Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 2 - August 2019
Evaluation of lipid profile in CKD patients on hemodialysis with control population: A hospital-based study
Mandarapu Roopalatha
Associate Professor, NRIMS, Visakhapatnam, INDIA.
Abstract Background: Lipid disorder is very much frequent in chronic kidney disease (CKD) patients and is dependable for cardiovascular disease (CKD) which is mainly general source of mortality in them. So, it is essential to study the lipid profile in CKD patients in dialysis to avoid morbidity and mortality. Materials and Methods: All the subjects in this study consisted of 60 patients with CKD undergoing Haemodialysis. The 60 control subjects were enrolled at Department of Biochemistry, Pinnacle Hospital Visakhapatnam, during the period of January 2017 to July2018.A venous blood sample was obtained from each patient and control subsequent to an overnight fast for evaluation of lipid profile and other blood parameters. Results: The mean of total cholesterol (215.7 ± 32.8 mg/dL) and triglyceride (149.91 ± 46.5 mg/ dL) was higher when compared with that of controls (152.5 ± 13.5 mg/dL and 109.1 ± 28.6 mg/dL) respectively. Similarly, a prominent level of LDL Cholesterol was also observed in CKD patients as compared to controls. (139.12 ± 18.1 mg/dL versus 101.01 ± 14.9 mg/dL) There was a minor decrease in HDL Cholesterol in study patients (40.01 ± 6.91 mg/dL) when compared with controls (49.89 ± 5.2 mg/dL). Conclusion: Our study outcomes indicate that patients undergoing hemodialysis show significant abnormalities of triglycerides, total cholesterol, and LDL-cholesterol levels were elevated in the CDK group compared to controls. All were statistically significant. There was a negative association exists among HDL- cholesterol level, where as serum creatinine levels which were statistically significant. There was a significant decrease in HDL-cholesterol and increase in TGLs in both conventional and hemodialysis groups. The present study underscore the need for early evaluation of these patients for lipid abnormalities as prompt treatment may prevent cardiovascular measures and delay the development of kidney disease. Key Words: Haemodialysis, Dyslipidemia, Hyperlipidemia, Chronic kidney disease
INTRODUCTION Chronic kidney disease (CKD) has turn out to be a public health problem with a worldwide prevalence of around 8–16%1 Mortality rates among dialysis patients have been declining 2–3% per year since 2001 (28% reduction), and in 2012 reached a level comparable to rates reported in 1982.2 Data from National Health and Nutrition Examination Survey showed that CKD prevalence among ages 60 and above increased from 18.8% in 1988-1994 to 24.5% in 2003-2006.3 Cardiovascular diseases (CVD) remain the major basis of death among patients with kidney diseases still after renal replacement therapy is reached, more than half patients die, mostly for Cardiovascular causes due moreover to uraemia-related cardiovascular risk factors (such as anaemia, hyperhomocysteinemia, mineral bone disease-CKD with hyperparathyroidism, prothrombotic factors, hypoalbuminemia, chronic inflammation, oxidative stress) or to traditional ones (age, gender, diabetes, obesity, hypertension, smoking, insulin levels, family history, Dyslipidemia 4. Along with the last causes Dyslipidemia represents one of the most important, potentially improvable risk factor 5. Since hyperlipidemia can be modulated by beneficial interference, it is valuable to study and evaluate lipid profile abnormalities in chronic kidney disease patients. Indian studies on lipid abnormalities in CKD have not been reliable. Few studies found that hyperlipidemia 6, whereas In the review Cases A et al.7 by observed hypertriglyceridemia and summary high-density lipoprotein (HDL) levels in CKD patients as in western countries. In view of discrepancy and incomplete confirmation in the North coastal part of Andhra Pradesh, it was determined to study the serum lipid profile in CKD patients undergoing long-term continuation haemodialysis.
MATERIALS AND METHODS All the subjects in this study consisted of 60 patients with CKD undergoing Haemodialysis. The 60 control subjects were enrolled at Department of Biochemistry, Pinnacle Hospital Visakhapatnam, during the period of January 2017 to July2018. The haemodialysis regularity of study group was two to three times per week and each session lasts for four hours. General information of each patient (age, sex, BMI, duration and frequency of HD, underlying renal disease, and family history of hypertension, hyperlipidemia and myocardial infarction) were recorded. Patients with acute renal failure and nephrotic syndrome, Diabetes, liver disease, Cushing’s, or other metabolic disorder and those who are on drugs affecting lipid metabolism such as β-blockers, statins, and oral contraceptive pills and pregnant women were excluded from the study. Five ml of venous blood was drawn aseptically from the antecubital fossa of each patient and control after an overnight fast for lipid profile determination. Blood was allowed to clot and serum was separated after centrifuging the samples. Other biochemical parameters like urea, creatinine and serum electrolytes along with the lipid parameters - total cholesterol, triglycerides, LDL and HDL cholesterol were also analysed. All the parameters were estimated using commercially available kits on fully automated autoanalyser. The serum total cholesterol and high density lipoprotein cholesterol (HDL) were analyzed using cholesterol oxidase CHOD-PAP method, triglyceride by GPO-PAP method while low density lipoprotein cholesterol (LDL) was obtained using Frieldwald formula: LDL cholesterol= Total cholesterol − TGL÷5 – HDL cholesterol. And the data obtained was statistically analyzed using M.S Excel 2010 to determine the mean and standard deviation.
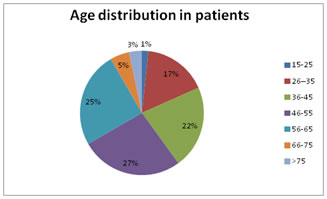
RESULTS Age of the cases varied from 17 years to 82 years. Male and female ratio distribution was shown in table 1. Majority of patients fall in the age group between 26 and 65 years. The mean age in this study was 48.75 years (Graph 1).The weight of patients (65.5 ±14.7kg) was greater than that of the controls (57.8±12.5kg). Likewise comparing the body mass index, it was found to be high in patients (23.2±6.9 kg/m2) than that of the controls (17.9±3.6kg/m2). Both the systolic (158.1 ± 26.61mmHg) and diastolic (90.1 ± 19.2 mmHg) blood pressure in patients were high when compared to that of the controls (117.9 ± 5.2 mmHg and 78.9 ± 5.3mmHg respectively). The mean values of urea (119±41.8 mg/dL) and creatinine (8.02 ±4.29 mg/dL) in CKD patients were found to be very high as compared to controls (29.1±4.9 and 1.3±0.7 respectively). The mean values of serum sodium and potassium in CKD patients were (129.06±5.1 and 5.01±4.1mmEq/L) correspondingly. When compared to controls (140.3±4.6 and 3.6±1mmEq/L) correspondingly representing the electrolyte imbalance in them. The lipid profile pattern in the CKD patients and the controls were compared. The mean of total cholesterol (215.7 ± 32.8 mg/dL) and triglyceride (149.91 ± 46.5 mg/ dL) was higher when compared with that of controls (152.5 ± 13.5 mg/dL and 109.1 ± 28.6 mg/dL) respectively. Similarly, a prominent level of LDL Cholesterol was also observed in CKD patients as compared to controls. (139.12 ± 18.1 mg/dL versus 101.01 ± 14.9 mg/dL) There was a minor decrease in HDL Cholesterol in study patients (40.01 ± 6.91 mg/dL) when compared with controls (49.89 ± 5.2 mg/dL). The prevalence of Dyslipidemia from lipid profile components in the study population: Total cholesterol (41.4%), HDL (11.6%), LDL (15%) and triglyceride (32%) were shown in table 2. Table 1: Sex distribution among CKD and control subjects
Table 2: Prevalence of Dyslipidemia in the study subjects
DISCUSSION This study was conducted to conclude the lipid profile changes in CKD patients on conventional management and regular hemodialysis and to evaluate them with normal healthy controls. The study population was 120, of which 60 were patients and 60 were controls. They were preferred as per the inclusion criteria. Serum TC, HDL cholesterol (HDL-C), LDL-C, and TGLs were considered using autoanalyzer. The results were statistically analyzed. In our study, the hit frequency of CKD was among 26 and 65 years of age. Patients with CKD were establishing to have elevated BMI as compared to the controls, which showed that weight raise is a risk factor of CKD. (Saul Pampa Saico et al 2016)8. The indicate values of both systolic and diastolic blood pressure were elevated in CKD subjects as compared to that of the controls. This was not unexpected as hypertension was the one of the important reason of CKD in this study. The incidence of hypertension in these patients could increases the progression of dyslipidaemia and development of CKD. 7 Our study reported that the signify values of all the lipid profile deliberate were elevated than those of the controls. It underscores the significance of evaluating CKD patients for lipid disorders as lipids add in a straight line to glomerulosclerosis and tubulointerstitial injury and that alteration of lipid abnormalities related with renal disease will slow the development of chronic kidney disease. (Wahl P et al 2016).9 Cardiovascular (CV) disease is the most important root of mortality in patients on continuation haemodialysis (MHD) accounting for approximately 50% of deaths. Dyslipidemia develops near the beginning in renal failure and it becomes additional different as the renal disease progresses since of disproportion between lipoprotein synthesis and degradation due to impaired activity of lipoprotein lipase and straight inhibitory consequence of a variety of uremic toxins on the enzymes concerned in lipid metabolism. The distorted lipoproteins are in turn in use up by the hunter receptors on macrophages and vascular smooth muscle cells, which are amplified in uraemia, favouring the progress of atherosclerotic plaques.10. An antagonistic positive approach is essential in the management of CKD and this will contain the control of hypertension, smoking, infections, dyslipidaemia, diabetes mellitus, and alcohol consumption. The must to strengthen attempt on health instruction and screening of general public for CKD and dyslipidaemia cannot be over emphasized. Regular counseling and hopeful substantial activity in MHD patients has possible to recover physical performance, optimizing the superiority of life and probably improving the plasma lipids and lipoprotein pattern.
CONCLUSION Our study outcomes indicate that patients undergoing MHD show significant abnormalities of triglycerides, total cholesterol, and LDL-cholesterol levels were elevated in the CKD group compared to controls. All were statistically significant. There was a negative association exists among HDL- cholesterol level, where as serum creatinine levels which were statistically significant. There was a significant decrease in HDL-cholesterol and increase in TGLs in both conventional and hemodialysis groups. Decrease in HDL is further in conventional management and raise in TGLs is more in hemodialysis group which could contribute to atherosclerosis and cardiovascular disease and may enhance the morbidity and mortality of CKD subjects. Additional investigations have to be done to substantiate whether untimely detection and management of this Dyslipidemia is somewhat promising, in the prevention of unfavorable clinical outcomes in predialysis CKD patients and in those on maintenance haemodialysis.
REFERENCES
|
 Home
Home