|
Table of Content Volume 11 Issue 3 - September 2019
Review of the brachial canal and its content among the African people living in Benin: About 20 cases
Pilabre Wh*, Agossou Ac, Agossou-Voyeme Ak, Hounnou Gm
Laboratory of Human Anatomy and Organogenesis, Faculty of Health Sciences, Cotonou, BENIN. Email: pilabreherve@yahoo.fr
Abstract Background: The brachial canal is commonly addressed in surgery, clinical practice, or to achieve a nerve block anesthesia. The aim of this work was to study by corpse dissection, the anatomy of the brachial canal to meet the anatomical variations. Material and Method: It had been a cadaveric study, descriptive of brachial canal and its content including the brachial artery and veins, the median nerve, the musculocutaneous nerve and the medial cutaneous nerve of the forearm. We dissected twenty (20) brachial canals in ten (10) corpses during a three-month period from June to August 2014. All the corpses were adults well preserved in a formalin bath without concept of trauma or distortion or malformation of the upper limb. Results: The size of the corpses averaged 168,7cm. The average length of the arms was 30,6cm. The main changes are as follows: one (01) case of the brachial artery bifurcation in the arm at 20, 7 cm from the elbow giving high origin of the radial and ulnar arteries; two (02) cases of anastomosis between the median and the musculocutaneous nerves, the average length of these anastomotic branches was 5.7cm; in one (01) last case, it was found an unusual branch of the ulnar nerve, which had replaced the defective dorsal branch of the medial cutaneous nerve of the forearm itself remained undivided. For the rest, the anatomy of the brachial canal observed in our study was consistent with literature. Discussion: Among the changes observed in this study, anastomosis between median and musculocutaneous nerves are quite common; high brachial artery bifurcation is described although infrequent; about the abnormality of the medial cutaneous nerve of the forearm and the ulnar nerve, it has not been described to our knowledge. Conclusion: The variations and anomalies noted deserve to be known by practitioners in the diagnostic investigations and therapeutic interventions on the arm Key Word: brachial canal, dissection, brachial artery bifurcation, nerves variations.
INTRODUCTION The brachial duct contains the vasculonervous bundle of the arm, namely the brachial artery, the two brachial veins along the brachial artery, which receive the basilic vein in the middle third of the arm, medial, ulnar and cutaneous median nerves of the arm and the forearm. The knowledge of the surface anatomy, the segmental arrangement and the disposition of the elements of the brachial canal content is necessary for the physician, particularly when interpreting angiography, taking nerve grafts, making multi- truncus of the brachial plexus or surgical operations on the arm. The anatomy of the brachial duct and its contents is described in the literature. The inter and intra-individual variations of the contents are in the order of 30% to 38%.1,2 To our knowledge, there are very few studies of the anatomy of the brachial duct and its contents in the African environment, especially Benin. The aim of this work was to study the brachial duct and its contents in the Beninese subject from the dissections of corpses.
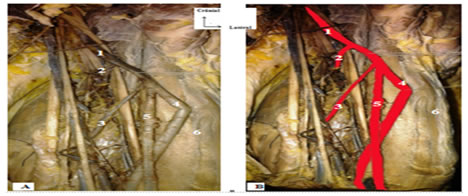
MATERIAL AND METHODS OF STUDY It was a cadaveric, descriptive and analytical study of the contents of the brachial canal. We had dissected twenty arms of ten corpses at the Anatomy Laboratory of the Faculty of Health Sciences in Cotonou over a period of three months. All cadavers were adults without trauma or deformity or malformation of the thoracic limb. The well-preserved bodies were included in the study in a formalin bath. Photographs of the dissection pieces were made using a Samsung-branded color camera with a 4.0x super zoom with built-in flash. The photos had been stained with the Photoshop 7 software. The cadavers were placed in supine position, the thoracic limb abducted between 70° and 90° and supinated to reveal the medial aspect of the arm. The dissection technique consisted of: - a vertical cutaneous incision, involving only the skin from the lateral end of the clavicle to 3 cm above the middle of the crease of the elbow, -Two horizontal incisions perpendicular up and down at the ends of the vertical and extending from one edge to the other of the arm; the dissected cutaneous flaps were folded down on each side, The subcutaneous cellular tissue was incised, dissected and folded in the same manner as the skin, - After vertical incision of the brachial fascia, we removed its deep face to the medial and lateral intermuscular septums of the arm before dissecting the soft parts which include the muscles, vessels and nerves. Then we removed the two fragments of the brachial fascia while preserving the medial cutaneous nerve of the forearm and the basilic vein which cross it before the photograph. RESULTS Brachial artery: In 19 cases, the brachial artery descends as usual in the anterior and medial region of the arm along a rectilinear path. It passes through the medial bicipital furrow, bends laterally to the ventral region of the elbow. In 01 cases, we found a bifurcation of the brachial artery in the left thoracic limb. The bifurcation was located 20.7 cm from the elbow crease immediately after the deep brachial artery and the upper ulnar collateral artery (Figure 1).
Figure 1: Ventral view of the arm showing the bifurcation of the brachial artery (1. Brachial artery 2. Deep brachial artery 3. Upper ulnar collateral artery 4. Main brachial artery 5. Accessory brachial artery 6. Biceps brachial muscle) Ulnar nerve and medial cutaneous nerve of the forearm (MCF): By dissecting the ulnar nerve, we found that it is located at the medial border of the brachial artery at its origin. It then moves away, pierces the medial intermuscular septum, leaves the brachial canal and walks between this partition and the medial head of the triceps brachial.
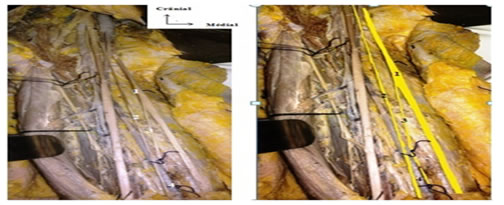
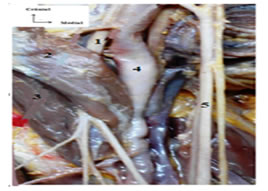
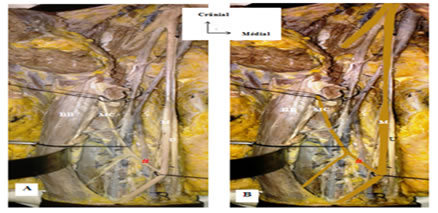
Figure 2: Ventral view of the arm showing the absence of bifurcation of the medial cutaneous nerve of the forearm compensated by the existence of an unusual branch of the ulnar nerve (1. Ulnar nerve 2. Medical nerve of the forearm and ventral branch of medical nerve of the forearm 3. Dorsal branch of medical nerve of the forearm 4. Basilic vein) Musculocutaneous nerve and median nerve: The musculocutaneous nerve (MC) perforated the coraco-brachial muscle by insinuating itself between its dorso-lateral and ventro-medial bundles; Then he passed between the brachialis biceps muscle forward and the brachial muscle back. After giving branches to the coraco-brachial muscles, biceps and brachial muscles, he traveled in the lateral bicipital groove between the biceps brachial and brachio-radial muscles. (1. Musculocutaneous Nerve 2. ventro-medical bundle of the coraco brachial muscle 3. laterl dorso bundle of the coraco brachial muscle 4. Brachial artery 5. Medical nerve) The median nerve conformed to the classical description. He was born on the lateral edge of the brachial artery and crossthis artery in X to find himself on its medial edge. In 02 cases, he had presented a fickle anastomotic branch which unites it to MC nerve. Each time it was a distal communication with respect to the point of penetration of MC nerve in the coraco-brachial muscle. Figure 4: Ventral view of the arm showing the anastomosis between the median and musculocutaneous nerves (U: ulnar nerve M: Medical nerve MC: Musculo-cutaneous nerve BB: Biceps brachii #: Anastomotic branch) DISCUSSION High bifurcation of the brachial artery: We observed one (01) high bifurcation case of the brachial artery on 20. Celik in an angiographic study on 81 arms found it in 7 cases or 8.6% of the cases4. Kian on his side had found 12.3% of cases out of 481 arms.5 The difference is not significant given the numerical weakness of our sample. The lateral branch of this high bifurcation was named accessory brachial artery by Adachi6. It corresponds to a high origin of the radial and ulnar arteries according to Keen, Jurjus, Kodama and Aughteen7;8;9;10. In our case, the high bifurcation of the brachial artery to be differentiated from a double brachial artery was observed in the left thoracic limb as Coskun and Krstonosic11;12. Aughsteen10 described this variation in the two thoracic limbs. In our study this bifurcation occurred after the birth of the deep brachial artery as in Cherukupalli13. The existence of such variation is clinically important. It may cause complications during intravenous drug delivery or percutaneous brachial venous catheterization. Doppler ultrasound makes the diagnosis of in vivo certainty of this anatomical variation. His knowledge is thus useful, not only for anatomists, but also for radiologists, orthopedic surgeons, vascular surgeons or plastic surgeons. Anastomosis between median nerve and musculocutaneous nerve: The anastomosis between the median nerve and the musculocutaneous nerve is the most frequent variation of the brachial plexus below the clavicle. In our study, it is of type IV in the 1st case and of type III in the second case according to the classification of Le Minor14. The classification of Venieratos and Anagnostopoulou15 makes it possible to compare the results of our series with those of other authors (table). Table: type of communication between median nerve and MC nerve in the various studies according to the Venieratos classification
This table shows that types I and II are the most often encountered and that the predominance of one in relation to the other is variable according to the authors. Our two cases are distal or II but do not support the comparison given the numerical weakness of our sample. The average length of the anastomosis was 5.7 cm versus 1.77 cm in Eglseder19 but the comparison is not possible either. The embryogenesis of the musculature of limbs and peripheral nerves play an important role in the etiology of these anatomical variations.19 Ulnar nerve and medial cutaneous nerve of the forearm: We observed a case of absence of division of the medial cutaneous nerve of the forearm (MCF) in the ventral and dorsal branch as usual. This nerve trunk continued the usual direction and path of its ventral branch while an unusual upper branch of the ulnar nerve substituted for the deficient dorsal branch of the MCF nerve. This observation has not been described in the literature to the best of our knowledge. It could explain some cases of partial failure of the brachial plexus block to the brachial duct and be important during surgical procedures.
CONCLUSION
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||
 Home
Home