Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
Effect of preanesthetic medication Clonidine vs gabapentin on hemodynamic responses following laryngoscopy and tracheal intubation: A comparative study
Chauhan A1, Konduri S2*, Bollampally B3
1Consultant, Department of Anaesthesiologist, Tristar Hospital, Surat, Gujarat, INDIA. 2Assistant Professor, Department of Anaesthesia, Apollo Institute of Medical Sciences and Research, Hyderabad, Telangana, INDIA. 3Consultant, Department of Anaesthesiologist, Aditya Hospitals, Hyderabad, Telangana, INDIA. Email:dr.sushma@gmail.com
Abstract Objective: Comparing the effect of Clonidine and Gabapentin as premedication in attenuating hemodynamic responses following laryngoscopy and tracheal intubation was primary objective. Methods: In this randomized, prospective study, patients aged 18-60 years with American Society of Anaesthesiologists grade I or II were included and randomized into three groups (Control, Clonidine (0.2mg) and Gabapentin (900mg).Control group received standard of care; those randomized to other groups received either Clonidine or Gabapentin as premedication, 120mins prior to the procedure. Heart rate (HR), systolic and diastolic blood pressure (SBP and DBP), mean arterial pressure (MAP) were monitored. Results: Thirty patients in each group with Mean±SD age of 40.5±14.9years, and body weight 53.5±5.3Kgs were included. HR in control group reached maximum (111.33beats/min) at 1min after laryngoscopy and remained above baseline till 10min after laryngoscopy and intubation. Maximum and minimum HR was 92.83 and 84.10beats/min with Gabapentin and 85.53 and 76.33beats/min with Clonidine were noted at 1 min after laryngoscopy, respectively. Highest mean SBP 151.33±8.47mmHg, DBP 100.33±6.70mmHg and MAP 117.11±5.04mmHg was in control group at 1 min after laryngoscopy. Lowest mean SBP of 109.36±5.89mmHg, DBP 72.06±5.40mmHg and MAP 84.50± 3.92mmHg was seen with Gabapentin at 10 min after laryngoscopy. HR, SBP, DBP and MAP differed significantly (p<0.0001) among the study groups and to time (p<0.0001). Conclusion: Gabapentin and Clonidine at given doses, as premedication, 120min before surgery are effective in blunting hemodynamic response to laryngoscopy and endotracheal intubation. Clonidine has greater impact on HR; Gabapentin has significant attenuating effect on the SBP, DBP and MAP. Key Words: Attenuation of hemodynamic response, Clonidine, Gabapentin, Endotracheal intubation, Laryngoscopy.
INTRODUCTION Laryngoscopy is known to have profound cardiovascular effects like transient hypertension, tachycardia and various arrhythmias along with an increase in circulating catecholamine. The hemodynamic changes probably are of little significance in healthy individuals but are severe and more dangerous in hypertensive and coronary artery disease patients.1Preanesthetic medication forms an integral part of anesthetic management, and some form of premedication is universally administered before any anesthesia. The ideal premedicant must be effective and pleasant to be taken orally, have analgesic and anti-emetic properties, must not impair cardiovascular stability or depress respiration, have antisialogogue effect and effectively alleviate apprehension of the patient. Many pharmacological interventions have been suggested to attenuate these reflex responses to laryngoscopy and intubation including the use of a variety of agents such as β- blockers, calcium channel blockers, vasodilators, local anesthetics (lidocaine), magnesium, etc.2 In the recent decade, several studies have focused on Clonidine and newly on Gabapentin premedication to attenuate the hemodynamic responses following laryngoscopy and tracheal intubation. Clonidine is an α2 –adrenoceptor agonist with sedative and analgesic effects. It also has the beneficial effect of blunting hyperdynamic responses due to laryngoscopy and tracheal intubation.3-9 Gabapentin, introduced in 1993, is a second generation anticonvulsant drug with a widespread effect on pain and hemodynamic response. Pre-treatment with a single dose of Gabapentin prevented the dose-dependent development of hyperalgesia (which is N-methyl-D-aspartate (NMDA)-mediated) and tactile allodynia (which is α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and metabotropic receptor-mediated).10 The mechanism by which Gabapentin attenuates the hemodynamic response to laryngoscopy and intubation is unidentified. The drug inhibits the membrane voltage-gated calcium channels, therefore acting in a manner like calcium channel blockers. Recently, its role in attenuation of hemodynamic responses following laryngoscopy and intubation has been noticed.11-13 The advantages of using Gabapentin or Clonidine premedication for attenuation of cardiovascular responses to the laryngoscopy are easy administration, no significant side effects, and availability with low price. Also, both drugs have antinociceptive effects that may be beneficial for controlling post-operative pain. We compared the effect of Clonidine and Gabapentin in modifying the hemodynamic response following laryngoscopy and tracheal intubation.
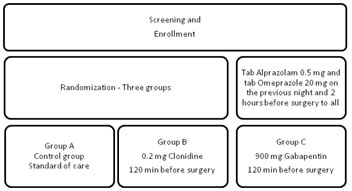
MATERIAL AND METHODS This prospective observational study was carried out by the Department of Ear, Nose and throat of a tertiary care Hospital in southern India, after the approval from the Institutional Ethics Committee (ECR/58/Inst/AP/2013/RR-16). We screened prospective subjects after obtaining a written informed consent. This study focussed on the hemodynamic response to laryngoscopy and intubation in patients undergoing elective surgeries with the primary objective of comparing the effect of Clonidine and Gabapentin as premedication in attenuating hemodynamic responses following laryngoscopy and tracheal intubation in these patients. Selection Criteria: Patients aged 18-60 years (both inclusive) with American Society of Anesthesiologist (ASA) grade I or II were included and those with anticipated or encountered difficult airway, emergency surgeries, with ASA Grade ≥III, those with cardiovascular, renal, hepatic, neurological and endocrine disorders, those on psychotropic drugs or history of drug allergies were excluded. Randomization: Patients were randomly allotted to one of the three groups according to the agents used before the induction of anesthesia (fig 1). Procedure: In the operating room 18 G intravenous (IV) cannula was inserted in an appropriate vein and Ringer’s solution was infused, at a rate of 10 ml/kg/hour throughout the study period. Monitoring tools included an automated BP manometer, electrocardiography and pulse oximetry. Baseline values of Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and heart rate (HR) were recorded. After preoxygenation, anesthesia was induced with thiopentone sodium 5 mg/kg, fentanyl 2 µg/kg and vecuronium 0.1 mg/kg. Patient’s lungs were manually ventilated for 3 min with 50% oxygen and 50% N2O along with 0.4% isoflurane before orotracheal intubation was performed. Direct laryngoscopy was performed 3 min after loss of verbal contact by using a Macintosh 3 laryngoscopy blade, and tracheal intubation was accomplished within 15sec. Patient’s lungs were then mechanically ventilated with a tidal volume of 8-10 ml/kg and a respiratory rate of 12/min to maintain end-tidal PaCO2 at around 35-38mmHg. Anesthesia was maintained with isoflurane and with a fresh gas flow of 4 l/min (50% N2O in O2). In each patient blood pressure (BP) (SBP, DBP, MAP) and Heart Rate were measured: baseline and post-intubation at 1, 3, 5 and 10 min. Hypertension was defined as a MAP >30% of a patient’s baseline value or 130 mmHg whichever was greater. Hypotension was defined as a MAP < 70% of a patient’s baseline value or 65 mmHg, whichever was less. Tachycardia and bradycardia were defined as a HR > 120 beats/min (bpm) and < 60 bpm, respectively. On completion of surgery, the remaining neuromuscular blockade was reversed with neostigmine 0.04 mg/kg and glycopyrrolate 0.01 mg/kg. Patients were observed for possible side effects (such as bradycardia, hypotension, nausea and vomiting, respiratory depression, dizziness, somnolence, peripheral edema and, headache) throughout the procedure. Statistical Analysis: Sample size and Sample technique: In the absence of an accurate outcome of results in the literature, we selected the sample of 30 in each group (total 90) randomly. Statistical analysis was done using independent students t-test to test the difference between the control and study groups. A p-value of <0.05 was considered significant. The means of parameters at different time points for control and study groups individually were tested using repeated measures of ANOVA (one-way analysis). Descriptive statistics, tables, graphs were used as appropriate to describe the results. RESULTSTable 1: Demographic characteristics of the study populaiton
Table 2: Baseline hemodynamic parameters
Figure 1:
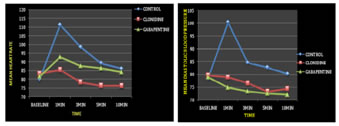
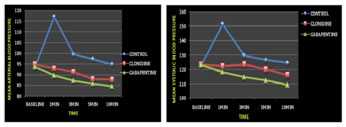
Figure 2 Figure 3 Figure 4 Figure 5 Figure 1: Randomization of patients into study groups.; Figure 2: Attenuation of heart rate in three study groups; Figure 3: Attenuation of systolic blood pressure in three study groups; Figure 4: Attenuation of Diastolic blood pressure in three study groups; Figure 5: Attenuation of Mean arterial pressure in three study groups
Demography: We included 90 patients meeting the selection criteria, grouped randomly into three groups, 30 in each group. There were 49 males and 41 females. Mean±SD age of patients was 40.5±14.9 years, the median being 40 years (range18-60 years). Mean±SD body weight of patients was 53.5±5.3Kgs. Demographic characteristics of each group is tabulated in table 1. Hemodynamic parameters: At baseline: There were no statistically significant changes in the hemodynamic parameters between groups (Table 2). During the procedure: Heart rate: The HR in the control group reached maximum (111.33 beats/min) at 1 min after laryngoscopy and stayed above baseline till 10 min after laryngoscopy and intubation. Heart rate in the study groups reached a maximum of 92.83 beats/min with Gabapentin and 85.53 beats/min with Clonidine at 1 min after laryngoscopy. The lowest HR recorded in Clonidine group was 76.33 beats/min and in Gabapentin group was 84.10 beats/min at 10 min after laryngoscopy. Heart rate differed among groups (p<0.0001), to time between groups (p<0.0001). Clonidine has a greater impact on the heart rate compared to gabapentin (Fig 2). Systolic Blood Pressure: Highest mean SBP 151.33 ±8.47 mmHg was seen in the control group at 1 min after laryngoscopy. The lowest mean SBP 109.36±5.89 mmHg was observed in the Gabapentin group at 10 min after laryngoscopy (fig 3). The SBP differed among group (p<0.0001), to time between groups (p<0.0001). Gabapentin had a significant effect on the SBP compared to other groups. Diastolic Blood Pressure: Highest mean DBP 100.33±6.70mmHg was seen in the control group at 1 min after laryngoscopy. The lowest mean DBP 72.06±5.40 mmHg was observed in the Gabapentin group at 10 min after laryngoscopy (fig 4). The DBP differed among groups (p<0.0001), to time between groups (p<0.0001). Attenuation of DBP was better with gabapentin.Mean arterial pressure: Highest mean MAP 117.11±5.04 (mmHg) was seen in the control group at 1 min after laryngoscopy. The lowest mean MAP 84.50± 3.92 (mmHg) was observed in the gabapentin group at 10 min after laryngoscopy (fig 5). The MAP differed among groups (p<0.0001), to time between groups(p<0.0001). Gabapentin had better control over the increase in the MAP among the study groups.Adverse effects: There was no adverse effect reported in this study.
DISCUSSIONDirect laryngoscopy and endotracheal intubation often lead to increase in BP and heart rate.14 Mechanism of cardiovascular response to intubation is considered to be a reflex sympathetic response to the mechanical stimulation of larynx and trachea. Significant increases in serum levels of norepinephrine and epinephrine after laryngoscopy with and without tracheal intubation have been described.1 Many pharmacological interventions have been suggested to attenuate these reflex responses to laryngoscopy and intubation.2 Gabapentin has emerged as a promising agent in attenuating the hemodynamic responses following laryngoscopy and meta-analysis by Doleman B et al supports this fact.15 Fassoulaki and colleagues in 2006 revealed the efficacy of Gabapentin in attenuating hemodynamic responses following laryngoscopy.11 They showed that pre-treatment with Gabapentin 1600 mg Q6H starting the day (noon) before surgery attenuates the hemodynamic response to laryngoscopy and intubation of the trachea. They emphasized that Gabapentin did not affect HR. SBP and DBP were significantly lower in the Gabapentin group than in the control group (p<0.05) immediately also at 1, 3, 5 and 10 minutes after laryngoscopy. The results of our study showed that, compared with Group A (control group), HR, SBP, DBP, and MAP were significantly lower in both Group B (Clonidine) and C (Gabapentin). The effect of Clonidine on attenuation of the hemodynamic response to the laryngoscopy and tracheal intubation has been reported previously by many studies. Efficacy of Oral Clonidine in attenuating hemodynamic response following laryngoscopy and tracheal intubation was reported by Nishikawa T et al. (5μg/Kg)3 and Matotet al. (300µg).7 We too observed similar results with oral Clonidine (0.2mg). We preferred a dose of 0.2 mg Clonidine as previous studies achieved blunted catecholamine release during intubation and surgery with a dose of 4µg/kg Clonidine and higher doses did not show any better effect. Smaller doses, nevertheless, were not adequate to blunt the reaction to laryngoscopy. Additionally, the maximum dose of Clonidine is limited by its action on peripheral α-adrenoceptors. Larger doses might cause peripheral α stimulation, resulting in increased blood pressure.16-17 Studies have proven the better efficacy of Gabapentin over Clonidine in attenuating the hemodynamic response following laryngoscopy and intubation.18Memiş M et al.15 observed better results with 800 mg of oral gabapentin compared to 400 mg; Bala I et al.19 reported no significant difference in the effect when 800 mg of gabapentin given once compared to twice as a preanesthetic medication to attenuate the pressor effects. Bafna U et al20 observed that Gabapentin (1000 mg) administered an hour before surgery was effective in attenuating the hemodynamic responses following laryngoscopy in normotensives. Based on these, we administered 900mg or oral gabapentin. Agarwal S et al.21 noted that MAP was lower with premedication with Gabapentin; they also caution that it may not have any significant impact on the procedure induced tachycardia; hence, the anesthesiologist and the operating surgeon must be careful in assessment and management. Nanda A et al.22too support the observations of Agarwal S et al. Marashi SM et al.23 compared the attenuating effects of Clonidine and Gabapentin and report that both were effective in their attenuating the hemodynamic responses post-procedure, but response with gabapentin was more impressive. Ayatollahi V et al’s24 report on the use of oral Gabapentin as premedication in microlaryngoscopic surgeries cautions us that only mean arterial pressure is lowered but not SBP, a point to be remembered particularly in those with hypertension. With recent reports supporting the efficacy of Gabapentin25-27 its use as premedication to attenuate the procedure associated pressor response is justified. In contrast, Yadav JBS et al.28 noted better attenuating effects with Clonidine than Gabapentin; Parida S et al.29 too reported that oral Gabapentin alone was not effective in attenuating the hemodynamic effects. Manian K et al.30 demonstrated that a lower dose of oral gabapentin (600 mg) is not effective in attenuating these effects. In a comparative study on Indian patients, oral Clonidine (200 μg) scored over oral Gabapentin (900mg) administered 90 minutes before the anesthetic procedure, in attenuating the pressor effects post procedure.31Kapse UPS et al.32too support this observation on oral Clonidine; they used a slightly higher dose of Clonidine (5μg/Kg) and 800 mg of Gabapentin. Few have found oral Clonidine has better effect than oral Gabapentin.33-35Galat JS et al.36 concluded that both Clonidine (0.2mg) and gabapentin (800mg) as premedication given orally have comparable efficacy in attenuating the pressor response following laryngoscopy and tracheal intubation, with good but similar safety profile; this study did not support the superiority of one agent over the other. Similar observations were reported.37 We observed the highest rate of SBP, DBP, and MAP in the control group especially at one minute after laryngoscopy followed by Clonidine and Gabapentin. Our data also confirmed HR, SBP, DBP, and MAP significantly differed among the groups and to time (p< 0.05). Heart rate was high in the control group followed by Gabapentin and lowest in Clonidine group. As Clonidine also stimulates α-2 adrenergic inhibitory neurons in the medullary vasomotor center, there is a decrease in the sympathetic nervous system outflow from the central nervous system to the peripheral tissues. This causes central and peripheral attenuation of sympathetic outflow and central activation of noradrenergic imidazoline preferring receptors. Decreased sympathetic nervous system activity manifests as peripheral vasodilatation and a decrease in SBP, heart rate. Our result confirms the better effect of Clonidine in attenuating the increase in HR whereas gabapentin on SBP, DBP and MAP. Reports on the safety profile of gabapentin when used as a preanesthetic medication for laryngoscopy and tracheal intubation are limited with most of the studies cited above focussing on the efficacy; Galat JS et al.36 reported good safety profile. None of our patients had hypotension before induction of anesthesia. Also, none of the patients in Group B or Group C exhibited severe hypotension compared with the control group; this observation supports the good safety profile of both agents. The hypotensive effect has been described in other studies in which Clonidine was used either in its IV form or as an oral dose of 4 or 5 mg/kg. In our study, hypotension occurred only during the induction of anesthesia and could be related to the use of thiopentone sodium. There was no case of bradycardia or hypotension among three groups. No ST segment depression or other electrocardiogram changes was noted in either group. Paul A et al.38 report variation in hemodynamic responses with different types of laryngoscope used. Verifying this and correlating with hemodynamic changes would have helped us more in determining the effect of these agents. Our study confirms the comparable efficacy of oral Gabapentin (900mg) and Clonidine (0.2mg), given 120 min before surgery, in blunting the hemodynamic response to laryngoscopy and endotracheal intubation, with significant differences between the groups in the first 10 min post-laryngoscopy. Gabapentin is preferred to Clonidine as premedication due to fewer side effects such as bradycardia and adverse drug interactions compared to Clonidine. The potentially beneficial effect of α2 agonists may be counteracted by bradycardia and hypotension. Our results suggest better control of hemodynamic responses following laryngoscopy and tracheal intubation, lesser drug interactions and no significant variation in heart rate from baseline values with gabapentin compared to Clonidine.
CONCLUSION Gabapentin 900mg and Clonidine 0.2 mg orally as premedication 120 min before surgery are effective in blunting hemodynamic response to laryngoscopy and endotracheal intubation in the study population. REFERENCES
|
|
 Home
Home