|
Table of Content Volume 11 Issue 3 - September 2019
A morphometric study of dry human sacra
Sarika H Dakare1*, Pritha S Bhuiyan2
1Registrar, Department of Anatomy, HBT Medical College, Juhu, Mumbai, Maharashtra, INDIA. 2Professor & HOD, Department of Anatomy, Seth G.S. Medical College, Parel, Mumbai, Maharashtra, INDIA. Email: sarika.dakare@gmail.com
Abstract Background: Sacral hiatus is the most important landmark for caudal epidural anaesthesia in obstetrics as well as orthopedic practice for diagnosis and treatment. Aim: The aim of this study was to observe morphometric characteristics of sacral hiatus. Material and Method: This study was conducted on 109 dry human sacra, obtained from the bone library, Department of Anatomy of a tertiary care teaching institutes. Result: The most common shape sacral hiatus in the present study was inverted U (51.38 %). Second most common shape of sacral hiatus found was inverted V (29.36%). Absent sacral hiatus was seen 1.83% while complete spina bifida and incomplete spina bifida was seen in 1.83% and 2.75% respectively. Apex of sacral hiatus was observed most commonly at S4 with 66.97%. Level of base of sacral hiatus found most commonly at S5 level in 94.50 %. Conclusion: Different variations of shape and level of sacral hiatus found in this study will help anesthetists during caudal epidural anaesthesia. In the present study, the method used to detect sacral hiatus using a triangle formed by bony landmarks will help clinicians for giving a safe epidural anaesthesia using newer approaches. Key Word: sacra, hiatus, triangle.
INTRODUCTION The sacrum is a large, triangular fusion of five vertebrae and forms the posterosuperior wall of the pelvic cavity, wedged between the two hip (innominate) bones. Sacral hiatus is produced by the failure of the laminae of the fifth sacral vertebra to meet in the median plane and as a result the posterior surface of the body of that vertebra is exposed on the dorsal surface of the sacrum1. Caudal epidural anaesthesia is most commonly used in obstetrics. It has been also widely used for the treatment of lumbar spinal disorders and for the management of chronic back pain. A needle is introduced through the inferior hiatus and anaesthetic solution is injected to block second, third, fourth sacral nerves and coccygeal nerves during caudal epidural anaesthesia. The sacral nerves contain sensory fibres from the derivatives of the cloaca (bladder, vagina and rectum).2 Thus, sacral hiatus is the most important landmark for caudal epidural anaesthesia in obstetrics as well as orthopaedic practice for diagnosis and treatment3. So, it is important to know anatomy of sacral hiatus to avoid caudal epidural block failure.
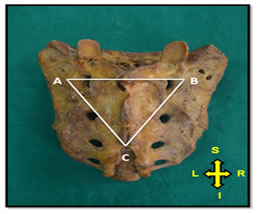
MATERIAL AND METHOD This study was conducted on 109 dry human sacra, obtained from Department of Anatomy of a tertiary care teaching institute. The sacra were of undetermined age and gender. The measurements were taken by using divider, ruler and thread. Length of sacral hiatus: It was distance (mm) from apex to midpoint of base (i.e. midpoint of line joining inner aspects of inferior limits of sacral cornua) of sacral hiatus. Width of base of sacral hiatus: It was distance (mm) between inner aspects of inferior limits of sacral cornua. Linear distance from apex of sacral hiatus to lower end of S2 foramina: It was perpendicular distance (mm) between the apex of sacral hiatus and midpoint of the line joining medial margins of 2nd dorsal sacral foramina. Linear distances between apex of sacral hiatus to left superolateral sacral crest and right superolateral sacral crest: These were distances (mm) between the apex of sacral hiatus and the highest point of left superolateral crest and between apex of sacral hiatus and the highest point of right superolateral crest at the level of upper margin of first sacral foramina respectively. Linear distance between right and left superolateral sacral crests: It was distance (mm) between the right and left uppermost points of superolateral crest at level of upper margins of first sacral foramina. Shape of sacral hiatus: The different shapes of sacral hiatus like inverted U, inverted V etc. were observed. Level of apex and base of sacral hiatus: The vertebral level corresponding with apex and base of sacral hiatus was observed. Descriptive statistical methods like mean, standard deviation and percentage were used for depicting and analyzing data. Microsoft Word and Excel were used to generate graphs and tables. Figure 1: Illustration showing triangle to detect sacral hiatus AB: Distance between left and right superolateral crest of sacrum; AC: Distance between apex of sacral hiatus and left superolateral crest; BC: Distance between apex of sacral hiatus and right superolateral crest. RESULT Various parameters related to sacral hiatus were measured in hundred and nine dry human sacra of undetermined age and gender. Also anatomical variations of sacral hiatus were observed in the present study. All these measurements and observations were mentioned below. Table 1: Different parameters of sacral hiatus
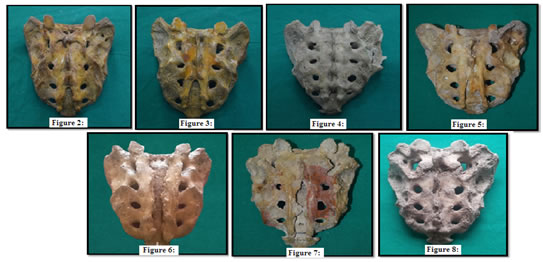
Figure 2: Illustration showing Inverted U shape of sacral hiatus; Figure 3:Illustration showing Inverted V shape of sacral hiatus; Figure 4: Illustration showing Dumbbell shape of sacral hiatus; Figure 5:Illustration showing Irregular shape of sacral hiatus; Figure 6:Illustration showing Complete spina bifida; Figure 7:Illustration showing Incomplete spina bifida; Figure 8:Illustration showing Absence of sacral hiatus
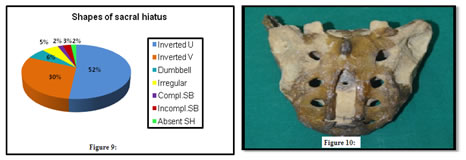
Following pie diagram (Figure 9) showed the comparison of percentage of variations of shape. Figure 9: Comparison of percentage of different shapes of sacral hiatus; Figure 10: Illustration showing sacral hiatus with apex above the level of S2 foramina The most common shape of sacral hiatus in the present study was inverted U which found in 56 sacra out of 109 (51.38 %). Second most common shape of sacral hiatus found was inverted V in 32 sacra out of 109 (29.36%). Absent sacral hiatus was seen in 2 sacra out of 109 (1.83%) while complete spina bifida and incomplete spina bifida were seen in 2 and 3 sacra out of 109 respectively. Level of apex of sacral hiatus varied from S2 to S5 in the present study. Apex of sacral hiatus was seen most commonly at S4 with 66.97%. Level of base of sacral hiatus found at S4 or S5 level. Out of which, most commonly seen was at S5 level in 94.50 %.
DISCUSSION Accurate localization of sacral hiatus is a challenge for clinicians during caudal epidural anaesthesia due to variations in this region. Entry into sacral canal should be safe to avoid dural puncture and to protect surrounding structures. In present study, we observed anatomical variations of sacral hiatus and used newer methods for localization of sacral hiatus using bony landmarks. It is important to know that lesser distance between apex of sacral hiatus and dural sac will be increases chances of dural injury4.Mean length of sacral hiatus in the present study was in accordance with most of the previous studies by Nagar S K5, Patel Z K et al6 and Shewale S N et al7. Width of sacral hiatus is the distance between inferior limits of sacral cornua which is important landmark for caudal epidural anaesthesia. This distance should be sufficient enough for needle insertion. The mean width of base of sacral hiatus in present study corresponds with that in studies by Mustafa M S et al3, Ramamurthi K S et al8 and Phalgunan V et al9. It was higher in present study than that in most other previous studies. The distance between apex of sacral hiatus and level of second sacral vertebra indicates the length of needle that can be safely introduced into the canal. Mean of distance between apex of sacral hiatus and level of second sacral foramina almost resembled with the previous studies like Patil D S et al10, Pal D R et al11 and PhalgunanV et al9; except in study by Mustafa M S et al3. In the present study, measurements of triangle formed between apex of sacral hiatus and uppermost points of left and right superolateral crests was used to locate sacral hiatus. The uppermost points of superolateral crests coincide with posterior superior iliac spines which seen as dimples over skin of lower back. The mean linear distances between apex of sacral hiatus and left and right superolateral crests were almost same as in previous Indian studies while it was higher in study done by Mustafa M S et al3 in Egypt. In inverted U and inverted V shapes, there is sufficient space available for needle insertion in caudal epidural block but it is difficult in irregular and dumbbell shape3. Caudal epidural block cannot be given in absent sacral hiatus12. While caudal analgesia can be given in complete spina bifida as the dorsal wall of the canal is closed by sacrococcygeal ligaments but it may be partially successful as anaesthetic drug infiltrate in surrounding tissues and not block the nerves13. Inverted U was the most common shape of sacral hiatus followed by inverted V in the present study which was comparable with the previous studies. Percentage of dumbbell shape was more common than irregular shape in the present study while this is vice a versa in previous studies. Percentage of complete spina bifida almost resembled with that of previous studies. Incomplete spina bifida and absence of sacral hiatus percentage was higher in present study than previous studies. In present study, apex of sacral hiatus found most commonly at the level of fourth sacral vertebra which coincided with most of the previous studies as well as with standard textbooks. In present study, longer sacral hiatus found in twenty six bone specimens in which apex was at higher level. Out of which; apex is at third sacral vertebra in twenty five specimens and it was significantly higher level at second sacral vertebra in one specimen. More care should be needed in such cases while inserting needle in sacral canal. Reliability and success of caudal epidural anaesthesia depends upon accurate localization of sacral hiatus (SH) but there are considerable anatomical variations in this area, resulting in discrepancies in the size and shape of hiatus which may make its identification difficult. The present study was focused on anatomical variations of sacral hiatus and identification of bony landmarks for localization of sacral hiatus to make caudal epidural anaesthesia successful.
CONCLUSION Different variations of shape and level of sacral hiatus found in this study will help anesthetists during caudal epidural anaesthesia. The method used to detect sacral hiatus using a triangle formed by bony landmarks will help clinicians for giving a safe epidural anaesthesia.
REFERENCES
|
|
 Home
Home