|
Table of Content Volume 12 Issue 1 - October 2019
Myocardial bridges: Cadaveric study
M P Wakchaure
Assistant Professor, Department of Anatomy, Topiwala National Medical College, A.L.Nair road, Mumbai Central, Maharashtra, INDIA. Email: drsonu0281@gmail.com
Abstract Coronary arteries are characterized by subepicardial localization. The intramyocardial segment of epicardial coronary artery is termed as myocardial bridge (MB). MB has been considered as a benign condition which remains silent in majority of cases, MB has been associated with complications like angina, arrhythmia, transient ventricular dysfunction, decreased left ventricular function. New imaging techniques have led to improved identification and functional quantification of myocardial bridging in vivo and hence for commencing appropriate therapy. Present study was carried out in 100 formalin fixed adult cadaveric hearts irrespective of gender. The overall incidence of myocardial bridges was found to be 54% with left anterior descending artery showing highest prevalence. An attempt to find correlation between dominance of coronary circulation with myocardial bridges was done. Key Words: angina, coronary artery, dominance, left anterior descending artery, myocardial bridge
INTRODUCTION The main arteries and major branches of coronaries are usually subepicardial, but those in the atrioventricular and interventricular grooves are often deeply sited, and occasionally hidden by overlapping myocardium or embedded in it1. The coronary artery may dip into the myocardium for varying lengths and then reappear on heart’s surface. This segment of coronary artery present below the thickness of myocardium is known as tunneled artery and the myocardium overlying it is known as myocardial bridge. MB was first recognized more than 200 years ago. It was first described by Reyman in 17372. The first postmortem observation was reported by Geiringer3 in 1951 and was followed by the first radiological description by Portman and Iwig4 in 1960. In 1951 Geiringer referred to over bridged arteries as mural coronaries and suggested that in their intramyocardial segments these vessels are protected from obstructive atherosclerosis. The frequency of myocardial bridging reported in autopsy, cadaveric and radiologic studies has varied considerably (from 0.5 to 86%) 5, 6, 7, 8, 9, 10.It has been considered as a normal variant or a benign coronary anomaly 11, 12. However, reduced coronary flow reserve and an altered vasoreactivity have been documented in arteries with an intramuscular segment.12,13,14 Moreover, myocardial bridging may present a technical challenge during coronary arterial bypass surgery because surgical exposure of intramuscular coronary artery may be difficult, may result in accidental opening of chambers of heart12. Conversely it has been proposed that the intramyocardial parts of arteries may be protected from atherosclerosis when compared with vessels of the same heart that do not form bridges. However, the proximal segment of bridged vessel is more susceptible to development of atherosclerotic lesions because of local hemodynamic disturbances 15. Traditionally considered as benign condition, MB has been associated with non Q wave and even Q wave myocardial infarctions, myocardial stunning or hibernation, ischemia, coronary spasm, acute coronary syndrome, exercise induced A-V conduction block, ventricular septal rupture, early death after cardiac transplantation and sudden death, due to coronary blood flow reduction to peripheral myocardium 16,17,18. A high prevalence has also been reported in heart transplant patients and in patients with hypertrophic obstructive cardiomyopathy (HOCM)19. With each systole the coronary artery is compressed. The degree of coronary obstruction by myocardial bridge depends on factors such as its location, length and thickness of muscle bridge and degree of contractility.
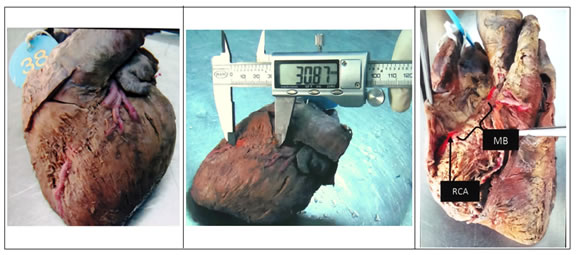
MATERIALS AND METHOD Inclusion criteria- hearts without evidence of gross external pathologies Exclusion criteria- hearts with evidence of gross external pathologies like cardiomyopathy, pericarditis and malignancies. Aim -To study the incidence of myocardial bridges over major branches of right and left coronary arteries. Objective- 1. To measure the length of myocardial bridges 2. To find the correlation between cardiac dominance and myocardial bridges Materials- Dissection instruments- Scalpel, small scissors (one each of straight and curved), toothed and plain forceps, Vernier caliper, Black silk suture material, Ruler, Acrylic colours and painting brush. Methods A total of 100 cadaveric human hearts irrespective of sex were studied. All the parameters were studied by dissection method. The hearts procured from dissection hall were thoroughly washed under running tap water to remove clots. The entire course of Right and Left coronary arteries was traced by cleaning the epicardium and fat in piecemeal. The sites where branches were overlapped by the myocardium were preserved. The right coronary artery (RCA) was dissected from its origin to the posterior interventricular groove and some area beyond this region along the atrioventricular groove. The RCA was divided into 1st segment from its origin to right border of heart, and 2nd segment from right border to commencement of posterior interventricular artery (PIVA). PIVA was traced into the groove of same name till it became too small to dissect. Similarly the Left coronary artery (LCA) was dissected from its origin. The numbers of terminal branches originating from the main trunk of LCA were determined. The anterior interventricular artery (AIV) extending from its origin to apex of heart and beyond it was dissected. The circumflex artery (Cx) from its origin to the posterior interventricular grove was traced. When the length of MB was small it was measured directly with Vernier caliper but when the MB was long enough along the curved heart surface its length was measured with a silk segment and then with Vernier caliper for accurate measurements. Depending on the PIVA the coronary dominance was determined. RESULTS Figure 1: MB located on middle 1/3rd of AIV artery Figure 2: Method of measuring length of MB Figure 3: MB on 1st segment of RCA
Table 1: Overall incidence of MB
Table 2: Distribution of MBs on LCA and RCA
Various branches of LCA appeared to be more affected by MBs than RCA (Table no. 2).
Table 3: Distribution of MBs on individual branches of LCA
(AIV- anterior interventricular artery, diag-diagonal, Cx- Circumflex) Since the AIV branch seemed more prone to have myocardial bridges it was studied in detail by dividing it into three approximately equal segments as proximal, middle and distal. Though any part of AIV can be under MB, almost 25% of the MBs were located in middle segment of it. 16% specimens revealed MBs in its proximal segment and 6% revealed it in distal segment of AIV (TableNo.4). Table 4: Distribution of study group as per location of MBs on segments AIV artery
Table 5: Distribution of MBs on individual branches of RCA
The 1st segment of RCA appeared to be affected by MBs more and the 2nd segment was not affected at all. The dominance of the coronary circulation was determined by PIVA given by RCA or LCA. An effort was made to correlate between dominance and presence of MBs. This correlation was checked for each branch of LCA and RCA. But there was no significant co-relation found between the dominance and MBs.
Table 6: Dominance pattern of Heart
It was seen that 84% of specimens were showing right and 16% were showing left dominance pattern. No co dominance or balanced circulation pattern was observed.
Table 7: Association among study groups between Dominance and MBs on RCA
There is no significant association of MBs over right circulation and left dominance. However, the MBs in right circulation are exclusively present with the right dominant circulation. Table 8: Association among study groups between Dominance and MBs on LCA
The above table shows that there is no significant association of MBs over left circulation and left dominance, however, the MBs in left circulation are common with right dominant circulation. Since AIV is most common branch to be involved in myocardial bridging, and to have various clinical manifestations due to MBs, than any other branch of both the coronaries, the association if any, between the dominance of heart and myocardial bridging on AIV branch was assessed.
Table 9: Association among study group, between dominance and location of MB on AIV according to its segments
(Prox-proximal, mid-middle, dist-distal) The incidence of MBs over AIV was more in right dominance. Table 10: Incidence of MBs by dissection method
The overall highest incidence of myocardial bridging was noted as 58 % by Reig J et al20 in 1993. The present study found the overall incidence as 54%. The highest incidence of MBs, 25%, in present study was found in middle 1/3rd segment of AIV branch which is consistent with findings of Bharambe VK et al25 in 2008. The highest 6% incidence of MBs over 1st segment of RCA is noted in the present study. Regarding MBs on AIV artery the findings are co-incident with the previous authors. In present study the maximum length of MB in AIV artery was in middle third segment being 65.1mm. The maximum lengths in diagonal, circumflex branches of LCA were 67.88 and 37.68mm and in 1st segment and PIVA of RCA were 45.46mm and 15.1mm respectively. Coronary atherosclerosis in association with MBs has primarily been studied in the AIV. The segment proximal to the bridge frequently shows atherosclerotic plaque formation, although the tunneled segment is typically spared 27, 28. In contrast to proximal and distal segments, foam cells and modified smooth muscle cells were missing in patients’ tunneled segments 29. Hemodynamic forces may explain atherosclerotic plaque formation at the entrance of tunneled segment. There the endothelium is flat, polygonal, polymorph indicating low shear, whereas in tunneled segment, the endothelium has a helical, spindle-shaped orientation along the course of the segment as a sign of laminar flow and high shear.29,30,31 The low shear force may induce release of endothelial vasoactive agents contributing to atherosclerotic plaque formation while a high shear may have a protective role in tunneled segment32. With the use of simultaneous proximal and distal pressure recordings, Ge et al10 identified the highest intravascular pressure just proximal to the bridge and a pressure gradient across the bridge. The likelihood of ischemia also increases with the intramyocardial depth of the tunneled segment. An increase in sympathetic drive during stress or exercise likely facilitates ischemia, because tachycardia leads to an increase of systolic-diastolic time ratio at the expense of diastolic flow. Increased contractility during stress further aggravates systolic compression 7. Incidence of MBs over branches of RCA in right dominant circulations in present study was 9.5% and of LCA in left dominant circulations was 50%. In both these cases, obstruction of the dominant coronary artery due to MBs would result in widespread effects due to larger percentage of myocardium being supplied by the dominant artery. In case of obstruction of LCA due to myocardial bridging, the wider distribution of RCA in right dominant hearts may result in lesser part of myocardium suffering from an infarct. Similarly, in case of obstruction of RCA due to myocardial bridging, the wider distribution of LCA in left dominant hearts may result in lesser part of myocardium suffering from an infarct. The present study shows that the maximum incidence of MBs in branches of LCA was seen in right dominant circulation which was 51.1%, but the incidence of the same in left dominant circulation was 50% indicating no significant difference. The maximum incidence of MBs in branches of RCA was seen in right dominant circulation only.
CONCLUSION 1. Incidence of Myocardial bridges is significant (54%). 2. The AIV artery is the most commonly involved branch in myocardial bridging. 3. Myocardial bridges can affect the branches of right coronary artery too. 4. The dominance of the heart has no significant correlation with occurrence of MBs.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home