|
Table of Content Volume 11 Issue 3 - September 2019
Anatomical study of cystic duct and its clinical correlation
Usha K Dandekar1*, Kundankumar N Dandekar2
{1Associate Professor, Department of Anatomy} {2Professor, Department of Surgery} Rural Medical College, Pravara Institute of Medical Sciences, Deemed to be University, Loni Bk Taluka- Rahata, Dist- Ahmednagar, Maharashtra PIN-413736, INDIA.
Abstract Background: The cystic duct is important landmark in operation of cholecystectomy. In cholecystectomy surgeons need to identify cystic duct so as to clamp or clip it carefully. The anatomical study of cystic duct was undertaken to provide a cadaveric map of cystic duct and its possible variations. Results: The cystic duct was present in all specimens and its length varied from 0.7cm to 8cm with an average length of 2.22 cm. The external diameter of cystic duct varied from 2mm to 5mm with an average diameter of 3.76mm. Duplication of cystic duct was found in one specimen (2%), where one cystic duct joined the common hepatic duct and the accessory cystic duct arose from the right margin of gall bladder, passed downward and posterior to cystic artery and joined the common hepatic duct at its commencement on right side. In 98% of cases, the cystic duct joined the common hepatic duct. Out of them in 72%, it joined the common hepatic duct on right side, in 18% on left side and in 8% on posterior aspect of common hepatic duct. In one specimen the cystic duct, right hepatic duct and left hepatic duct joined at the same level while the common hepatic duct was absent. In one specimen the gall bladder and cystic duct were situated left to the common hepatic duct and the cystic duct crossed the common hepatic duct anteriorly and opened on its right side. In 60% cases, cystic ducts were closely related to arteries like cystic, accessory cystic, superficial and deep branches of double cystic, right hepatic and aberrant right hepatic arteries. Out of them in 34% the arteries were found to be running anterior and in 26% posterior to the cystic duct. In 40% the duct possessed no arterial relations. Conclusion: Sound anatomical orientation of cystic duct and its related structures is important. Anatomical dissection provides a good orientation to the surgeons indulging in cholecystectomy. Key Word: Cystic duct, cholecystectomy. INTRODUCTION The cystic duct (CD) is important organ which denotes important landmark in operation of cholecystectomy. Cholecystectomy is the commonest open or laparoscopic procedure where surgeons need to identify the CD (and cystic artery) so as to clamp or clip it carefully and preserve the structures in its vicinity to avoid injury and complications which may prove disastrous. The gall bladder (GB) is connected to common bile duct (CBD) through CD. In cholecystectomy the CD is clipped just before its union to the common hepatic duct (CHD) to remove the GB. This anatomy of CD is of immense importance to a surgeon indulging in open or laparoscopic cholecystectomy because definite identification of CD is key step. There is always possibility of anomalies in this region which may interfere with identification of CD and may result in morbid and disastrous complications. The GB frequently gets involved in disease processes like cholecystitis, cholelithiasis, and choledocholithiasis. Most of these conditions need operative intervention of cholecystectomy: open or laparoscopic. The open cholecystectomy is now almost replaced by laparoscopic cholecystectomy but in certain cases open cholecystectomy is still required. In fact now a days open cholecystectomy needs more expertise because most of the times difficulty in the laparoscopic surgery calls for conversion to open surgery. These difficulties include adhesions, inflammation and anomalies. All of them leading to problem in identification and exposure of CD. It may not be wrong to say that inadequate knowledge of the course and relationship of CD combined with failure to expect anomalies which are common in this region may lead to most of the major intra and post-operative complications. The CD bridges the GB to the CHD. The average length of CD measures about 2-4 cm and average diameter is of 3-4 mm. It runs parallel to the CHD and becomes adherent by fibrous tissue a short distance before its union to CHD. It passes backwards, downwards and to the left to join the right lateral aspect of the CHD to form the CBD. The mucosa of the CD contains 5-12 crescenticfolds, similar to those seen in the neck of the GB. They project obliquely in regular succession and form spiral valve, called as spiral valves of Heister. When the duct is distended, the spaces between the folds dilate and externally the CD appears twisted. As mentioned in the beginning the CD is important landmark to be identified, clipped or clamped and cut in cholecystectomy. So operative procedure needs a systematic approach to reach the CD. The commonest and popular approach to CD includes primary identification of another important landmark known as hepatocystic triangle or Calot’s triangle which is bounded superolaterally by inferior surface of right lobe of liver, inferolaterally by CD and medially by CHD. It contains cystic artery, right hepatic artery, and occasionally aberrant or accessory bile duct or aberrant right hepatic artery1.In situation where Calot’s triangle is difficult to approach as in adhesions, a “fundus first” approach can be utilizedin which the fundus of GB is identified first and retrograde careful dissection towards union of CD and CHD is pursued.
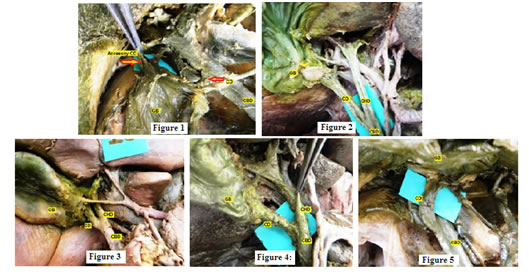
MATERIAL AND METHODS This prospective, observational, cross sectional, cadaveric study was conducted on 50 formalin embalmed adult cadavers with normal subhepatic anatomy, from the department of Anatomy of Rural Medical College, PIMSDU, Loni, Maharashtra. The dissected cadavers represent a heterogeneous sample of local population. Cadavers with scar mark or evidence of operative procedure in subhepatic region or any subhepatic pathology were excluded. The Subhepatic region of the abdomen was exposed by separating the lesser momentum with gross dissection to identify the extrahepatic biliary apparatus and followed by fine dissection to expose the CD. The morphology, any variations of CD and related arteries were carefully observed and noted. The measurements were obtained with the help of Vernier calliper, divider, thread, and scale. Findings of every cadaveric dissection were recorded and extensively photographed for records. Finally all the collected data was analysed and compared with the findings of the various workers. RESULTS The CD was present in all specimens and its length varied from 0.7cm to 8 cm with an average length of 2.22 cm. In 25 specimens (50%), it measured between 2 to 4 cm. In 23 specimens (46%), it was less than 2 cm long and in 2 specimens (4%) the length of the CD was more than 4 cm. Short CD was found in almost 46% of cases where the incidence was quite high as compared to the long CD. By applying Z test of difference between two proportions there is a significant difference between proportions of short CD as compared to long CD (i.e. p<0.05). Duplication of CD was found in one specimen (2%), where one CD joined the CHD and the accessory CD arose from the right margin of GB, passed downward and posterior to cystic artery and joined the CHD at its commencement on right side. (Figure 1) In the present study the mode of union of the CD to CHD was of angular type in 31 cases (62%), [Figure2] parallel type in 10 cases (20%) [Figure 3] and spiral type of union in 9 specimens (18%)[Figure4].The percentage of angular type of union was on higher side. All 10 specimens of parallel type of union were of the short parallel typei. e. the two ducts, CD and CHD, were running parallel to each other for a distance of less than 4 cm. In the spiral type of union, the spiraling of the CD was either on anterior or posterior aspect of the CHD. In 2 cases the CD showed anterior spiraling (Figure 5) and in 7 cases it showed posterior spiraling. (Figure 4) The posterior spiral type was more than anterior spiral type. In the present study the CD joined the CHD in 49 specimens (98%).Out of them in 36 specimens (72%) the CD joined the CHD on right side, in 9 specimens (18%) on left side and in 4 specimens (8%) on posterior aspect of CHD. In one specimen (2%) the CD, right hepatic duct and left hepatic duct joined at the same level where the CHD was absent. An interesting fact was observed in one specimen where GB and CD were situated on left side of CHD and the CD crossed the CHD anteriorly and joined on its right side. (Fig.5) In 47 specimens the CD joined the CHD above first part of the duodenum while in 3 specimens the union occurred behind the first part of duodenum(low union). In 60% cases, cystic ducts were closely related to arteries like cystic, accessory cystic, superficial and deep branches of double cystic, right hepatic and aberrant right hepatic arteries. Out of them in 34% the arteries were found to be running anterior and in 26% posterior to the cystic duct. In 40% the duct possessed no arterial relations. Figure 1: Duplication of cystic duct; Figure 2: Angular union of the cystic duct and common hepatic duct; Figure 3: Parallel union of the cystic duct and common hepatic duct; Figure 4: Spiral union of the cystic duct and common hepatic duct; Figure 5: Cystic duct crossing Common Hepatic Duct from left to right side (Anterior spiraling)
DISCUSSION Maingot described about 55 % of CD were 2 to 4cm long, 20 % were less than 2cm long and 25% were longer than 4cm2. In the present study these ranges were found to be 50%, 46% and 4% respectively. We found the incidence of short CD was quite higher. The short CD needs careful surgical attention because chances of injury to CHD or CBD are increased during clamping or ligation of such short CD3 Confirmation of short CD also poses difficulty during surgery and may lead to inadvertent or accidental ligation of CHD. Though the average length of CD was similar to the findings of Dowdy3 and Johnston4 but the range of length of CD was found comparatively higher than other authors: Maingot, Lindner, Adkins and Sivak2,5,6,7. A longer CD also has surgical importance. During cholecystectomy the CD needs to be removed flush to its junction to CHD Failure to remove the CD completely, may leave behind a remnant or stump that in future may cause formation of stone and recurrence of symptoms8. In the present study long CD was found in two cases where both were posterior spiral. The average external diameter of CD in this study was 3.76mm which corresponds to the findings of Dowdy3. The literature reveals that variations in the CD are quite common but occurrence of double CD is extremely rare. Whenever such double CD is present, 80% are associated with double GB [9].Duplication of CD has been reported by Houston and Senapati9,10. In the present study, duplication of CD was found in one specimen (2%), where one CD was arising from normal position and joined the CHD while accessory CD arose from the right margin of GB, 3cm away from neck of the GB and joined the CHD at its commencement. Therefore the surgeon should keep in mind the possibility of accessory CD before ligating the CD during cholecystectomy. In the present study angular, parallel and spiral types of union of CD and CHD were found in 62%, 20% and 18% of specimens respectively. The findings are almost similar to that of Johnston4. Angular type of union was similar to Beaver11. It was less than the studies of Ruge, Descomps, Eisendrath as mentioned by Johnston4. The parallel type of union is comparable to the findings of Eisendrath and Kune4 while the spiral type of union was less than the findings of Ruge, but it is quite higher as compared to the studies of Beaver11. Hayes12 reported 0.75% anterior spiral and 0.75% posterior spiral union of CD and CHD. In the present study spiraling of the CD was seen in 18% where, in 4% it was anterior spiral and in 14 % it was posterior spiral type.Maingot2 described that the CD normally opens on the right side of the CBD, but in 8 to 10 percent of cases it enters on the anterior surface, on the posterior surface or even on the medial side twisting spirally around the main duct. In 15% of cases it enters the left side of the CBD. Flint13 observed this opening on right side in 94%, on anterior aspect in 4%, on posterior aspect in 1% and on left side in 0.5%. In the present study almost 72% of cases the CD opened on right side of the CBD, in 18% on left side and in 8% on posterior aspect of CBD. This incidence of termination of CD is not comparable to the findings of Flint13.In the present study, in 94% of cases the CD joined CHD above the level of first part of duodenum. Whatever the union of CD with CHD, the length of CD was found to be 2.8cm to 4.5cm. This suggests that the length of the CD does not depend on the low union or high union of the CD with the CHD. Surgical significance of various sites of union of the CD: When the CD drains into the right hepatic duct it may prove a source of confusion and danger during cholecystectomy. In this condition the right hepatic duct may consequently be tied off and divided where it joined the left hepatic duct. The resultant stricture is quite refractory to surgical treatment2. When the CD joins at the junction of right and left hepatic ducts or all three join together at the same level, either the right hepatic duct or the left hepatic duct may be injured at the time of ligation of the CD. Also traction on the GB produces a kinking of the hepatic ducts and either of them may be caught in ligature placed around the CD. When the parallel type of union of the CD and CHD exists, the two ducts may be closely adherent to each other, so that it is very difficult to put a clamp upon the CD or to isolate it without injuring the CHD1. In spiral and parallel unions a variable length of the CD is found joining CHD at the lower level and the two are enveloped in a common connective tissue sheath (producing a "double barrelled CBD"). Failure to recognize these during operation may result in injuries to the duct system. In case of low union of the CD with the CHD, during a cholecystectomy, lower the union, the greater are the chances of leaving behind a long CD stump8,14. Johnston et al4 found 25.7% of cystic ducts having anterior arterial relations and 22.8% having posterior arterial relations. In the present study anterior arterial relations of CD was found in 34% and posterior arterial relations in 26% of cases. Amongst the arteries, Johnston et al4 found cystic artery anterior and right hepatic or accessory right hepatic artery posterior to the CD. We found the same arterial relations as Johnston. Therefore one should know the possibility of aberrant cystic, right hepatic or aberrant right hepatic arteries being situated posterior to the CD.
CONCLUSION The clipping or clamping of CD is important event in open or laparoscopic cholecystectomy respectively. It is important to have sound anatomical orientation of CD and structures related to it. Anatomical cadaveric dissection provides a good orientation and knowledge of anatomy of CD to the surgeons indulging in open or laparoscopic cholecystectomy.
REFERENCES
|
|
 Home
Home