|
Table of Content - Volume 22 Issue 1 - April 2022
Prevalence of undernutrition and associated factors among under five children
Amit Vasant Deshpande1*, Baer Philip Ravikumar2
1Associate Professor, 2Professor And H.O.D., Department of Community Medicine, Mamata Medical College, Khammam, INDIA.
Abstract Background and aims: Under nutrition in under 5 children continues to be major public health challenge both on a global scale as well as in India. Aim of the present study was to assess prevalence of undernutrition and its associated factors in under five children in a rural district of Telangana. Methods: The present study was crossectional in design and conducted in 20 Anganwadi Centres chosen by systematic random sampling among 384 children under five years of age. History of socio-demographic factors, respiratory tract infections and diarrhoea and infant and child feeding practices were elicited from mother. Anthropometric measurements of the children were performed and duly recorded as per WHO standard manual. Results: Mean age of children was 3.45(±0.94) years, Median age was 3 years. There were 196(51.54%) male children and 188(48.96%) female children. Among total 384 children; prevalence of stunting, wasting and underweight were 26%, 19% and 23% respectively. Mother's education, BMI, height, wealth index, child birth-weight and sex were factors significantly associated with stunting, wasting and underweight. Conclusions: Prevalence of undernutrition specifically stunting and underweight is high in underfive children of rural district in Telanagana. Maternal literacy, family size and faulty infant and child feeding practices were factors significant associated with undernutrition. Keywords: Under-nutrition, Under 5 children; stunting; Under-weight; Wasting; infant and child feeding practices.
INTRODUCTION Under nutrition is defined by measurements that are below 2 standard deviations under the normal weight-for-age (underweight), height-for-age (stunting) and weight-for-height (wasting).1 In children under 5 years, under nutrition continues to be major public health challenge; in 2020 globally 149 million children under 5 years were estimated to be stunted and 45 million were estimated to be wasted. (2)Undernutrition is linked to 45% of deaths and several morbidities among children under 5 years which occur mostly in low- and middle-income countries. In India too, the burden of under nutrition is considerable with prevalence of stunting being 35% and 32.2% under five children being currently underweight.3 Malnutrition may affect growth and prevent children from achieving their optimum height/weight for age. Poor congnitive development, behavioural abnormalities and poor scholastic achievement have been reported. Long lasting effects include risk of developing obesity, diabetes, hypertension and consequently cardiopathies.4 Etiology of undernutrition is complex and multifactorial. Determinants of undernutrition are largely environmental and include poverty and disease (mainly diarrhoea, respiratory infections and parasites),lack of education, natural disasters and poor access to health care.Other factors are inadequate food consumption during growth (insufficient energy, good quality protein, vitamins and minerals); deficiency in gastrointestinal absorption and/or increase in demand, or even by an excessive excretion of nutrients.5 Undernutrition usually manifests early between the age of 6 m to 2 years.Assessment of prevalence of undernutrtion and factors associated with it in children under five years canaid in planning family specific nutritional interventions keeping into account the educational and socioeconomic status along within fant and child feeding and cultural practices.Some studies have however documented positive effects of nutritional recovery on weight and height, body composition. Similarly, the Integrated Child Development Services programme for children from 0-6 years which is being implemented in India since 1976 incorporates several schemes including supplementary nutrition, growth monitoring to combat malnutrition in under five children. (4). Under five beneficiaries of ICDS provide a cohort which can be monitored after assessment of nutritional status. Inspite of the above, there are relatively few studies from Indian subcontinent assessing factors associated with undernutrition. Thus the present study was conducted to assess nutritional status prevalence of undernutrition and its associated factors among under five children in a rural district of Telangana.
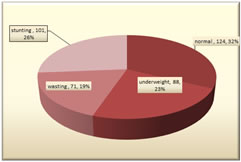
METHODOLOGY Approval from the institutional ethical committee was obtained prior to commencement of the study. Sample size: the minimum sample size was determined using the formula n=4pq/d2 wherep=prevalence, d= absolute precision and with 95% confidence interval. Prevalence was taken as 32%3 with absolute precision of 5% and was calculated at 338. Study design: The present study was a crossectional study conducted in rural area in Telangana over a period of 6 months. Study Population: A list was made to include all Anganwadis in the area of study. By systematic random sampling every fifth anganwadi was selected. The concerned anganwadi workers (AWC) and ASHA worker were contacted and Anganwadis were visited on days allotted by them. All children under 5 years present were included in the study. Revisit was made to examine absent children on other allotted days. A total of 18 Anganwadi centres were visited. Data collection instrument was a semi-structured pretested questionnaire. Mothers were interviewed and their age, education and family size were recorded. A person who could not read and write was labeled as illiterate.10 According to years of schooling educational status was classified as education up-to 6th standard (primary) and 7th to 10th standard, 12th, Graduate and above. Birth history of child, breast feeding commencement, duration, introduction of complementary feeding; history and current feeding practices were noted. History of recent (last fortnight) episode of respiratory tract infection and/or diarrhea was duly noted. Anthropometric measurements of the children were performed and duly recorded as per WHO standard manual.11 Age was recorded as completed years. Weight was measured using portable (LIBRA) weighing scale calibrated to nearest 100g and the scale was zeroed for each measurement. Height was recorded using portable stadiometer to nearest 0.1cm. Children were measured without footwear in light clothing. Mid arm circumference was recorded by measuring tape to nearest 0.1 cm. General examination was done for pallor, dental caries and skin changes due to vitamin deficiencies were noted. Underweight, wasting, and stunting were computed using weight and height measurement.1 Statistical Analysis: Data were entered into MS Excel and transferred into IBM SPSS version 20.0 software for further analysis. Data were checked for its’ completeness and consistency. `Numerical data were presented as mean, median and standard deviation. Categorical data was presented as frequencies and proportions and significance of difference between proportions was analyzed using Fischer’s exact test or Chi square test as applicable and P value of <0.05 was considered significant. Significant variables were considered as associated factors for undernutrition. RESULTS The study was finally conducted with 384 children. Mean age of children was 3.45(±0.94) years, Median age was 3 years. There were 196(51.54%) male children and 188(48.96%) female children. Among total 384 children; 124(32%) children had normal nutritional status and 88(23%) children were underweight (low weight for age). The prevalence of wasting was 19 % (low weight for height) and 101(26%) children were stunted (low height for age). Maternal literacy, birth weight, and faulty infant and child feeding practices (not initiating breast feeding within 1 hr of birth, not being exclusively breast fed for 6 months, delayed introduction of complementary feeding, inadequate nutrient intake) were found to be significantly associated with undernutrition in children under five years of age as depicted in table 2.
Figure 1: Prevalence of undernutrition in children under 5 years Table 2: Factors Associated With Under nutrition in Under 5 Children
P<0.05*: statistically significant P<0.001**: highly significant statistically
DISCUSSION In the present study, prevalence of stunting was 26%, 23% children were underweight (low weight for age) and 19% children were wasted (low weight for height). Prevalence of stunting, wasting and underweight is lower than undernutrition prevalence in overall Telangana state (2019-20) (NFHS-5) where the prevalence of stunting, wasting and underweight was 33.1%, 21.7% and 31.8% respectively. Child stunting in India has shown downward trend; it dropped by 10 percent (from 48% to 38%) over the 10-year period (2006 to 2016) but still remains unacceptable.14 Varied prevalence of undernutrition has also been reported by other recent similar studies; in 2017prevalence of stunting ranged from 16.4% to 62.8% among the 723 districts of India.16A study in tribal areas7 of western India, underweight and stunting prevalence was almost double (64% and 61%) respectively of national prevalence. In a recent study in urban slums and rural area of Maharashtra, prevalence of wasting, stunting and underweight was 17.1%, 45.9% and 35.4% respectively.6 Ina recent systematic review; overall estimate of prevalence of stunting, wasting and underweight were 43.4%, 17.8% and 35.5%15 respectively. Variations and inequalities in magnitude of burden of undernutrtion are seen between districts; inequalities increased for stunting in 28 out of 31 states from 2010 to 2017, for wasting in 16 states, and for underweight in 20 states.16 Lower prevalence in the present study could be due to difference in study population as the present study included children enrolled in ICDS scheme and had been receiving supplementary nutrition, growth monitoring, health check up and nutrition health education. Children included in NFHS and other studies are from general population and would also include children not enrolled in ICDS scheme, children of migrant and other disadvantaged sections of the population. Factors associated with undernutrition: In the present study maternal literacy, family size and faulty infant and child feeding practices (not initiating breast feeding within 1 hr of birth, not being exclusively breast fed for 6 months, delayed introduction of complementary feeding, inadequate nutrient intake) were factors associated with undernutrition. Comparable findings have been reported by other similar studies.Undernutrition was associated with literacy of mother, household wealth index and morbidities.7 History of diarrhea in past 2 weeks, male gender, illiterate fathers and larger completed family size, age of initiating complementary feeding were significantly associated with being underweight.9,12 Unsafe drinking water and sanitation, short maternal stature, acute respiratory infections and diarhoea and awareness regarding the conditions were also determinants of undernutrtion.13 Child stunting prevalence was higher among poorer compared to wealthier households.14 Mother's education, BMI, height, wealth index, child birth-weight and sex were also factors significantly associated with stunting, wasting and underweight.15 Stunting results from chronic malnutrition and continued prevalence of nearly 1/3rd of under five children being stunted and underweight is alarming despite more than four decades of social welfare programmes. Factors associated with malnutrition have included parental education, lower socioeconomic status and faulty infant and child feeding practices as described above.,9,12-15 Potential interventions to address the above factors for reducing undernutrition in under-five children could be nutrition health education and counselling with practical demonstrations of preparation nutrient dense meals using local cost effective ingredients incorporated and made a part of RMNCH+A strategy.Under this, Adolescent and pregnant and lactating mothers can acquire skills on correct infant and child feeding practices along with antenatal and postnatal nutritional education. Private organizations working in field of women and child health can be enrolled as private providers of supplementary nutrition for migrant, street and urban slum children. Regular consumption of nutrient poor and calorie dense junk food by children is widely prevalent even in lower socioeconomic house-holds. Regulatory approaches can be adopted to discourage production, marketing, advertising and consumption of unhealthy, ultra-processed foods, beverages, and snacks. Strengths And Limitations: Findings of the present study add to the scarce evidence base of prevalence of under-nutrition and its associated factors in under five children residing in a rural district of Telanagana. Limitations include relatively smaller sample size.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home