|
Table of Content - Volume 4 Issue 1- October 2016
A Study of various complications among type II diabetic patients at rural tertiary heath care center
Mithun Somaiah C S
Assistant Professor, Department of General Medicine, BGS Global Institute of Medical Sciences, No. 67, BGS health and Education city Uttarahalli road, Kengeri, Bengaluru, Karnataka- 560060, INDIA.
Abstract Background: The present situation about diabetes makes it all the more important that we make attempts to understand the prevalence of these complications and possible risk factors in order to develop potential preventive programmes. Aims and Objectives: To Study various complications among type II Diabetic patients at Rural tertiary heath care center. Methodology: After approval from institutional ethical committee, a cross-sectional study was carried out in patients who were admitted to Sri Adichunchanagiri hospital and research center, B.G. Nagara, Mandya attached to Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya. From the patients admitted, 50 cases with H/O Type 2 diabetes mellitus were taken as subjects for the study. Analysis of variance (ANOVA) has been used to find the significance of study parameters between three or more groups of patients, Student t test (two tailed, independent) has been used to find the significance of study parameters on a continuous scale between two groups( Inter group analysis) on metric parameters. Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups. Result: The most common complication was Retinopathy i.e. 42% followed by Neuropathy 34%, Nephropathy 14%, Cardiovascular in 18%, Cerebrovascular Accidents 4%. In Insulin treatment group Retinopathy and Cardiovascular complications were more common (54%), followed by OHA was having Neuropathy 38.2%, Insulin+ OHA was having CVS -80% and Retinopathy 60% was more common. The commonest complication among males was retinopathy with an incidence of 52.9%, followed by IHD (41.2%). The commonest complication among females was peripheral neuropathy (25%) and IHD (25%). There was not much variation seen among the parameters irrespective of the duration of diabetes. Conclusion: It can be concluded from our study that the most common complication was Retinopathy, followed by Neuropathy and Nephropathy. In Insulin treatment group Retinopathy was common followed by OHA was having Neuropathy, Insulin+ OHA group was having Cardiovascular complications like MI, Retinopathy. The commonest complication among males was retinopathy with an incidence, followed by IHD. The commonest complication among females was peripheral neuropathy and IHD. Key Words: Type II Diabetes, Complications of Diabetes, Neuropathy, Nephropathy, Retinopathy.
Diabetes mellitus is one of the most important non-communicable disease of public health concern today 1. According to the International Diabetes Federation (IDF), the estimates of diabetics in India in the 2015 was 69.2 million, which is predicted to rise to 123.5 million by 2040, next only to China. The same atlas also reported national prevalence as 8.7% (7.0 - 10.6) and 1,027,911.6 diabetes related deaths in the 20-79 year age group 2. There are 350 million people with diabetes worldwide and the numbers are expected to double in the next 20 years. It is with this in mind that the World Health Organisation has declared ‘beat diabetes’ as the central theme for World Health Day 2016 3. At the most humble estimates India is projected to spend 4.8 billion USD in 2030 on diabetes accounting for 11% of health expenditure, which will be a considerable burden on a country already battling with tuberculosis, malnutrition, infant and maternal mortality superimposed on poverty 7. A large amount of this will be spent on direct costs like drugs and management of chronic debilitating complications of diabetes 8, 9. The present situation makes it all the more important that we make attempts to understand the prevalence of these complications and possible risk factors in order to develop potential preventive programmes.
MATERIAL AND METHODS After approval from institutional ethical committee a cross-sectional study was carried out in patients who were admitted to Sri Adichunchanagiri hospital and research center, B.G. Nagara, Mandya attached to Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya. From the patients admitted, 50 cases with H/O Type 2 diabetes mellitus were taken as subjects for the study. Age and sex matched 50 Non-diabetic were taken as controls. The diagnosis of Diabetes is based on revised criteria according to consensus panel of experts from National Diabetes Data Group and WHO. Patients with Type 2 diabetes mellitus of more than 40 years of age, Duration of Diabetes more than 4 years were included into study while The control group consists of non diabetics more than 40 years, who are normotensive, who do not have concomitant diseases or other conditions or use drugs that affect lipid levels. Type -2 diabetes patients with concomitant diseases or condition affecting the lipid levels liken hypothyrodism, on lipostatic drugs, thiazides etc and Age below 40 years were excluded from the study. A detailed history and careful physical examination was done alongside Routine Blood and Urine examination. Biochemical analysis for Fasting and post prandial blood sugar, Fasting sample for Serum Triglycerides, Total Cholesterol, HDLc, LDLc, VLDLc, The lipid and lipoprotein assay was done using Dr. Lange LP 700 equipment, Total cholesterol-CHOD - DAP method, Total Triglycerides-GPO - DAP method, HDL cholesterol (HDL - C)-Enzymatic estimation, LDL Cholesterol estimation-LDL = Total cholesterol – HDL – Serum Triglyceride/5, VLDL Cholesterol-its concentration can be approximated by dividing the amount of plasma triglycerides by 5 described by Friedewald in 1972. All the complications with respect to various parameters were noted. Statistical Analysis was done by Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5 % level of significance. Analysis of variance (ANOVA) has been used to find the significance of study parameters between three or more groups of patients, Student t test (two tailed, independent) has been used to find the significance of study parameters on a continuous scale between two groups (Inter group analysis) on metric parameters. Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups.
RESULT
Table 1: Distribution of Complications in patients studied
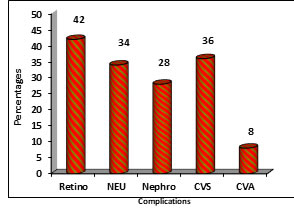
The most common complication was Retinopathy i.e. 42% followed by Neuropathy 34%, Nephropathy 14%, Cardiovascular in 18%, Cerebrovascular Accidents 4%.
Figure 1: Distribution of Complications of patients studied
Table 2: Distribution of complications with Therapy of patients studied
From above Table In Insulin treatment group Retinopathy and Cardiovascular complications were more common (54%), followed by OHA group having Neuropathy as a complicationat 38.2%, Insulin+ OHA group having CVS complications at 80% and Retinopathy (60%).
Table 3: Distribution of complications with Therapy of patients studied according to gender
This table shows the distribution of associated complications among male and female subjects. The commonest complication among females was retinopathy with an incidence of 52.9%, followed by IHD (41.2%). The commonest complication amongmales was peripheral neuropathy (25%) and IHD (25%).
Table 4: Distribution of complications with Therapy of patients studied according to duration
This table shows a co-relation between the various parameters of the lipid profile and the duration of diabetes mainly categorized as more than 7 years and less than 7 years. There was not much variation seen among the parameters irrespective of duration of diabetes.
DISCUSSION Macrovascular complications mainly involve coronary artery diseases atherosclerosis and peripheral vasculopathy. Several clinical studies including diabetes control and complications Trial (DCCT) and the UKPDS33 have shown that the severity of these complications are directly associated with hyperglycemia regardless of the different pathogenesis of type 1 and type 2 diabetes. Macrovascular disease is not specific to diabetics although occur more frequently, more aggressively and earlier in diabetics than in non diabetics. The effect of diabetes on macrovascular disease is related to the elevated plasma LDL, cholesterol and VLDL levels. Data indicate that approximately 75% of deaths in diabetics is accounted due to macrovascular disease. There is free radical production in diabetes, which results in irreversible damage to collagen in arterioles. Long tern poor control of diabetes can cause non-enzymatic glycation of tissue components and glycation of apoliopoproteins result in defective binding of apo B 100 and E to LDL receptor and this inturn further increases the serum lipid levels. There is now clear evidence from the UKPDS 33 and the Kumamoto study that improved glycemic control through intensive diabetes management delays the onset and significantly retards the progression of macrovascular complications in Type 2 Diabetes Mellitus. Coronary Artery Diseases: The major cause of mortality and morbidity in diabetics is macrovascular artherosclerosis. There is a positive association between CAD and elevated total cholesterol and LDLc and negative associations with HDL in both diabetic and non-diabetic individuals. Raised levels of triglycerides and VLDL are associated with both types of diabetes and represent an independent risk factor for macrovascular disease within the diabetic patients. Attention has recently been focused on lipoprotein (a) and its protein component apo A. Lp (a) possesses both thrombotic and atherogenic properties. Studies show that Lp (a) is associated with an increased risk of cardiovascular disease6 and may be an independent risk factor. Bell found that death from CHD was 40% higher in diabetics than non-diabetics and such deaths tend to occur in younger population.7 In WHO multinational study cardiovascular disease accounted for 44% deaths in type 1 and 52% in type 2 diabetes mellitus.8The results from the UKPDS are reassuring in that, although intensive treatment with insulin was associated with increased at gain and hypoglycemia, there is no evidence of any harmful effect of insulin an cardiovascular outcomes, which has been a controversial issue. Several evidences have contributed to our current understanding of the relationship between increase in plasma cholesterol and development of CHD. Premature atherosclerosis results from high cholesterol levels,9 even in the absence of other cardiovascular risk factors. The onset of atherosclerosis occurs early in life with diffuse regular thickening of the arterial intima in childhood. The smooth appearance of the arterial tree is usually lost during the teenage years with formation of nodular aggregates or cushions of fibro-elastic tissue, termed fatty streaks.10 Fatty streaks are collections of lipid, mainly cholesterol esters in macrophages and smooth muscle cells deposited in the intima of the artery. These fatty streaks are the precursors of the hallmark of atherosclerosis, the fibrous atheromatous plaque. The fibrous plaques are white lesions that usually protrude into the vessel lumen and consists of a core of cholesterol, cholesterol ester, phospholipid and necrotic cells covered by a fibrous cap of elastin and collagen. There is also proliferation of the smooth muscle cells into the media. Another important component is the foam cells, which contain a large quantity of lipid.11 Another important predictor of cardiovascular risk is HDL level. The cholesterol content of HDL is relatively small fraction of plasma cholesterol (20-25%). This fraction is inversely related to cardiovascular risks HDL decreases, the risk of CHD increases and vice-versa. In the Framingham study, average HDL level in middle aged men was 45 mg/dl and 55 mg/dl in the female counterparts. The relationship between high triglyceride and CHD remams controversial. Some patients with hypertriglyceridemia are at increased cardiovascular risk others are not. However epidemiological studies suggest that the increased risk seen be due to lither risk factors such as obesity, low HDL and hypercholesterolemia. Hypertriglyceridemia also maybe a marker of an individual with a genetic defect of lipoprotein metabolism, such as accumulation of VLDL remnants which are associated with premature atherosclerosis. An important factor for the development of atheromatous plaques is oxidized LDL, which causes increased chemotaxis of monocytes, and increased uptake of oxidized LDL by macrophages.12 Cerebrovascular Disease: The several fold increased risk of cerebrovascular disease with diabetes can be explained by the independent effects of diabetes and the concurrence of hypertension. Peripheral Vascular Disease: The prevalence of peripheral vascular disease is increased in diabetes and is related to the independent effect of diabetes and other risk factors such as hyperlipidemia, cigarettes smoking and hypertension. It is characterized by a gradual reduction in blood flow to one or more limbs secondary to atherosclerosis. Bell observed that gangrene of lower extremities was about 40 times more common in diabetics as compared to non-diabetics.13 Microvascular complications in diabetes: Microangiopathy is a disorder specific to diabetes that affects small vessels. Microangiopathic lesion impairs nutrition of tissue which could interfere with development of collateral circulation. In addition the lesion could intensify the atherosclerotic process by increasing the intraluminal pressure. It is clinically apparent in the eyes (retinopathy), kidneys (nephropathy) and vasa nervosum of peripheral nerves (neuropathy). The microvascular complications are the most specific and long term complications of diabetes. Diabetic Retinopathy: Diabetic Retinopathy is considered as the hallmark of diabetes, more than 25% of all diabetes suffer from any one of the microvascular complications, either retinopathy or nephropathy. Diabetic retinopathy is the most frequent cause of blindness among adults, particularly in the working age group in the developing countries. Indian studies on this subject reveals that the prevalence of retinopathy among type 2 diabetes range between 7.0% - 34.0 %. In a large population based study showed the over all prevalence of diabetic retinopathy in Urban South Indians was 17.6%.4 This is much lower than that reported in Europeans. The prevalence of diabetic retinopathy at onset of diabetes also appears to be lower in Indians.15 Diabetic retinopathy may have a familial aggregation.16 There appears to be a strong correlation between duration of diabetes and retinopathy in type-1 diabetes. Three other variables associated are long term glycemic control, serum triglyceride levels and age.17 Diabetic Nephropathy: Lipoprotein abnormalities are strongly associated with diabetic nephropathy. Diabetic patients with microalbuminuria have raised levels of total cholesterol, LDL and triglycerides and lower concentrations of HDL. This usually presents as microalbuminuria and hypertension, then progresses to nephritic syndrome and chronic renal insufficiency.18 The presence of nephropathy in type-1 and type-2 diabetes increases the risk of mortality in comparison with diabetics who do not develop this complication. This increase can be attributed to cardiovascular disease. This excess risk is related to lipoprotein abnormalities and the increased prevalence of hypertension found in association with nephropathy.19 In patients with type-2 diabetes with proteinuria the risk of developing cardiovascular death is high. Diabetic nephropathy is the most common for over 40% of new causes.20 Further patients with diabetes mellitus account for more than one third of all cases of End Stage Renal Disease. About 20-30% of subjects with Diabetes have microalbuminuria.20 Diabetic Peripheral Neuropathy: Diabetic Mellitus is the most common cause of leg pain in patients with diabetes and is responsible for 50 – 70% of non-traumatic amputations. Reduced sensation to sensory stimuli including pain, temperature, touch and vibration in the feet and lower parts of the legs in diabetic patients is invariably a result of sensory neuropathy and may go unnoticed by patients for years unless specifically tested for sensory disturbances. The simple definition of Diabetic Peripheral Neuropathy is “the presence of symptoms and / or signs of peripheral nerve dysfunction in people with diabetes after the exclusion of other causes”.21 Neuropathy is present at the diagnosis of type-2 to diabetes mellitus in up to 10% of subjects. 50% of chronic diabetic peripheral neuropathy may be asymptomatic, 10 – 20% experience trouble some symptoms sufficient to warrant specific therapy. The prevalence of diabetes peripheral neuropathy in type-2 diabetes mellitus has been reputed to be 17.5 to 19.1% in Indians. While autonomic neuropathy was prevalent in 35.7% of Indians.22,23 In our study we have seen that the most common complication was Retinopathy i.e. 42% followed by Neuropathy 34%, Nephropathy 14%, Cardiovascular in 18%, Cerebrovascular Accidents 4%. In Insulin treatment group Retinopathy and Cardiovascular complications were more common (54%), followed by OHA was having Neuropathy 38.2%, Insulin+ OHA was having CVS -80% and Retinopathy 60% was more common. The commonest complication among females was retinopathy with an incidence of 52.9%, followed by IHD (41.2%). The commonest complication among the males was peripheral neuropathy (25%) and IHD (25%). There was not much variation seen among the parameters irrespective of duration of diabetes. These findings are similar to Ankush et al 24 they found Out of the 3261 patients 1025 (31.4%) had macrovascular complications and 1122 (34.4%) had at least one microvascular complication. The prevalence of peripheral vascular disease, coronary artery disease and stroke were 6.7%, 21.3% and 6.6% respectively and were significantly higher in males. The prevalence of diabetic retinopathy, nephropathy and neuropathy were 16.7%, 16.5% and 16.3% respectively with diabetic nephropathy being significantly higher in males. Trend analysis showed significant association of rising prevalence of all complications with age (p<0.05). except Duration of diabetes which showed significantly positive trend for all complications (p<0.05) this could be due to different setup and improvement in the treatment methods which prevents the complications.
CONCLUSION It can be concluded from our study that the most common complication was Retinopathy, followed by Neuropathy and Nephropathy. In Insulin treatment group Retinopathy was common followed by OHA group having Neuropathy as a complication, Insulin+ OHA group had more commonly cardiovascular and Retinopathy complications. The commonest complication among females was retinopathy followed by IHD. The commonest complication among males was peripheral neuropathy and IHD.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home