Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 1 - January 2018
Correlation between LDH isoenzyme and lipid profile on the development of ischemic heart disease
Madhu Sinha1*, Yogesh Krishna Sahay2, Moumita Goswami3
1Associate Professor, 2Assistant. Professor, 3PG Student, Department of Biochemistry, Anugrah Narayan Magadh Medical College, Gaya, Bihar, INDIA. Email: madhusinha03@gmail.com
Abstract Background: In studying patients with myocardial infarction we found a high serum lactic dehydrogenase (LDH) but a normal serum isocitric dehydrogenase (ICD) although the myocardium is rich in both enzymes. For elevations to occur, the equilibrium between the rate of enzyme elimination and the rate of entry from the blood must be disturbed, but there is no explanation of why certain enzymes do not increase when their tissue of origin is damaged. Method: It was observational, and case control study to Correlation between LDH isoenzyme and Lipid Profile on the development of Ischemic heart disease. This study was conducted in the Department of Biochemistry and Medicine OPD, in Anugrah Narayan Magadh Medical College, Gaya. Bihar. The duration of study was from September 2016 to October 2017. 50 cases of high risk group e.g.: H/O diabetes, AMI, Hypertension (HT), Smoker, sedentary lifestyle was studied at the Out Patient Department of Medicine. 50 normal cases were studied as well. And both the control and cases are compared and studied, routine diagnostic procedures were based on history, medical examination, serial standard 12-lead ECG and laboratory tests described. Result: Densitometric study of isolated LDH isoenzyme done for detection of percentage of LDH1 to LDH5 in total LDH value. PAGE analysis of LDH isoenzyme in cases as soon majority had an alteration in LDH4 isoenzyme. There are some cases with HT depression also has got lipid profile alteration which may be indication of ongoing atherosclerosis. Most of the patients having increased LDH level (specially LDH4) with altered Lipid profile which may be the cause of IHD because most of the cases having increased LDH4 level has hypercholesterolemia and increased Tg level, has changes in ECG showing ischemic heart disease which may proceed to permanent cardiac damage. Conclusion: Proper management and regular check up can prevent myocardial infarction. Routine check-up can be done as blood and physical examination. So along with blood and ECG LDH isoenzyme analysis may be helpful to prevent the occurrence of MI in these cases. Key Words: Hypertension, Lactic dehydrogenase, Ischemic Heart Disease, LDH isoenzyme.
Heart disease, along with malignancies, are the top two causes of death in developed countries. In the United States approximately 25 % of all deaths occur because of cardiac diseases. This is equivalent to 610,000 deaths each year from heart disease1 Sixty-one percent of the deaths, or 370,000 events, are due to coronary heart disease (CHD).1 that is caused by cholesterol plaque build-up with consequent narrowing of the coronary arteries. This is known as coronary artery disease (CAD). When this plaque ruptures it activates the coagulation cascade locally and the developing thrombus restricts or completely stops blood flow to the cardiac muscle downstream from the occlusion, causing the clinical conditions known as angina and heart attack (myocardial infarction). According to the 2013 US national statistics, the 370,000 deaths per year are the consequence of approximately 735,000 heart attacks of which about one third (1/3) are recurrent events [1]. Based on population statistics it can be calculated that approximately 310 heart attacks per hundred-thousand people older than 18 years of age and approximately 150 deaths per hundred-thousand adults can be expected each year in developed nations. The number of people with heart disease and the death rate from CHD varies between sexes, racial groups and geographic region within a country and it increases with increasing age even within the same country, but CHD and heart attack are large public health issues and consume large amounts of health care dollars. As the severity of consequences of a heart attack increases with each minute of delay in diagnosis and treatment, early diagnosis is mandatory to minimize long term sequelae of an acute coronary event. For many people the first sign of having CHD is chest pain, caused by heart attack, but others may learn about their CHD from their doctor after receiving results of laboratory tests as part of their annual check up. Diet, smoking, presence of diabetes, hypertension or hyperlipidemia, among other things, can help estimate one's chance of having CHD or CAD, therefore measurement of blood pressure, cholesterol, blood sugar, body weight and body mass index as well as obtaining relevant medical history to collect information about one's diet, exercise and smoking habits can be the first steps of working up a patient for possible presence of CAD. If it appears that one is at high risk for CAD, additional tests can be performed using a variety of diagnostic procedures consisting of electrocardiogram (ECG or EKG), echocardiogram, exercise test, cardiac catheterization and coronary angiogram. During an acute chest pain event the concentration of biochemicals can be measured in one's blood to asses if the person's CAD has progressed into a heart attack or if the chest pain is due to some other disease entity than coronary artery closure. The laboratory markers used in the diagnosis and differential diagnosis of acute chest pain are collectively called cardiac markers, myocardial injury markers or biochemical markers of myocardial injury. This article will present a brief overview of the most significant cardiac markers and it will discuss the use of those markers for the diagnosis of cardiac diseases but it will not talk in details about the non-laboratory diagnostic modalities. LD activity is present in all cells of the body with highest concentrations in heart, liver, muscle, kidney, lung, and erythrocytes. As with other proteins used as tissue-function markers, the appearance of LD in the serum occurs only after prolonged hypoxia and is elevated in a number of clinical conditions including cardiorespiratory diseases, malignancy, hemolysis, and disorders of the liver, kidneys, lung, and muscle. LD is a tetrameric cytoplasmic enzyme, composed of H and M subunits. The usual designation of the isoenzyme is LD-I (H4), LD-II (H3M), LD-III (H2M2), LD-IV (HM3), and LD-V (M4). Tissue specificity is derived from the fact that tissue-specific synthesis of subunits occurs in well-defined ratios. Most notably, heart muscle cells preferentially synthesize H subunits, while liver cells synthesize M subunits nearly exclusively. Skeletal muscle also synthesizes largely M subunits so that LD-V is both a liver and skeletal muscle form of LD. The LD-I and LD-V forms are most often used to indicate heart or liver pathology, respectively. LD-I appears elevated in the serum about 24 to 48 hours after a myocardial infarction (MI), but is generally not as useful as troponin or creatine kinase-MB (CK-MB) for detection of MI, unless the MI occurred at least 24 hours prior to testing. Normally, LD-II is greater than LD-I; however, when a MI has occurred, there is a "flip" in the usual ratio of LD-I/LD-II from less than 1 to greater than 1 (or at least >0.9). Use of the ratio for evaluation of patients with possible cardiovascular injury has largely been replaced by TPNT / Troponin T, Serum. The LD-V form is pronounced in patients with either primary liver disease or liver hypoxia secondary to decreased perfusion, such as occurs following an MI. However, LD-V is usually not as reliable as the transaminases (eg, aspartate aminotransferase, alanine aminotransferase) for evaluating liver function. LD-V also may be elevated in muscular damage and diseases of the skin. Although it does not appear to cause or be associated with any symptoms or particular diseases, the presence of macro-LD (LD combined with an immunoglobulin) can cause an idiosyncratic elevation of total LD. Type of Study: Case- control study. Study Area: This study was conducted in the Department of Biochemistry and Medicine OPD, in Anugrah Narayan Magadh Medical College, Gaya. Bihar. The duration of study was from September 2016 to October 2017. Eligibility of the study population: 50 cases of high risk group e.g.: H/O diabetes, AMI, Hypertension (HT), Smoker, sedentary lifestyle was studied at the Out Patient Department of Medicine. 50 normal cases were studied as well. And both the control and cases are compared and studied, routine diagnostic procedures were based on history, medical examination, serial standard 12-lead ECG and laboratory tests described. Electrocardiography: Electrocardiography was performed. The following definitions were used: ST-T wave abnormalities= ST segment deviation (ST segment depression->0.1 mV or elevation ->0.1 mV in limb leads or 0.2 mV in periodical leads) QRS complex broader on the ECG; uncodable ECG= poor quality or the presence of suppression codes (i.e. bundle branch block, artificial pacemaker, complete atrioventricular block). The ECGs were evaluated independently. Tools and Technique: Sample Collection: Blood samples were collected in three types of vial. (Clot, EDTA, Fluride vial) All the biochemical parameters were performed in semi automated analyzer and Vertical Electrophoeresis machine. Samples were collected for estimation of: The serum levels of Lactate Dehydrogenase, LDH isoenzyme, Lipid Profile, Bilirubin, SGOT, Urea Creatinine and blood glucose and glycosylated Hb levels were determined for all samples. All tests were done on semi auto analyzer. Strict external quality control using sera with known values will be performed to validate the results.
Inclusion Criteria The patients attending the OPD of Medicine who have high risk history for developing ischemic heart disease and coronary artery disease in future (Such as Hypertension, diabetes, H/O of AMI, smoker, sedentary life etc.) Exclusion Criteria The patients were excluded from the stud:
Statistical analysis was done by SPSS software version 10.
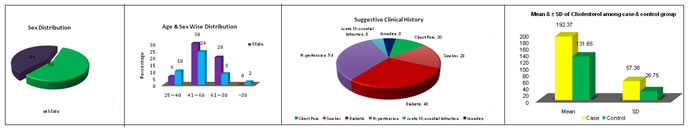
RESULTS Table 1: Sex Distribution
Table 2: Age and Sex Wise Distribution
Table 3: Suggestive Clinical History
Table 4: Mean and± SD of Cholesterol among case and control group
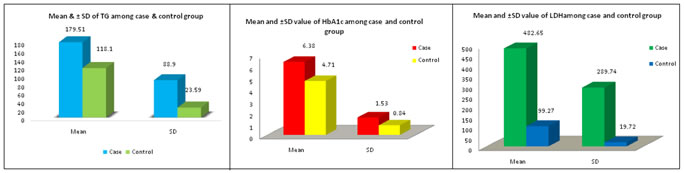
Table 5: Mean and ±SD of TG among case and control group
Table 6: Mean and ±SD value of HbA1c among case and control group
Table 7: Mean and ±SD value of LDH among case and control group
Figure 1 Figure 2 Figure 3
Figure 4
Figure 5 Figure 6 Figure 7 Legend Figure 1: Sex Distribution; Figure 2: Age and Sex Wise Distribution; Figure 3: Suggestive Clinical History; Figure 4: Mean and± SD of Cholesterol among case and control group; Figure 5: Mean and ±SD value of TG among case and control group; Figure 6: Mean and ±SD value of HbA1c among case and control group; Figure 7: Mean and ±SD value of LDH among case and control group
In general serum total LDH is significantly increased in cases with respect to control. In general serum total LDH activity is significantly increased in cases with respect to control. There is change in isoenzyme pattern from normal. After doing PAGE it is seen that among all LDH isoenzyme the LDH 4 is increased which is corporate by densitometer study. The value of LDH4 fraction was increased from its normal percentage (i.e. 3-8%) to 10-25% which is highly significant. Lipid profile analysis shows 40 patients had increased cholesterol level among 50 patients (Mean 192.37) and triglyceride (Mean 179.5) but HDL and LDL level are not significantly changed from normal value. ECG changes in more cases are ST depression i.e. in 28 patients among 50 cases.
DISCUSSION The patients thus selected has undergone Blood tests for fasting blood glucose, urea, creatinine, cholesterol, triglyceride, HDL, LDL, VLDL, total bilirubin, direct bilirubin, SGOT, HbA1c and LDH. LDH assay by PAGE method and quantification by densitometer was done. ECG of all cases was done. Lactic dehydrogenase which is present in all living cells, plays an important role in glycolysis by catalyzing the reversible conversion of lactate to pyruvate, producing in the process a molecule of' reduced DPN. Most workers believe there are five electrophoretically distinct molecellar forms of LDH otherwise known as isoenzymes. Each of the five isoenzymes is a tetramer: that is it is composed of fou' subunits. These four sub units are of two basic types: the n M II or muscle-liver unit and the "H" or heart unit. LDH-I and LDH-5 are homogeneous, containing four II M II and four “R" units, respectively, whereas LDH-2, LDH-3, and LDH-4 are combinations of the two basic subunits. The techniques used for identifying the LDH isoenzymes have included the electrophoretic rate of migration in solid media and the relative heat ~bility. Electrophoretic demonstration of isoenzyme activity is accomplished by conversion of neotetrazolium to purple formazin by LDH production of DPNH. Nomenclature is basea upon electrophoretic migration rates, with the form having the highest mobility toward~ the anode being designated as LDH-I. Thus, the hea.rt fraction is LDH-l and the slowest or liver and skeletal muscle fraction is LDH-5. LDH-l is more heat stable than the other isoenzymes. This property gives rise to a heat stab1e test for isoenzymes which affords separation of LDH activity into three categories:LDE-l; L:!2H-2,3,1+; and. LDH-5. Densitometric study of isolated LDH isoenzyme done for detection of percentage of LDH1 to LDH5 in total LDH value. PAGE analysis of LDH isoenzyme in cases as soon majority had an alteration in LDH4 isoenzyme. LDH4 is an isoenzyme for kidney and pancreas so rise in LDH4 isoenzyme indicates that the group of cases had developed some degenerative changes in pancreas and kidney. It is not clear here whether these are the cause of effect of diseases. From analysis of ECG changes it is being observed majority of cases with alteration of LDH isoenzyme pattern (LDH4 fraction) has ST depression changes in ECG. ST depression in ECG is an indication of ischemic heart disease. So the cases had already developed some sort of ischemia. It is also not clear whether the ischemia has got a relationship with change in isoenzyme pattern. But ischemic changes in cases should have routine check up which should be enhanced if there are associated isoenzyme pattern changes. There are some cases with HT depression also has got lipid profile alteration which may be indication of ongoing atherosclerosis. Most of the patients having increased LDH level (specially LDH4) with altered Lipid profile which may be the cause of IHD because most of the cases having increased LDH4 level has hypercholesterolemia and increased Tg level, has changes in ECG showing ischemic heart disease which may proceed to permanent cardiac damage. The association of cholesterol, LDH4 isoenzyme and ST depression in ECG, they may have potentially at risk of developing myocardial infarction.
CONCLUSION Proper management and regular check up can prevent myocardial infarction. Routine check-up can be done as blood and physical examination. So along with blood and ECG LDH isoenzyme analysis may be helpful to prevent the occurrence of MI in these cases.
REFERENCES
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home