|
Table of Content Volume 10 Issue 3 - June 2019
Inferior mesenteric vein variation in draining pattern: A cadaveric study
Meenakshi P Borkar1, Swapna Chavan2*, Mehera Bhoir3
1,2Assistant Professor, 3Professor and HOD, Department of Anatomy, HBTMC, RNCH, Mumbai, Maharashtra, INDIA.
Email: drmeenakshiukey@gmail.com, drswapnarc@gmail.com
Abstract Background and Objectives: This article examines the variation in the drainage pattern of inferior mesentric vein. During the routine cadaveric dissection of the abdomen at the department of Anatomy of HBTMC and Dr. R.N Cooper hospital, Mumbai, in one of the cadaver it was found that the Inferior Mesentric Vein (IMV) drained into the confluence of splenic and Superior mesenteric vein. Generally, Anatomy resources consistently state that, the Inferior Mesentric Vein anatomically joins and drains into the splenic vein. However, the Inferior Mesentric Vein can also join and drain into the Superior mesenteric vein or the junction between the splenic vein and the Superior mesenteric vein. Material and Method: Study carried out on 30 cadavers during the period of 3 years in the Department of Anatomy of HBTMC and Dr. R.N .Cooper hospital, Mumbai. Conclusion: It has been observed that all the three sites of drainage are not reported in the Anatomy textbooks. Prerequisite information of the drainage pattern of Inferior Mesentric Vein is important for surgeons to choose adequate technique and to avoid injury to inferior mesenteric vein.
Key Word: inferior and superior mesenteric vein, splenic vein, dehiscence.
INTRODUCTION
Anatomy resources consistently state that the inferior mesentric vein anatomically joins and drains into the splenic vein. However, the inferior mesentric vein can also join and drain into the superior mesentric vein or junction between the splenic vein and superior mesentric vein. The inferior mesenteric vein drains blood from the rectum, sigmoid colon, descending colon, and splenic flexure. Together the ascending superior rectal vein, along with sigmoid veins and left colic vein forms the inferior mesentric vein. These veins are accompanied by the arteries of same name. A known data of the drainage pattern of inferior mesentric vein would be helpful to the surgeons to redecide on the adequate technique and to avoid injury during colorectal surgeries, especially at the time of inferior mesentric vein ligation. It is observed that anatomical variations around inferior mesentric vein compromised blood supply to the left colon, congestion, ischemia and different levels of colitis or anatomical dehiscence. Hence some surgical complications like colic congestion and ischemia due to venous drainage compromise can be prevented. The complexity of these procedures places an even higher importance on extensive preoperative knowledge of mesenteric venous anatomy, its relationship to arterial anatomy, and the improved quality of preoperative computed tomography (CT) gives the surgeon a tool to “map out” planned resections and reconstructions1.
MATERIAL AND METHODS
Study carried out on 30 cadavers during the period of 3 years irrespective of age and sex in the Department of Anatomy of HBTMC and Dr. R. N. Cooper hospital, Mumbai. During the routine cadaveric dissection of the abdomen in one of the cadavers it was found that the inferior mesentric vein drains into the confluence of splenic and Superior mesentric vein. Generally, it is known that inferior mesentric vein drains into the splenic vein. Dissection was done meticulously and clean to rule out the variation and photographs were taken with and without coloring the vessels. Figure (1) shows the drainage of inferior mesenteric vein at the confluence of superior mesenteric and splenic veins. Figure (2) is the same figure after highlighting the veins with blue paint, along with splenic artery colored in red. Figure(1) sv=splenic vein, sa=splenic artery, imv=inferior mesentric vein, smv=superior mesentric vein Figure(2)
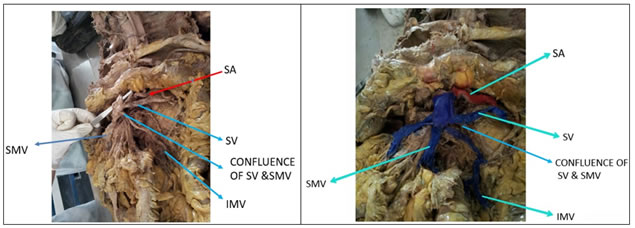
Figure 1 Figure 2
DISSCUSSION
Inferior mesentric vein is a continuation of superior rectal vein, its main tributaries are sigmoid and left colic vein. It lies usually at left anterior pararenal space, anterior to left psoas muscle and behind duodenojejunal junction. IMV is located close to the ligament of Treitz and passes below lower border of pancreas to join the splenic vein. In surgical practice inferior mesentric vein is ligated at the lower border of pancreas for more medial mobilization and tension free anastomosis to prevent vascular ischemia. Surgeons call it “critical zone of IMV”. A study based on 113 cadaveric dissection done by Weinhaus, A.J. et al2 at the University of Minnesota reported that the inferior mesenteric vein drained into the splenic vein in 36.3% of cases, the superior mesenteric vein in 41.6% of cases, and the junction between the superior mesenteric vein and the splenic vein in 21.2% of cases2. It is also observed that variability of the collateral blood supply to the splenic flexure and its relation to make it a part of our concern during colorectal surgical procedure. The drainage pattern of inferior mesentric vein will help the anatomical landmarks need to be recognized during colorectal procedures, especially at the time of inferior mesentric vein ligation. The inferior mesenteric vein (IMV) emerges from small veins that drain the sigmoid colon. It runs medial to the descending colon gathering its draining veins within the mesocolon in the left anterior pararenal space. Here it is usually located lateral to the superior and inferior mesenteric artery and anterior to the left ureter and gonadal veins. It passes behind or lateral to the duodenojejunal junction. Finally it drains either into the splenic vein, the confluence of splenic vein and superior mesenteric vein, or into the superior mesenteric vein (SMV). Krumm et al3 analysed 916 abdominal CT-scans to document anatomic variations of the IMV. These authors found that the IMV typically drains into the splenic vein (approx. 40%), into the portal confluence (approx. 30%), or into the SMV (approx. 20%) these anatomic details were best seen on coronal images. This knowledge is important for gastrointestinal surgery, e.g. transplantation planning, pancreatic cancer surgery, etc. Another interesting point in this study was the small distance to the portal venous system from where the IMV drained either into the splenic vein (1.66cm) or into the SMV (0.75cm), respectively. Such anatomic knowledge is also important for colour duplex sonography; the examiner must take care to visualise the portal confluence and its surroundings including the draining vessels. Otherwise thrombosis, cancerous invasion, etc. might be missed. This kind of studies are helpful for the vascular resection in patients with pancreatic adenocarcinoma, and preoperative knowledge of each patient’s anatomy is crucial in planning for resection and reconstruction. The ability to identify a patient’s mesenteric venous anatomy with preoperative CT scans can also avoid major blood loss by anticipating the course of the veins. Avoiding injury to these branches also prevents injury to the SMA that can occur in an attempt to control venous bleeding with sutures. The surgeons must be aware of mesenteric venous variants to perform peripancreatic surgery.
CONCLUSION
In the present case report it was found that the inferior mesentric vein drains into the confluence of splenic vein and superior mesentric vein, generally it drains into the splenic vein. It has been observed that all the three sites of drainage i.e. at splenic vein, superior mesentric vein and confluence at splenic and superior mesentric veins are not reported in the books. It is imperative that all these common drainage sites of the inferior mesentric vein should be stated in Anatomy resources, so that students can learn realistic Human Anatomy including its common variations. The aim of this case report is to draw attention to the variable drainage pattern of the inferior mesentric vein and kindly see to it that students are taught about these common variations and should be included in the Anatomy textbooks.
REFERENCES
- Papavasiliou P, Arrangoiz R, Zhu F, Chun Y, Edwards K, and Hoffman J. The Anatomic Course of the First Jejunal Branch of the Superior Mesenteric Vein in Relation to the Superior Mesenteric Artery. International Jou Surg Onco.2012; 1-4. [15].
- Variation of the drainage pattern of the Inferior mesentric vein. Weinhaus, A.J.and Henderson (2011) In clinical Anatomy. 24(8), p.1016-1042
- Pylephlebitis of a variant mesenteric vein complicating sigmoid diverticulitis. Falkowski AL, Cathomas G, Zerz A, Rasch H, TarrPE.JRadiol Case Rep. 2014 Feb; 8(2):37-45. Epub 2014 Feb 1
- Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K et al. Analysis of anatomic variants of mesenteric veins by 3-dimensional portography using multidetector-row computed tomography. The American Journal of Surgery.2010; 200(1):15-22. [16].
- Snell, R. The Abdomen: Part II The Abdominal Cavity. In Clinical Anatomy for Medical Students :5th edition. Little, Brown and Company:1995. p. 212. [17].
- Y. S. Chun, B. N. Milestone, J. C. Watson et al., “Defining venous involvement in borderline resectable pancreatic cancer,” Annals of Surgical Oncology, vol. 17, no. 11, pp. 2832–2838, 2010.
- J. B. Stokes, N. J. Nolan, E. B. Stelow et al., “Preoperative capecitabine and concurrent radiation for borderline resectable pancreatic cancer,” Annals of Surgical Oncology, vol. 18, no. 3, pp. 619–627, 2011.
- M. H. G. Katz, P. W. T. Pisters, D. B. Evans et al., “Borderline resectable pancreatic cancer: the importance of this emerging stage of disease,” Journal of the American College of Surgeons, vol. 206, no. 5, pp. 833–846, 2008.
- K. Misuta, H. Shimada, Y. Miura et al., “The role of splenomesenteric vein anastomosis after division of the splenic vein in pancreatoduodenectomy,” Journal of Gastrointestinal Surgery, vol. 9, no. 2, pp. 245–253, 2005
- H. G. K. Matthew, J. B. Fleming, W. T. P. Peter, J. E. Lee, and D. B. Evans, “Anatomy of the superior mesenteric vein with special reference to the surgical management of first-order eranch involvement at pancreaticoduodenectomy,” Annals of Surgery, vol. 248, no. 6, pp. 1098–1102, 2008.
- J. N. Vauthey and E. Dixon, “AHPBA/SSO/SSAT consensus conference on resectable and borderline resectable pancreatic cancer: rationale and overview of the conference,” Annals of Surgical Oncology, vol. 16, no. 7, pp. 1725–1726, 2009.
- Graf O, Boland G. W, Kaufman J. A, Warshaw A. L, Fernandez del Castillo et al. Anatomic variants of mesenteric veins: Depiction with helical CT venography. Amer J Roent. 1997;168(5):1209-13.
- O. Graf, G. W. Boland, J. A. Kaufman, A. L. Warshaw, C. Fernandez Del Castillo, and P. R. Mueller, “Anatomic variants of mesenteric veins: depiction with helical CT venography,” American Journal of Roentgenology, vol. 168, no. 5, pp. 1209–1213, 1997.
- S. Vedantham, D. S. K. Lu, H. A. Reber, and B. Kadell, “Small peripancreatic veins: improved assessment in pancreatic cancer patients using thin-section pancreatic phase helical CT,” American Journal of Roentgenology, vol. 170, no. 2, pp. 377–383, 1998.
- H. J. Kim, Y. T. Ko, J. W. Lim, and D. H. Lee, “Radiologic anatomy of the superior mesenteric vein and branching patterns of the first jejunal trunk: evaluation using multi-detector row CT venography,” Surgical and Radiologic Anatomy, vol. 29, no. 1, pp. 67–75, 2007.
- T. Sakaguchi, S. Suzuki, Y. Morita et al., “Analysis of anatomic variants of mesenteric veins by 3-dimensional portography using multidetector-row computed tomography,” American Journal of Surgery, vol. 200, no. 1, pp. 15–22, 2010.
- K. K. Christians, A. Lal, S. Pappas, E. Quebbeman, and D. B. Evans, “Portal vein resection,” Surgical Clinics of North America, vol. 90, no. 2, pp. 309–322, 2010
- Nayak SB, Aithal AP, Melanie RD, Guru A, Kumar N. Unusual jejunal tributaries of the splenic veinand their surgical importance: a case report. OA Case Reports 2013;2(4):36-40
- Knight HO. An anomalous portal vein with its surgical dangers. Annals of Surgery 1921;74(6):697-702
- Lin YY, Lee RC, Tiu CM, Chiang JH, Chang CY. Absence of Inferior Mesenteric Vein: a case report. J Radio Sci 2014; 39: 17-20.
- Anatomical variation of the Inferior mesentric vein’s drainage pattern. Master of science (Biomedical science), Zilaie Mina, May 2015, 44pp.
- Popovici Z. Angiographic research on the blood supply of the colon with a view to oesophagoplasty (author's transl). Journal de Chirurgie 1976; 113(5-6):517-26.
- The relation between Inferior mesentric vein ligation and collateral vessels to splenic flexure. Anatomical landmarks, Technical precaution and clinical significance. Sami F. Al-Asari, Daero Lim, Byung Soh Min, and Nam Kyu Kim. Yonsei Med J 54(6):1484-1890, 2013
- Krumm P, Schraml C, Bretschneider C, et al. Depiction of variants of the portal confluence venous system using multidetector row CT: analysis of 916 cases. Rofo. 2011;183(12):1123–9.
|
|