|
Table of Content Volume 4 Issue 2 -November 2017
A study on variations of intercostobrachial nerve
Kailash Damodhar Balkund1, S Priyadharshini2*
1Associate Professor, 2Assistant Professor, Department of Anatomy, Al azhar medical college and superspeciality hospital, Ezhalloor, Thodupuzha, Kerala, INDIA.
Abstract Background and aims: The lateral cutaneous branch of second intercostal nerve which remains undivided is known as intercostobrachial nerve. This nerve is known to exhibit numerous variations. The aim of this study is to record these variations of intercostobrachial nerve. Aims and objectives: 1. To study the anatomical variations of intercostobrachial nerve. 2. To know the dominant type of variation. Material and methods: This study was carried out on 30 adult human cadavers (60 axillae) available in the department of anatomy at Al azhar medical college. Results: Among 60 axillae, 30 axillae (50%) was type 1, 20 axillae (33.3%) was type 2, 8 axillae (16.6%) was type 3, 2axillae (3.3%) was type 4. Type 5 and Type 6 variants were not found. Conclusion: The knowledge of these variations is important for the surgeons in surgeries of breast carcinoma to reduce the post mastectomy pain Key words: intercostobrachial nerve, post mastectomy pain, breast carcinoma.
INTRODUCTION The lateral cutaneous branch of second intercostal nerve which remains undivided is intercostobrachial nerve (ICBN) which crosses axilla to innervate upper medial portion of arm, axilla and part of anterior chest wall.1-3 It pierces the intercostal muscles and the serratus anterior muscle in the midaxillary line, crosses the axilla to the medial side of the arm and joins with a twig. From the medial cutaneous nerve of arm. While crossing the axilla the nerve gives off the posterior axillary branch which supplies the posterior axillary fold. Thereafter the ICBN pierces the deep fascia and supplies the skin of the upper half of the medial and posterior part of the arm.4 Axillary dissection during breast carcinoma surgeries poses risks to intercostobrachial nerve from stretching as well as from frank transaction. So it is important to study the anatomical variations in intercostobrachial nerve.5 Enlargement of axillary group of lymphnodes, which occurs in breast carcinoma may compress intercostobrachial nerve and cause pain in the area of nerve distribution.6 So it is important to have sound knowledge of intercostobrachial nerve. The alar thoracic artery (ATA) is a variable branch from the second part of the axillary artery supplying the fat and lymph nodes of the axilla. Surgical procedures on the axillary region and pectoral region can be complicated by the presence of an ATA.7 This nerve exhibits numerous variations. The aim of this study is to record these variations in the adult human cadavers.
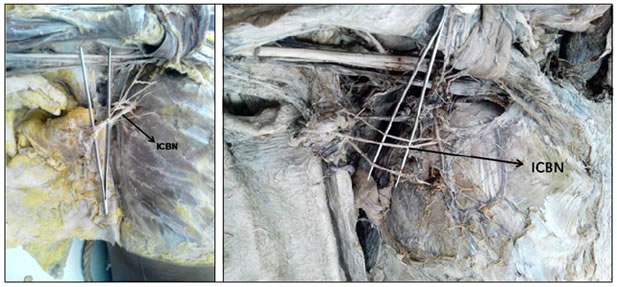
MATERIALS AND METHODS The Axillary dissection was done in 30 well embalmed human cadavers during routine undergraduate dissection. The adult cadavers of both genders were included. Methodology Dissection procedure was carried out as per Cunningham manual of practical anatomy. After removing the loose connective tissue, fat and lymphnode from axilla contents were exposed.8 The course of intercostobrachial nerve was traced and its variations were recorded
RESULTS Axillary dissection was carried out in 30 cadavers. Totally 60 axillae were dissected. Among 60 axillae, 30 axillae (50%) was type 1, 20 axillae (33.3%) was type 2, 8 axillae (16.6%) was type 3, 2axillae (3.3%) was type 4. Type 5 and Type 6 variants were not found. Table 1: Dominant type of intercostobrachial nerve in human cadavers
DISCUSSION The undivided lateral cutaneous branch of second intercostal nerve is called as intercostobrachial nerve. Anatomy of Intercostobrachial nerve varies from person to person. By considering this fact study conducted by Cunnick et al9 classified anatomy of this nerve into six types: TYPE 1: ICBN arises from T2 alone and does not gives off any branc TYPE 2: ICBN arises from T2 alone and divides into large main trunk and a small branch TYPE 3: ICBN arises from T2 alone and divides equally into two branches. TYPE 4: ICBN formed by two equal branches from T1 and T2. No Significant branches. TYPE 5: ICBN formed by two separate T2 radical.No significant branches. TYPE 6: ICBN arises from T2 alone and has large main trunk and at least two small branches.
In another study conducted by Loukas et al10, out of 100 cadavers(200 axillae), 90 (45%) specimens were found to be type 1 variant , 50(25%) were found to be type 2 and 20(10%) were found to be type 3. Similar study conducted by Pulipatti Anilkumar4 found one ICBN on each side in 29 cadavers (72.5%), then two ICBN on each side in 8 cadavers (20%), then three ICBN on each side in 2 cadavers (5%) and five ICBN on each side in 1 cadaver (2.5%). Satyajeet et al11 in his study emphasised on the role of preservation of ICBN in breast cancer patients. At surgical dissection they found that 69.6% of patients were having type 1 variant followed by type 2. Type 5 and Type 6 variants were absent. Similar study conducted by Abdullah et al12 had shown that preservation of ICBN reduces the incidence of sensory deficit following axillary clearance. Another study conducted by Freeman et al13 stated that although preservation of ICBN increases the duration of the operative procedures but the postoperative sensory deficit is minimal. Eventhough the etiology of PMPS is multifactorial. The risk factors include younger age, increased body mass index, pre-operative pain, depression, anxiety, postoperative chemotherapy, radiotherapy, post-operative hematoma, and seroma formation, apart from ICB nerve injury.14 A benefit of preservation of the ICB nerve has been reported in several descriptive studies and includes a reduction in postoperative pain, improved sensation and reduced arm stiffness. In 1973 Aiyama.15 reported that he had identified in several cases a communication between MPN and the lateral cutaneous branch of ICBN. This communication was named the caudal pectoral nerve and, according to him, is 5% of the population have this variation. In these cases, if the communicating branch is distributed to the skin, MPN may be thought to contain a cutaneous branch. On the other hand, if this branch is distributed to the pectoralis major muscle, the lateral cutaneous branch of ICBN may be considered as containing a muscular branch to this muscle. But in our case out of 60 axillae we couldn’t find this type of variation.
CONCLUSION The present study has showed that dominant type of ICBN was not significantly different from that given in the literature. This anatomical knowledge will help the surgeons for the effective surgical practice .It is also advantageous to preserve the ICBN in surgeries for breast carcinoma to reduce the post mastectomy pain. It is always wise to know the normal course of the intercostobrachial nerve along with its variations, in order to avoid wrong diagnosis and iatrogenic complications during surgeries related to that area.
REFERENCES
|
|
 Home
Home