|
Table of Content Volume 14 Issue 2 - May 2020
Prevalence of surgical site infection in a tertiary care hospital: A prospective study
B Sudhakar Babu1, G Aparna2*, Prasada Rao Namburi3
1Associate Professor Of Community Medicine, Viswabharathi Medical College, R.T.Nagar, Penchikalapadu, Kurnool, INDIA. 2Associate Professor Of OBG, Government Medical College, Nizambad, INDIA. 3 Assistant Professor Of Microbiology, Fathima Medical College, Ramarajapalli, Kadapa, INDIA. Email: babusudhakar@gmail.com , aparnaganduri@gmail.com , raomcr@yahoo.com
Abstract Background: Surgical site infections (SSI) are the major contributor to patients mortality, morbidity and increased stay in the Hospital. The present study is undertaken to determine the frequency and risk factors of surgical site infections at tertiary care hospital in Kadapa. Methods: This cross-sectional, prospective study was carried out over a period of one year. Approval to conduct the study was obtained from the Institutional ethics committee. 250 patients who underwent surgery in General Surgery, OBG and Orthopaedics were included in the study. Risk factors were analyzed to predict SSI. After surgery, patients were followed during the stay in the hospital and after discharge on OPD to have a checkup for any sign of SSI Results: 19.2 % of operated patients had SSI and risk factors for SSI are increased age, Obesity, Anemia, Hypertension, Diabetes Mellitus, and prolonged pre-operative stay Conclusions: high incidence of SSI is observed in this study. Paying close attention to identified risk factors will reduce the burden of SSI. Keywords: SSI, nosocomial infections, risk factors, BMI
INTRODUCTION Surgical Site Infection (SSI) is defined as infection occurring within 30 days after a surgical procedure and affecting either the incision or deep tissues at the operation site. These infections may be superficial or deep or involving an organ space.1 Surgical site infections (SSIs) are among the most frequent nosocomial infections after surgery. SSIs affect patients by increasing morbidity and mortality and they affect economy of health care systems by increasing the length of hospital stay and costs.2 Surgical site infections (SSI) are serious postoperative complications with significant impact on morbidity and mortality. According to the National Nosocomial Infections Surveillance (NNIS) system, SSI are the third most frequently reported nosocomial infections, accounting for 12%-16% of all nosocomial infections among hospitalized patients.3 Postoperative wound infections delays recovery and often increases length of stay and may produce lasting sequelae and require extra resources for investigations, management and nursing care. Therefore, its prevention or reduction is relevant to quality patient care. 4 SSIs increase the rate of re hospitalization; the use of health care, diagnostic, and therapeutic resources; and hospital costs. The shorter the hospitalization time is for surgery, the lower the risk of infection.5 Notably, the risk factors for the development of SSIs may be related to the patients and the surgical procedures themselves. So the present study was undertaken to study the prevalence and risk factors of SSI among the patients who undergone surgeries in the departments of General Surgery, OBG and Orthopaedics.
MATERIAL AND METHODS Study subjects: two hundred and fifty patients who underwent various surgeries in the General Surgery, OBG and Orthopaedics departments of Fatima Medical College and General Hospital were studied. Study setting: Fathima Medical College and General Hospital which is a tertiary care teaching hospital in Kadapa Study design: prospective cross sectional study Study period: December 2018 to November 2019 Inclusion criteria: Elective surgeries and patients willing for the study Exclusion criteria: Grossly contaminated or infected wounds/procedures and patients unwilling for the study Ethics: This study was started after a prior approval by the Institutional Ethical Committee and obtaining consent from the patients. During the study period, after obtaining informed consent to be a part of the study, data were collected as per a predesigned questionnaire for all the patients who underwent surgeries. Demographic characteristics like age and sex were noted. Variables like BMI, Anemia, smoking status, Hypertension and Diabetes Mellitus and preoperative waiting period were compared in the infected and non-infected groups. After surgery, the patients were monitored daily for any signs of SSIs as per the CDC (Centre for Disease Controland Prevention) definition. Patients were followed after discharge on OPD (Out Patient Department) basis twice or thrice weekly for up to 30 days to have a checkup for any signs of SSIs. Patients with SSI were identified as per the following criteria6 • Involving skin and subcutaneous tissue at surgical site with any one of the following:
RESULTS Out of 250 patients who underwent surgeries at surgical wards of General Surgery, OBG and Orthopaedics, 48 patients developed SSIs.
Table 1: Incidence of SSIs
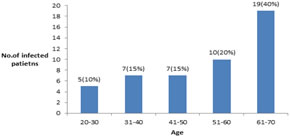
The highest incidence of SSI was observed among male patients (52.1%) compared to female patients (47.9%) which is shown in Table 2. The highest incidence of SSI (40%) was observed among the patients aged 60-70 years and the lowest incidence of SSI (10%) was observed among the patients aged 20-30 years which is shown in Fig 1 Table 2
Incidence of SSI in relation to age group
Figure 1: Age wise incidence of SSI Among patients with SSI, risk factors were Obesity (46%), Anaemia (42%), Diabetes Mellitus (21%), Hypertension (4%) which was shown in Fig.2 and Fig.3 and Incidence for the patients with preoperative stay of 10-15 days was 67% which was shown in Table 3.
Figure 2: Incidence of SSI in relation to BMI
Figure 3: Incidence of SSIs in relation to Comorbidity
Table 3: Incidence of SSI in relation to preoperative stay
DISCUSSION The aim of the study was to estimate the prevalence and risk factors of SSI. The incidence of SSI in our study was found to be 19.2%. Our findings were comparable with many other studies. A.R.Jamali et al.7 and Srivastava et al.8 in their studies found the prevalence of 19.2% and 20.1% which was similar to our study. In our study it was found that SSI was highest (40%) among patients aged 61 years and above are more prone to SSI than younger women. This was because increasing age is correlated with greater likelihood of certain chronic conditions, malnutrition and a fall in the body's immunological efficiency, causing more extensive SSI. 9 Johnson et al. in their study found increasing age a significant risk factor for overall SSIs. 10In our study it was found that patients with comorbidity are more prone to SSI. Out of which Obesity was found in 46%, Anaemia in 42%, Diabetes Mellitus in 21%, and Hypertension in 4% patients. Waqar11 in his study found that out of 117 SSI patients, obesity was found in 13%, undernutrition in 13%, Malignancies in 15% patients. In our study it was found that incidence of SSI was more when the pre hospital stay was more than 5 days. Kowli et al. found an infection rate of 17.4% when preoperative stay was 0-7 days, and an infection rate of 71.4% with a preoperative stay of more than 21days.12 Anvikar et al. demonstrated that preoperative hospital stay predisposed an individual to 1.76% risk of acquiring an infection. With an increase in preoperative stay, the risk increased proportionally. A preoperative stay of one week increased the risk rate to 5%.13 CONCLUSIONThe incidence of Surgical site infection in our study was 19.2%. The factors affecting rate of infection were patients age, BMI, Anemia, Diabetes Mellitus, Hypertension, duration of pre‑operative hospitalization.Acknowledgement: The author wishes to thank Dr. N Mary Hemeliamma, Professor and HOD, Department of Microbiology for her valuable suggestion.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Community Medicine (Print ISSN: 2579-0862) (Online ISSN: 2636-4743) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home