. Group II had no significant rise in MAP values following intubation and pneumoperitoneum. There was no significant difference in pre-operative and post-operative sedation scores up to 3hours between the 2 groups in our study. 16 out of 30(53.3%) patients in the controls group needed rescue analgesic fentanyl (0.5mcg/kg) after 1hr post operatively with VAS of 4 and above. Only 2 patients (6.7%) in the intervention group needed fentanyl at 1 hour post operatively. The post-operative fentanyl requirement at 1 hour post-operative period was significantly higher in the controls group as compared to the study group with p-<0.001. Our study showed vas scores of andgt;/ 4 at the end of first hour post-operative period which necessitated the need for earlier fentanyl administration in the control group.
Figure 1
Figure 3 Figure 4 Figure 1: Comparison of perioperative heart rate between cases and controls; Figure 2: Comparison of MAP (mm Hg) in two groups studied (Student t test); Figure 3: Post-operative fentanyl requirement after 1 hour; Figure 4: Post-operative fentanyl requirement
DISCUSSION In our study, the baseline hemodynamic parameters between the two groups were similar (no significance, Pandgt; 0.05). The increase in heart rate 1 min after intubation was higher in the control group in comparison with the pregabalin group. The heart rate changes at other time periods between two groups were insignificant. There was a significant rise in MAP 5 minutes after intubation which persisted upto 15 min in the control group. After laryngoscopy and intubation, the attenuation of mean arterial blood pressure in the premedicated group was statistically significant as compared with the control group. This is comparable to a perspective study by Kumkum et al 31 where Pregabalin premedication was used to see hemodynamic stability during general anesthesia, where an increase in heart rate 1minute after intubation was noted more in the control group compared to the intervention group. A significant rise in MAP was also noted following intubation that persisted upto 3 minutes after intubation, whereas Mean arterial pressure was attenuated in the pregabalin premedicated group to statistically significant value. Bhawna Rastogi et al 28 also conducted a similar study to see Oral pregabalin premedication for attenuation of haemodynamic pressor response of airway instrumentation during general anaesthesia: A dose response study were they compared placebo, pregabalin 75mg and pregabalin 150mg doses and they saw maximum increase in heart rate in control group then other two groups and there was also no significant change in heart rate between 75-150mg group. Attenuation of MAP was noted in a dose related manner in the pregabalin premedicated groups compared to the control group with maximum attenuation seen in the P150 group. This is comparable to the results found in our study. When assessing techniques to lessen the haemodynamic pressor responses of airway instrumentation, the induction agents may influence the results. The salivary and tracheobronchial mucus secretions necessitate prophylactic administration of an antisialagogue i.e Glycopyrrolate, which does not penetrate the blood–brain barrier. We have used propofol as an induction agent similar to the above mentioned study which produces hypotension more than thiopental and bradycardia, which has helped to compensate in part the haemodynamic changes induced due to laryngoscopy and intubation in all patients. By its effect at alpha-2-delta site Pregabalin has been shown to reduce the depolarization- induced calcium influx at nerve terminals with a consequential reduction in the release of several excitatory neurotransmitters, including glutamate, norepinephrine, substance P, and CGRPs. that have been implicated in pain perception. It is probable that this modulation of neurotransmitter release by pregabalin contributes to its reduction of haemodynamic perturbations following airway instrumentation and pneumoperitoneum and its analgesic effect. Pregabalin may be used in asthmatic and airway‑compromised patients as it does not cause post‑operative respiratory depression. There was no significant variation in etco2, spo2 between the groups in our study. Sedation scores and post-operative analgesic requirement There was no significant difference in pre-operative and post-operative sedation scores upto 3hours between the 2 groups in our study. Our study showed VAS scores of andgt;/ 4 at the end of first hour post-operative period which necessitated the need for earlier fentanyl administration in the control group I. A.Agarwal et al 32 conducted a study on the efficacy a single preoperative dose of 150mg pregabalin for attenuating postoperative pain and fentanyl consumption after laparoscopic cholecystectomy. Postoperative pain (static and dynamic) at 0-4 hours and postoperative patient-controlled fentanyl consumption were reduced in the pregabalin group compared with the placebo group (Pandlt;0.05). In May 2012, Fatih Balaban, MD 33 et al reported that Preemptive pregabalin decreased pain scores and postoperative fentanyl consumption in patients after laparoscopic cholecystectomy in a dose-dependent manner. (150mg and 300mg respectively) In May 2016 Rajshree Mishra et al 34 conducted a Comparative clinical study of gabapentin and pregabalin for postoperative analgesia in laparoscopic cholecystectomy. The VAS at 1hour post-operative was lower in the pregabalin group compared to the placebo groups as seen in our study. The time needed for first rescue analgesic was more in the pregabalin group which was also observed in our study. Kumkum gupta et al 31 reported in 2011 that Pre-incisional analgesia has been shown to be more effective in control of postoperative pain by protecting the central nervous system from deleterious effects of noxious stimuli and resulting allodynia and increased pain. Within the context of an integrated approach, attempts have been recently made to introduce adjuvant with the intention to facilitate early recovery with decrease side effects related to opioids. In our study there was no post op nausea and vomiting with 150mg pregabalin where same Ibrahim M Esmat et al 35 in their study titled “Comparative study between paracetamol and two different doses of pregabalin on postoperative pain in laparoscopic cholecystectomy” reported significant post-operative vomiting (P andlt; 0.01) in patients who received 300mg pregabalin preoperatively (9 patients) while it was absent in patients who received 150mg pregabalin preoperatively. A. Agarwal 32 et al also conducted a similar study to evaluate the effect of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy and found that there was no significant difference in the incidence of side effects namely postoperative nausea and vomiting (PONV), headache, sedation and respiratory depression in both pregabalin and placebo groups. CONCLUSION Pre-operative administration of oral pregabalin in a dose of 150mg reduces the haemodynamic effects of laryngoscopy and intubation and maintains stable haemodynamics in the presence of pneumoperitoneum during laparoscopic cholecystectomy. It also reduces immediate postoperative analgesic requirement without notable adverse effects.
REFERENCES
|
|
 Home
Home
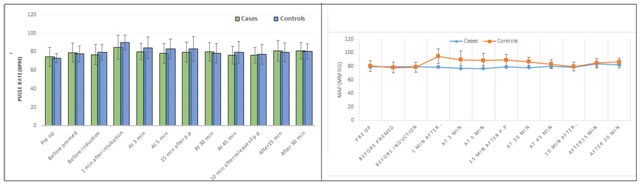 Figure 2
Figure 2