Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 2 - November 2018
K Veera Sudhakar1, B Ravindra Reddy2*, J Dineesh3, B V Surendra4
{1,2Assistant Professor, 3Professor, Department of Biochemistry} {4Assistant Professor, Department of Physiology} Viswabharathi Medical College, R.T. Nagar, Penchikalapadu, Kurnool-518463, INDIA. Email:bobre123@gmail.com
Abstract Background: Type 2 Diabetes Mellitus is associated with a marked increased risk of Cardiovascular Disease (CVD). Such risk of Cardiovascular disease can be attributed to diabetic dyslipidemia. Dyslipidemia is one of the common disorders which is observed in most of the diabetes patients, which causes cardio vascular disorders. This study is aimed at evaluating the lipid profile of type 2 diabetics and comparing the lipid profile of type 2 Diabetes males and females attending a tertiary hospital. Objective: To detect the lipid abnormality in type-2 Diabetic patients and compare the lipid profile of type 2 Diabetes males and females Methods: A total of 60 consenting type II diabetic patients comprising 30 Males and 30 Females aged 40-70 years were studied. Total Cholesterol (TCHOL), Triglycerides (TRG), High Density Lipoproteins (HDL-C), and Low Density Lipoproteins (LDL-C) levels) were analyzed for each group. Data was analyzed using unpaired t tests. Significance was set at p<0.05. Results: The mean values of TC, VLDL-C and LDL-C were higher and HDL-C was lower than the normal in T2DM patients. Comparison between males and females showed significantly higher TG, TC, LDL-C and lower HDL-C in T2DM females than males. Conclusions: This study noted the presence of dyslipidemia in T2DM population which is major risk factor for CVD. High LDL-C and low HDL-C was observed in T2DM females compared to T2DM males suggests higher risk for CVD in females compared to males Key Words: Type 2 Diabetes; Lipid profile; Dyslipidemia; Cardiovascular disease (CVD).
INTRODUCTION Diabetes Mellitus is a disorder associated with chronic hyperglycaemia resulting from complete or partial decrease in insulin secretion or decrease in biological action of insulin or both1. A variety of interrelated lipid and lipoprotein abnormalities is known to be associated with T2DM commonly termed as diabetic dyslipidemia2. Dyslipidemia is one of the major risk factor for cardiovascular disease in Type 2 Diabetes mellitus, characterized by elevated Total cholesterol (TC), Triglycerides (TG), Low density lipoprotein (LDL) and decreased High density lipoprotein (HDL)3. Because detection and treatment of dyslipidemia is one means of reducing Cardiovascular Disease (CVD) risk, determination of serum lipid levels in people with diabetes is now considered a standard of care4. Patients with type-2 diabetes have increased risk of cardiovascular disease associated with atherogenic dyslipidemia. Coronary artery disease, especially myocardial infarction is the leading cause of morbidity and mortality worldwide5. Hyperglycemia and atherosclerosis are related in type-2 diabetes6. The term diabetic dyslipidemia comprises a triad of raised triglycerides, reduced high density lipoprotein (HDL) and excess of small, dense low density lipoprotein (LDL) particles. The lipid abnormalities are prevalent in diabetes mellitus because insulin resistance or deficiency affects key enzymes and pathways in lipid metabolism7. It has been proposed that the composition of lipid particles in diabetic dyslipidemia is more atherogenic than other types of dyslipidemia8 In Jamaica population greater TC was observed in hypertensive T2DM females compared with hypertensive T2DM males9. In Saudi Arabia also female patients showed higher serum TC and lower HDL-C in comparison with male patients, whereas LDL-C and TG values were significantly increased in females compared with male T2D patients. Atherogenic incidences were also higher in female than those for males with T2DM10. Present study was conducted to identify the risk of dyslipidemia in T2D patients and to analyze the effect of sex on lipid abnormalities in T2D patients in a tertiary hospital, Kurnool.
.MATERIALS AND METHODS Study area and design: The study was carried out at Viswabharathi Medical College and general hospital, Kurnool which is in the Rayalaseema region of Andhrapradesh and was conducted in the Central Biochemistry laboratory of the hospital. A cross-sectional non-probability sampling method was adopted after patient’s consent had been taken. Ethical considerations: The study was approved by the ethical committee. Informed consent was obtained from all study participants who duly acknowledged by agreeing to the study. Patients selection and exclusion criteria: The study was conducted on medically diagnosed Type II Diabetes Mellitus male and female patients between 40 and 70 ages on diabetic treatment schedule to visit the hospital at regular intervals for routine medical review using the non-probability sampling method. Type II Diabetic pregnant women and patients on statins for abnormal lipid treatment were excluded. Sample collection and storage: Five ml venous blood sample was collected from antecubital vein of each of the diabetic patients in a metal-free sterile tube, between 7 and 8 AM after an overnight fasting. The blood was then allowed to clot at room temperature for 30 min and centrifuged at 3000 rpm for 15 min to extract the serum. The serum was taken in eppendorf tube and stored at −20 °C until analysis. Blood collection and serum separation were carried out in a dust-free environment. Measurement of biochemical parameters: Fasting glucose level was determined by Glucose Oxidase–Peroxidase method, Total cholesterol is measured by enzymatic method CHOD-PAP (Cholesterol Oxidase-Peroxidase 4- aminoantipyrine) in semiautoanalyzer using commercially available kit. Serum HDL-c is measured by enzymatic method after precipitation with polyanions in a semiautoanalyzer using commercially available kit. Friedewald Formula was used to calculate serum LDL-C. LDL cholesterol mg/dl = Total cholesterol – [HDL Cholesterol + Triglycerides/5] [10].Serum triglycerides is measured by enzymatic method GPO-ESPAS (Glycerol 3 Phosphate Oxidase- Peroxidase N-Ethyl-N-Sulfopropyl-n-anisidine) using commercially available kit in semi autoanalyser. Statistical analysis: Data was analyzed by SPSS software package (version 16.0). Values were expressed as mean ± SD. Comparison of data between male Diabetic and female Diabetic patients was performed by unpaired t test. P values < 0.05 was considered statistically significant.
OBSERVATIONS AND RESULTS
Table 1: Gender distribution and age of patients with type 2 diabetes
Table-I gives information about age of Male and Female type-2 Diabetic patients. The mean age of male diabetic patients is 56 years and mean age of female type-2 Diabetic patients was 55 years.
Table 2: The concentration of Fasting Blood Glucose in Diabetic patients
Table-2 gives information about the concentration of fasting blood glucose in male and female diabetic patients. The mean concentration of fasting blood glucose in males is 147.6 mg/dl and mean concentration of blood glucose in females is 167.2 mg/dl. It is observed that fasting blood glucose concentration is more in females than males.
Table 3: Comparison of results of TC, HDL-C, LDL-C,, and TG concentrations in type 2 Diabetic Males and Females
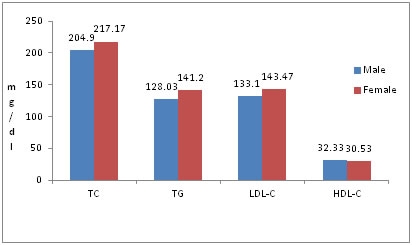
As shown in table-3 Diabetic patients have more T.C, T.G, LDL-C, less HDL-C than the normal range and comparison of lipid profiles of male and female T2D groups showed significant higher TC, TG,LDL-C values and significant lower HDL-C in T2DM females than males. This study supports the presence of dyslipidemia among type-2 Diabetic patients and significant difference of dyslipidemia among males and females by having more TC, TG,LDL-C and less HDL-C values in females and indicates the higher risk of CVD in females compared to males with T2DM.
Figure 1: Concentrations of TC, TG, LDL-C, HDL-C in type-2 diabetic male & female patients
DISCUSSION Diabetes Mellitus is associated with a greater risk of morbidity and mortality from cardiovascular disease. Detection and treatment of dyslipidemia in diabetes is one major step towards reducing the risk of cardiovascular disease associated with diabetes11. Altered lipid profile in T2DM is due to insulin resistance and defective insulin action on lipoprotein metabolism. Increased lipolysis will increase the synthesis of VLDL and triglyceride rich LDL-c. It will also increase triglyceride synthesis and promote quick breakdown of HDL-c12 Insulin affects the liver apolipopro-tein production. It regulates the enzymatic activity of lipoprotein lipase (LpL) and Cholesterol ester transport protein. All these factors are likely cause of dyslipidemia in Diabetes mellitus13. Moreover, insulin deficiency reduces the activity of hepatic lipase and several steps in the production of biologically active LpL may be altered in DM14.Insulin resistance in T2DM increases the free fatty acid flux to the liver which increases the TG synthesis in hepatic cells in turn causes the elevation of VLDL-C concentration17. Increased VLDL-C results in change of lipoproteins and causes elevation of small dense LDL-C and decreases HDL-C and apolipoprotein A-I.15,16 Reduction in the concentration of HDL-C and apolipoprotein A-I results in the accumulation of the cholesterol in blood vessels which increases the risk of atherosclerosis.16 Increase in the small dense LDL-C further increases the apolipoprotein B and are more tending to transfer into the arterial wall in T2DM patients18.Hy-perlipidemia in females may be attributed to the effects of sex hormones on body fat distribution, which leads to differences in altered lipoproteins19.This study reveals high prevalence of hypercholes-terolemia, hypertriglyceridemia, high LDL-C and low HDL-C levels which are well known risk factors for car-diovascular diseases in females compared to males. Thus this study extend earlier studies of sex-related differences of lipid profile20,21,22. Significantly more numbers of female diabetics were having dyslipidaemia than males. Elevated levels of total cholesterol, triglycerides, LDL cholesterol were more frequent in women compared to men.. Women have significantly different lipoprotein profiles than men regardless of menopausal status. Gender affects lipid parameters and this effect is independent of age and menopausal status. Presumably these differences are due to the different levels of circulating sex hormones, specifically estrogens and androgens in women versus men23,24.
CONCLUSION This study demonstrated the existence of dyslipidemia in T2DM male and female patients. High LDL-C, TG and low HDL-C indicate the risk for CVD in T2D patients. Whereas, in males and females, different CVD risk patterns were observed. In females increased T.C, T.G, LDL-C and decreased HDL-C was observed. Since higher LDL-C and decreased HDL-C was linked with severe CVD, risk of CVD will be expected more in females than the males.
REFERENCE
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home