|
Table of Content Volume 6 Issue 2 - May 2018
An angiographic study in terminal branching pattern of popliteal artery and its clinical connotation
Elamathi Bose1*, Vijaya Ramanathan2, Sudha Seshayyan3
1Assistant Professor, 3Director and Professor, Institute of Anatomy, Madras Medical College, Chennai, Tamil Nadu, INDIA. 2Professor, Department of Anatomy, Meenakshi Medical College and Research Institute, Enathur, Kanchipuram, Tamil Nadu, INDIA. Email: ila007dr@yahoo.co.in
Abstract Background: Popliteal artery is the continuation of femoral artery traversing popliteal fossa from opening in Adductor magnus to distal border of Popliteus where it divides into Anterior and Posterior Tibial arteries. Aim: To study the variations in Popliteal artery and its branching pattern. Materials & Methods: It was a retrospective study to evaluate the variants in terminal branching pattern of popliteal artery using 128 slice CT. The study was conducted between July 2015 to September 2017 on a total of 50 lower limb angiographic films obtained from the Department of Radiology of various institutions. Variations in branching patterns were noted. Results: Normal level of popliteal arterial branching was observed in 95% of cases. Trifurcation pattern was seen in 2.5% of cases. High division of popliteal artery, with anterior tibial artery being the first branch, arising above knee was observed in 2.5% of cases. Conclusion: Knowledge of variations in the branching patterns of Popliteal artery is important for the following reasons: Surgical approaches & choice of suitable arterial graft site, awareness to vascular surgeons during arterial reconstruction in Femoro-popliteal by-pass graft procedure, management of Peripheral vascular diseases, for orthopaedic surgeons ,to reduce incidence of serious unexpected arterial injury during surgical procedure in & around knee joint & in Popliteal artery entrapment syndrome Key Words: popliteal artery.
INTRODUCTION Popliteal artery is the deepest neurovascular structure present in the popliteal fossa.1 It extends from adductor hiatus, a hands breadth above knee joint to the fibrous arch in soleus, a hands breadth below the knee, corresponding to the lower border of popliteus, where it divides into its terminal branches, anterior tibial artery(ATA) and posterior tibial artery(PTA).2 Senior et al propounded that the persistence of segments, abnormal fusion and segmental hypoplasia or aplasia in the lower limb vasculature, can contribute significantly to the anatomic variations in terminal branches of popliteal artery. The popliteal artery gains importance in being the commonest blood vessel to get involved in aneurysm due to atherosclerosis3 and in entrapment syndrome.4 The commonly associated vascular anomaly reported in club footis the absence of ATA i.e. 85%.Here the PTA with its branch, lateral plantar artery becomes the predominant vessel supplying the foot. Therefore, assuming the absence of ATA, the PTA has to be preserved during pre-planning a surgical correction for club foot.5 Invaso-occlusive diseases of lower limb. due to atherosclerosis, arteritis, diabetes and vascular malformations, there is natural development of compensating crural anastomosis from peroneal artery, a branch of PTA.This should encourage vascular surgeons to consider Peroneal artery bypasses during surgeries to maintain the vasculature of limb.6 Understanding these different branching patterns can be beneficial to radiologists, vascular and orthopaedic surgeons to interpret angiographic reports and specialise in performing surgical and interventional procedures in this region to avert any damage to the entire lower limb.5 With the advent of angiography there has been an increase in the success rate of vascular grafting, surgical repair of the blood vessels, transluminal angioplasty, embolectomy and in the diagnosis of arterial injury. The favourable outcome can be contributed to proper planning of these surgical interventions.7 There are many studies related to Digital subtraction angiography8,9,10, and a few studies have been reported on the terminal branching pattern of popliteal artery by Computed Tomographic Angiography (CTA).The arterial branching pattern can be ascertained and the lower limb arterial disease can be assessed with great accuracy using CTA which is a non-invasive technique. This is a retrospective study to evaluate the variants in terminal branching pattern of popliteal artery using 128 slice CT. MATERIALS AND METHODS Patient Selection: The study was conducted between July 2015 to September 2017 on a total of 50 lower limb angiographic films. 10 lower limb CTA had narrowing or occlusion of popliteal artery and their assessment for branching pattern could not be discerned. Hence 40 lower limb CTA data were retrospectively reviewed for their branching pattern. The study was approved by Institutional ethics committee along with informed consent obtained from all individuals included in this study. Imaging Technique and analyses: The CTA examinations were performed by GE Optima 660, 128 slice CT scanner. The patients were placed in supine position with feet first. The scan covered the area from celiac axis to the tip of foot. The antecubital vein was chosen and 18 gauge iv. canula was introduced, 80ml contrast Iohexol containing 350mg iodine/ml at a flow rate of 5ml/s was injected followed by 40 ml saline chase. The scan was initiated when the threshold reached 100HU in abdominal aorta. The CT images were transferred to a remote workstation and the data was processed by using maximum intensity projection, volume rendering, multiplanar and curved planar reformatting techniques. The arterial segments were studied in coronal section. Kim et al12 classified the branching pattern of Popliteal artery into Type I, II and III. The same scheme was utilised to classify the branching pattern of popliteal artery in the present study. Type I showed branching of popliteal artery (PA) at the normal level, i.e., below the level of medial tibial plateau. This had further three subgroups. Type IA (normal) the first branch is anterior tibial artery(ATA) with the main artery continuing as tibioperoneal trunk and further dividing into peroneal (PRA) and posterior tibial arteries (PTA). Type IB showed trifurcation of ATA, PTA and PRA. Type IC with PTA as its first branch and ATA and PRA arising from the common tibioperoneal trunk. Type II showed branching of PA above normal level and this also had three subgroups. Type IIA shows branching of popliteal artery at or above the joint space and further had two subdivisions as follows: Type II A 1 the ATA has normal proximal course posterior to popliteus muscle, Type II A2 ATA has proximal and medial course, anterior to popliteus muscle. Type II B shows branching of PTA as the first branch at or superior to joint level and branching of ATA and PRA from common tibioperoneal trunk. Type II C denotes branching of PRA as the first branch at or superior to joint level and a common trunk for anterior tibial and posterior tibial artery. Type III shows hypoplasia or aplasia of the branches of PA with alteration in distal blood supply. This has further three subgroups: Type III A shows hypoplasia or aplasia of PTA and the blood supply is replaced by PRA. Type III B shows hypoplasia or aplasia of ATA and dorsalis pedis is substituted by PRA. Type III C has hypoplasia or aplasia of ATA and PTA and distal substitution is by PRA. Statistical Analysis: The incidence of the different patterns was determined and compared with CT angiographic studies conducted earlier. Microsoft excel was utilised to give a descriptive analysis on the common branching pattern of terminal branches of popliteal artery.
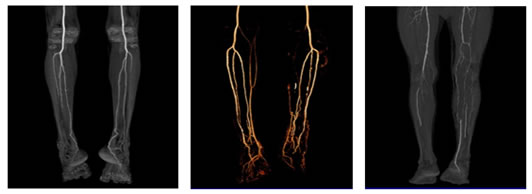
RESULTS A total of 40 lower limb angiographic films were evaluated for the branching pattern of popliteal artery in the current study. The frequencies of terminal branching patterns of popliteal artery, in the present study population are summarized in Table 1.The normal level of popliteal arterial branching, usual pattern Type IA (with anterior tibial artery as its first branch followed by the tibioperoneal trunk which then subdivides into peroneal and posterior tibial arteries) was observed in 38 limbs (95%) Fig:1. Normal level of popliteal arterial branching -Trifurcation pattern, type IB was seen in 1 limb (2.5%) Fig:2. High division of popliteal artery, with anterior tibial artery being the first branch, arising above knee and having a normal course posterior to popliteus muscle, Type IIA1 was observed in 1 limb (2.5%) Fig:3.
Figure 1: Showing CT Angiogram of Type IA normal branching pattern of popliteal artery Figure 2: Type IB- trifurcation of popliteal artery Figure 3: Showing Type IIA1 -High division of popliteal artery
Table 1: Distribution of the terminal branching patterns of popliteal artery
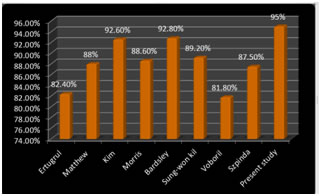
Figure 4: Compares the incidence of Type I A branching pattern of popliteal artery in different radiological studies DISCUSSION Type I A was identified to be the common branching pattern of popliteal artery in most angiographic studies with its incidence ranging from 81.8% to 92.8%.13,6,15,16,17 The radiological study of Kim et al 92.6%, and Bardsley et al18 92.8% correlates with the incidence of the present study 95% (Graph:1).Cadaveric study by Adachi et al 19 also revealed a high incidence 96% for Type I A branching pattern. Type I B pattern of branching was reported with an incidence of 0.4%-5.5%13,6,15,16,17. The present study showed an incidence of 2.5% which was close to the study by Szpinda et al 2.63%. Keen et al in a cadaveric study reported an incidence of 4.3% for Type IB pattern of branching. This trifurcating pattern poses technical challenge during angioplasty or embolectomy and thus assumes prime importance during interventional procedures.4 Type I C branching pattern was identified with an incidence of 0.1% to 1.97% 13,6,15,16,17. The present study had 0%incidence which coincided to the study done by Bardsley et al and Voboril et al. Type II A1 was reported with an incidence of 4.2% to 1.2% 13,6,15,16,17. The present study showed an incidence of 2.5% which was close to the study by Ertugrul et al 2.6% and Mathew et al 2.3%. Keen et al have revealed an incidence of 3.6% for Type IIA1 in their cadaveric study. High division of ATA is seen in Type IIA1 where the vessel will be in close contact with the posterior cortex of tibia and using sharp instruments as in total knee replacement will make the vessel vulnerable to injury. The adequate cognition about the ATA will also reduce arterial complications in surgical procedures like high tibial osteotomy, total knee arthroplasty, lateral meniscal repair, posterior cruciate ligament reconstruction, tibial tubercle osteotomy. The incidence of Type II A 2 is 1.3% by Ertugrul et al, 0.7% by Kim et al, 0.66% by Szpinda et al, 0.4% by Voboril et al. This branching pattern is absent in the present study 0% as reported by Mathew et al, Morris et al, Bardsley et al and Sung won kil et al. The incidence of Type II B is 5.9% by Szpinda et al, 2.4% by Voboril et al, 1.7% Bardsley et al, 1.5% by Ertugrul et al, 0.9% by Mathew et al, 0.8% by Kim et al and Morris et al, 0.4% by Sung- won kil et al and absent, 0% in the present study. The incidence of Type II C is 0.2% by Kim et al. This type of branching pattern of popliteal artery is absent, 0% in the present study which correlates with Ertugrul et al, Mathew et al, Morris et al, Bardsley et al, Sung-won kil et al, Voboril et al, and Szpinda et al. The incidence of Type III A is 5.1% by Sung won kil, 3.8% by Kim et al, 3.7% by Ertugrul et al, 0.9% by Bardsley et al. There is no incidence of this branching pattern in the present study 0%which coincided with the studies of Mathew et al and Morris et al. The incidence of Type III B pattern of branching is 2.3% as reported by Mathew et al, 2.2% by Ertugrul et al, 1.7% by Sung won kil et al, 1.6% by Kim et al. This branching pattern is absent in the present study which correlates with radiological studies conducted by Bardsley et al and Morris et al. Type III C pattern of branching of popliteal artery was reported with an incidence of 0.8% by Sung won kil et al, 0.2% by Ertugrul et al and Kim et al. The present study showed absence of incidence, 0% of this pattern and this correlated to the studies reported by Mathew et al, Morris et al and Bardsley et al. The lower limb arteries arise from two sources, one being the sciatic artery which is the axis artery, branch of internal iliac artery and the other being the primitive femoral artery, branch of external iliac artery21. The axis artery gives rise to the popliteal artery at the proximal border of popliteus muscle. The PA passes along the dorsal surface of this muscle and divides into PTA and primitive PRA, that lies superficial to tibialis posterior muscle. At the distal border of popliteus muscle, the PA gives away a branch, the anterior tibial artery which passes ventrally above the interosseous membrane and continues as the dorsalis pedis artery. The variation in the branching pattern of popliteal artery is determined by the embryonic vascular development from a combination of segments of sciatic artery and primitive femoral artery. Vascular grafting and repair is necessitated in atherosclerosis, emboli and trauma to these blood vessels. The choice of arterial vessel graft is greatly dependant on understanding the existing variations. The popliteal artery may be a continuation not of femoral artery, but of the sciatic artery (a branch of inferior gluteal artery). When this occurs, the popliteal artery has an abnormal relationship to popliteus1. It runs deep to the muscle before dividing into its terminal branches and can get occluded when the muscle contracts. This condition is known as popliteal artery entrapment syndrome22 and presents with claudication on exercising. Therefore, the embryologic development and subsequent anatomic variations does bear significant clinical implications.
CONCLUSION In the present study 5% variations was observed in branching pattern of terminal branches of popliteal artery. It is necessary to determine these variations by CTA which gives excellent images, is faster, is comfortable for patients, gives better spatial resolution before surgical intervention is planned in the lower limb. Professionals working with angiography, duplex ultrasound, magnetic resonance angiography and computed tomographic angiography should appreciate the existence of these variations so as to avoid misinterpretation of results. The vascular surgeons will be benefitted by knowing the incidence of branching patterns of popliteal artery. It can assist them during arterial reconstruction in femoro-popliteal bypass graft procedure, in choosing suitable arterial graft sites, during management of peripheral vascular disease and popliteal artery aneurysm which is the most common peripheral aneurysm due to atherosclerosis. Knowledge of these variations will be of potential consequence to orthopaedic surgeons to prevent vascular injuries while performing surgeries around knee joint, surgical procedures on fractured segments in distal femoral and proximal tibiofibular region and in total knee arthroplasty. This information can be utilised by interventional radiologists for the safe performance of infra popliteal interventions such as bypass surgery, transluminal angioplasty and subintimal angioplasty.
REFERENCES
|
|
 Home
Home