Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
Use of Baska mask for laparoscopic surgeries in adult patients: A prospective observational study
Anil Kumar M R, Sarika M Shetty*, Prashant Parmar, Vyshnavi S, Archana S, Madhu B
Department of Anaesthesiology, JSS academy of Higher Education and Research, Mysuru, Karnataka, INDIA. Email: drsarikamshetty@yahoo.com
Abstract Background: Baska mask is the first commercially available third generation, self-sealing supraglottic airway device that is recently introduced in India. This study is conducted to know the efficacy of the device in patients with normal airway when used for providing general anesthesia during laparoscopic surgeries. Material and Methods: Hundred patients in the age group of 18-60 years, American society of Anesthesiologists-physical status I and II and body mass index of 20-30kg/m2 undergoing elective laparoscopic surgery were included in the study. Exclusion criteria included any history or predictors of difficult intubation, pregnancy and head and neck surgery. Primary objectives were ease of insertion, time and number of attempts to successfully place the device, leak fraction and airway sealing pressure. Secondary objectives were fiberoptic view of the glottis (Brimacombe score) following placement of the device, and any airway morbidity following the insertion. Statistical analysis was done using SPSS software version 22. Descriptive statistics like Mean±SD, t test and chi square test were used. Results: In the first attempt, the device was placed successfully in 94% of the patients; ease of insertion was very easy in 84% of the patients and mean insertion time of 10.21 seconds. Average airway sealing pressure was 41.46 cm of H2O with leak fraction of 8% and fiberoptic view of the glottis was grade I in 87% of the patients. On removal of the mask, mild bloodstaining was noticed in 2%. Conclusion: Baska mask can be considered as an efficient supraglottic airway device in patients undergoing laparoscopic surgeries owing to its fast and easy insertion, effective sealing pressure and minimal trauma to the oropharyngeal tissues. Key Word: Supraglottic airway device, Baska mask, Laparoscopic surgery, Airway sealing pressure, Brimacombe scale
INTRODUCTION Endotracheal intubation was the gold standard technique of securing the airway during laparoscopic surgeries. Airway management during laparoscopy is complicated by intraperitoneal carbon dioxide inflation and change in patient position resulting in increased airway pressures. The increased risk of pulmonary aspiration secondary to increased intraabdominal pressure necessitates having a leak proof airway in the trachea. In recent times, various supraglottic airway devices (SAD) especially Proseal LMA are being used for laparoscopic surgeries with good results. The Baska Mask (Logikal Health Products PTY Ltd., Morisset, NSW, Australia) is the first commercially available third generation novel supraglottic airway device designed by Dr Kanag and Dr Meenakshi Baska, an Australian anesthetist and physician of Indian origin.1 The characteristic feature of Baska mask is that the airway pressure is transmitted intermittently to the flexible element of the cuff forming a perfect seal against the laryngeal wall. To begin with, we had completed (2016-17) an observational study on the use of Baska mask in 100 patients with normal airway for all elective surgeries requiring general anesthesia.1 Hence,the present study was undertaken to study the safety and efficacy of the Baska mask in patients with normal airway undergoing elective laparoscopic surgeries. Primary objectives of the study were ease of insertion, time and the number of attempts required to successfully place the device, airway sealing pressure and leak fraction. Secondary objectives were comparison of hemodynamic parameters pre and post insertion of mask, fiberoptic assessment of the glottic view through the airway, ease of removal, effectiveness of securing the airway in overweight patients and postoperative airway morbidity.
METHODS After obtaining ethical committee approval and informed written consent, this observational study of 6 months duration was conducted on 100 adult (18–60 years age) patients with American Society of Anesthesiologists-physical status (ASA-PS) grade I and II, Modified Mallampatti class I and II and body mass index (BMI) 20-30 kg/m2 undergoing elective laparoscopic surgeries under general anaesthesia. Patients with BMI of 20-24.9 kg/m2 were normal and 25-30 kg/m2 were overweight as per the World Health Organization (WHO) classification. The patients who were excluded from the study were those with predicted or previously documented difficult airway, pregnancy, increased risk for gastric aspiration, surgery in non-supine position and any past allergic reactions to silicone. A thorough pre-anaesthetic evaluation including airway examination was done 24-48 hours prior to the surgery, informed written consent was obtained and necessary advice was given. A pilot study was performed on 20 patients where it was noted that #3 size mask was suitable for patients up to 75 kgs and difficulty in insertion of #4 size mask was noticed as against the manufacturers recommendation (of #3 size for 30-50 kgs and #4size for 50-70 kgs.)Hence it was decided that #3 size Baska mask would be used for all the patients. On the day of surgery in the operation theatre, intravenous fluid was started, noninvasive monitors like electrocardiogram (ECG), non-invasive blood pressure (NIBP) and pulse oximeter (SPO2) were attached and basal parameters were recorded. Using lidocaine jelly, #3 size Baska mask was well lubricated. General anaesthesia protocol of our hospital was followed and all patients were uniformly premedicated with intravenous (IV) midazolam 0.02 mg/kg and IV fentanyl 1mcg/kg, 15 minutes prior to induction of anaesthesia. Preoxygenation was done for 3 minutes and anesthesia was induced in the supine position with the patient’s head in neutral position using propofol 2 mg/kg. After confirming adequacy of ventilation with end tidal carbon dioxide (EtCO2) tracing and bilateral chest rise, vecuronium 0.1 mg/kg was given and ventilated for 3 minutes. Following adequate muscle relaxation, the Baska mask was inserted by an anesthesiologist who had experience of inserting a minimum of 50 Baska masks prior to this study. Adequacy of ventilation was checked as indicated by bilateral chest rise and confirmed by capnography and the study parameters were noted. Insertion time was noted as the time period between the tip of the Baska mask passing through the lips to the first tracing of the EtCO2 curve (successful device placement). Ease of insertion was tabulated as very easy, easy, difficult and very difficult.1 2 minutes of post placement of mask the heart rate and mean blood pressure were recorded; SPO2 and EtCO2 were noted at 10 minute. At 5 minutes post placement of the Baska mask and prior to peritoneal inflation, airway sealing pressure was calculated as the plateau airway pressure with fresh gas flow of 5 litres/min and pressure adjustment valve set at 70 cmH2O. Leak fraction percentage was calculated as (Vinsp-Vexp)/Vinsp x100.1 Changes in the airway pressure and leak fraction were noted 5 minutes post insufflation of gas into the peritoneal cavity. 14-gauge well-lubricated Ryle’s tube was inserted through one of the 2 side ports present on either side of the mask. The correct placement of the device was assessed in terms of the glottic view obtained by fiberoptic (Karl Storz) evaluation using Brimacombe scoring system2 (Table 1). Anaesthesia was maintained with isoflurane 0.8% to 1.5% in a mixture of nitrous oxide and oxygen. On insertion of the laparoscope the surgeon was asked to check for any gastric distension. Haemodynamic parameters were again noted at 15 minutes following insertion of the mask. Table 1: Brimacombe scale2
At the conclusion of surgery, the Ryle’s tube was removed as it was connected to a continuous suction port, the sump cavity and the oral cavity is suctioned using a separate suction tube. Neuromuscular blockade was reversed using a mixture of neostigmine and glycopyrrolate and when the patient is fit for extubation, the Baska mask was removed making note of any trauma to the oropharyngeal structures as evidenced by blood stains on the mask. The ease of removal was graded as very easy, easy, difficult and very difficult.1 Postoperatively, patients were asked about any complaints of hoarseness, sore throat and dysphagia immediately after removing the mask and at 2 hours and 12 hours post extubation. RESULTS The data obtained were analyzed using SPSS software version 22 and interpreted as descriptive statistics in the form of percentages and mean ± standard deviation (SD). For analysis of continuous variables independent samples t-test was applied and for categorical variables chi-square test was used. Value of p <0.05 was considered significant in this study. Demographic values of the patients included in the study are as shown in Table 2
Table 2: Demographic profile
Table 3 represents the comparison between normal and overweight patients with respect to the efficiency of using Baska mask in both the groups.
Table 3: Comparison between normal weight and overweight patients
0.002*-p<0.05-statistically significant
Ease of insertion was very easy in 84% of patients, easy in 13%, difficult in 2% and very difficult in 1% of patient. Table 4 demonstrates the effect of pneumoperitoneum on airway pressure and leak fraction with the use of Baska mask.
Table 4: Efficacy after Pneumoperitoneum
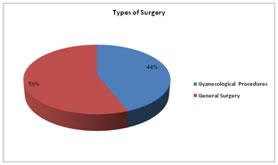
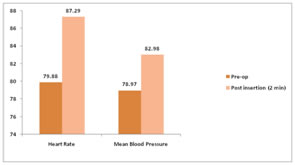
Graph 1 depicts the percentage of laparoscopic surgeries that belonged to gynecology and general surgery. Gyanecological surgeries included mainly Total Laparoscopic Hysterectomy (24), Laparoscopic ovarian cystectomy (7), Laparoscopic tubal ligation (7), and Diagnostic laparoscopy (6). General surgeries included mainly laparoscopic cholecystectomy(44), Laparoscopic appendectomy(7), Diagnostic laparoscopy(4) and Laparoscopic inguinal hernia repair(1) After insertion of the laparoscopic port, gastric inflation was noticed only in 7 cases. As shown in graph 2 the difference in heart rate in pre-operative period and 2 minutes after insertion of Baska mask is statistically significant (p < 0.001), but the difference was not clinically significant.
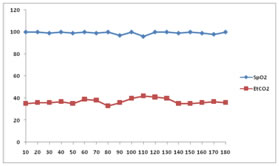
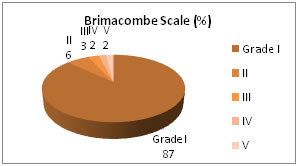
Graph 1 Graph 2 Graph 3 Graph 4 Graph 1: Type of the surgeries; Graph 2: Difference in hemodynamic parameters pre and post insertion of mask; Graph 3: Continuous monitoring of SpO2 and EtCO2 intraoperatively Graph 4: Brimacombe scale observation by fiberoptic bronchoscope
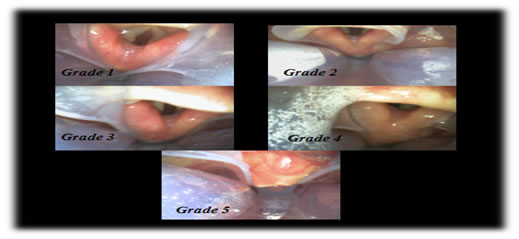
There was no episode of desaturation and oxygen saturation was maintained above 95%, and EtCO2 was maintained between 35-45mmhg in all the study patients throughout the procedure. Brimacombe scale - 87% patients showed grade 1 while only 6% patients had grade 2, 3% patients had grade 3, 2% patients had grade 4, 2% patients had grade 5; none had grade 6 as shown in graph 4
Figure 1 depicts the varied Brimacombe grades as obtained by using the fiberoptic scope after placement of the mask. Figure 1: Fiberoptic images and Brimacombe scaling Ease of removal was very easy (as per the classification1) in all the 100 patients. . Total duration of surgery was 89.9±36.3 minutes and the duration of anaesthesia was 101.07±36.4 minutes.
Mild blood staining of the device was noted in 2% of the patients. Table 5 depicts the airway morbidity observed in terms of sore throat, dysphonia and dysphagia following extubation. Table 5: Post-operative morbidity
DISCUSSION Endotracheal intubation under general anesthesia was considered as the ideal choice of airway management in laparoscopic surgeries. However, the exaggerated hemodynamic stress response during endotracheal intubation in contrast to quick, easy and decreased requirement of muscle relaxant during placement of the SAD have led to a declining interest in endotracheal tubes and this resulted in the use of supraglottic airway devices for laparoscopic surgeries under general anaesthesia.3 The safety of supraglottic devices has been upheld in terms of reducing the risk of aspiration more so in laparoscopic procedures. Hemodynamic stress response has been minimal and post extubation airway morbidity is almost insignificant. The latter generations of these devices like the Baska mask have been very efficacious in maintaining adequate ventilation and normocapnia, high sealing pressure prevents gastric distension, regurgitation and significantly reduces the risk of aspiration which is very vital during laparoscopy. It allows for easy passage of Ryle’s tube through one of its ports thus allowing easy suction of gastric secretions. The device also facilitates easy suctioning of secretions in the pharynx that is collected in the device. V. Alexiev, A. Salim, L.G.Kevin and J.G. Laffey4 conducted an initial observational study to assess Baska mask in 30 low-risk female patients. The overall success rate of insertion was 96.7%, while the success for the first insertion attempt was 76.7%, mean airway sealing pressure was 35.7cmH2O and the incidence of post-operative airway morbidity was very low They concluded that the Baska mask demonstrates a level of utility as an alternative supraglottic airway that is worthy of further clinical study. Similarly in all the 100 patients of our study, Baska mask was successfully placed in either the first attempt (94%) or second attempt (6%). Average airway sealing pressure was 41.44±4.79cmH2O and airway morbidity in the form of mild sore throat and dysphonia was present for few minutes in the immediate extubation period. Successful device placement and faster insertion time are the major goals of securing the airway during general anaesthesia for any kind of surgery which gradually improved with the experience of the anesthesiologist using the Baska mask in this study. Continuous positive pressure ventilation gradually increases the cuff seal around the larynx; hence airway sealing pressure is known to improve over time following insertion of the mask. However, serial measurements of airway sealing pressure were not done in our study. Alexiev, V.; Coyne, J.; Salim, A.; Laffey, J.5 reported the use of Baska mask in 19 low risk adult females undergoing gynaecologic laparoscopic procedures with 95% overall successful insertion rate and obtained a leak pressure of 40cmH2O and a leak fraction of 6.3% V. Alexiev et al.6 compared the Baska mask with the single-use classic laryngeal mask airway (cLMA) in 150 females posted for ambulatory surgery at low risk for difficult tracheal intubation in a randomised, controlled clinical trial. They found that the Baska mask had a higher airway seal pressure (40 cmH2O) when compared to cLMA (22cmH2O) indicating a better seal. This property of Baska mask is very useful in clinical situations like laparoscopic procedures where the seal with the glottic aperture takes priority over ease of insertion in order to prevent any regurgitation and aspiration. Adjustment of the depth of insertion may be required to minimize leaks and maintain higher airway sealing pressures. The author also had issues regarding appropriate sizing of the Baska mask that later followed the manufacturers recommendation based on the weight. However, initial unsuccessful attempts were followed by replacement of a larger size mask. Hence, this study was restricted to adult females to reduce variability with regard to choosing the appropriate size of the mask. Sun Kyung Park et al 7 in their meta-analysis study compared the SAD’s and endotracheal tubes with regards to clinical performances and incidence of complications in patients undergoing laparoscopic surgery. There was no significant difference in the insertion time, success rate of insertion, oropharyngeal leak pressure and incidence of desaturation. However, the incidence of laryngospasm, cough at removal, sore throat, dysphagia and dysphonia was higher in the endotracheal group as compared to the supraglottic device group. Thus they concluded that SAD may be a better alternative to endotracheal intubation in laparoscopic surgeries.6 Laparoscopic surgeries have been the mainstay of surgical specialty and its advantage include minimal invasiveness, reduced postoperative pain; early mobilization and shorter hospital stay.8 Intraoperative peritoneal CO2 insufflation can increase the respiratory load, risk of air leakage causing insufficient ventilation and gastric inflation, aspiration and other respiratory complications.9 M. Carrio Font a, R, Garcia-Aguado b and b Pascual J. Ubeda10 reported a case of laparoscopic Nissen fundoplication using Baska mask. The risk of regurgitation and aspiration being higher in this case of gastroesophageal reflux accompanied with Trendelenburg position during the surgery, Baska mask was chosen owing to its high sealing pressure and 2 gastric drainage and suction channels. Maltby JR et alconducted a study in 109 patients undergoing laparoscopic cholecystectomy classifying them as non-obese and obese (BMI>30 kg/m2) and 4/16 obese patients required endotracheal intubation due to failure of insertion of the SAD.11 As our study was a novice study conducted to evaluate the safety and efficacy of the Baska mask in adult patients undergoing general anaesthesia for elective laparoscopic surgeries, patients with any predictors of difficult airway and risk of aspiration were excluded from the study. Therefore, in future, use of Baska mask should be evaluated in patients with anticipated and unanticipated difficult airway, as well as its efficacy should be compared with other supraglottic airway devices or standard endotracheal intubation technique in patients undergoing laparoscopic surgeries. The limitation of this study- 1) #3 size mask was used for all the patients irrespective of the weight. 2) The hemodynamic parameters were noted only at 2 and 15 minutes after insertion of the mask and not at regular intervals as this study mainly concentrated on the ease of insertion and efficacy of Baska mask. CONCLUSION Securing the airway is the major concern of every practicing anesthesiologist. Baska mask was successfully and easily placed in the first attempt with airway being secured very rapidly. It provided effective ventilation in terms of minimal leak fraction and good airway sealing pressures, which is very essential in laparoscopic surgeries. Minimal incidence of airway morbidity helps in patient compliance and early recovery. So Baska mask can be considered as an ideal supraglottic airway device which can be used in patients with normal airway posted for laparoscopic surgeries. This research did not receive any specific grant from funding agencies in public, commercial, or not-for-profit sectors. REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home