Official Journals By StatPerson Publication
|
Table of Content-Volume 4 Issue 3 December 2017
Affect of flap and flapless implant placement on crestal bone level and implant stability
Sonam Rana1*, Ashish Verma2, Pooja Palwankar3, Nipun Dhalla4, Esha Tyagi5
1BDS, MDS(Periodontist), 2Professor, 3Professor and HOD, 4Reader, Department of Periodontology, Manav Rachna Dental College, Sector-43 Delhi- Surajknd Road Faridabad Haryana-121004, INDIA. 5Post Graduate Student, Army College of Dental Sciences Sikandrabad, INDIA. Email: drsonamrana@gmail.com
Abstract Aim: The aim of the present study was to analyze the effect of Flapless and flap implant placement technique on implant stability and crestal bone level at different time intervals 3 weeks, 3 months and 9 months. Material and Method: A total of 2 implants were placed in 2 healed molar sites with an age group of 18-45 years of both the sexes in each group (i.e. flapless and flap technique). Implant stability was measured at the time Resonance Frequency Analysis using Osstell Mentor® device. Crestal bone was measured by RVG (Radiovisiograpy). Results: All Implants exihibited clinically and radiographically successful osseointegration. The mean ISQ value in the Flapless group was observed to be 63.007.071, 64.001.414, 72.503.56 and 79.500.707 at the time of insertion, 3 weeks, 3 months and 12 months respectively. RFA mesuurements for flapless group was higher as compared to flap implant placemnt technique. Crestal bone level the mean difference in mesial bone loss from 0-3 months and 0-12 months was significantly more among Flap implant placement technique. The mean difference in distal bone loss from 0-3 months was significantly more among Flap implant placement technique and mean difference in distal bone loss from 3-12 months was significantly more among Flapless implant placement technique. Conclusion: The flapless technique showed favourable conditions with regard to implantstability and crestal bone level. Key Words: Flapless Implant Placement, Flap implant Placement Implant Stability and Resosnance Frequency Analysis.
With the improved medical care and increased life expectancy, the population of elderly people has increased with rise in number of edentulous patients. This has resulted in increased acceptance of dental implants as a rehabilitation procedure for missing teeth and has increased the demand of dental implants therapy in recent years. Implants is a fairly successful procedure. Albrektsson et al (1986)1 proposed that a dental implant is considered successful when it is immobile clinically and radiographically there is no evidence of peri-implant radiolucency. Furthermore, in the subsequent years, bone loss should be less than 0.2 mm annually with no persistent pain, discomfort or infection. Adell et al (1981)2 were the first to quantify and report marginal bone loss. Their study indicated greater magnitude and occurrence of bone loss during first year of prosthesis loading, averaging 1.2mm with a range of 0-3mm. Years subsequent to the first showed an average of 0.05- 0.13mm bone loss per year. The number of procedures have been performed to overcome the crestal bone loss like implant size, implant collar design and implant placement procedure (crestal or subcrestal).The elevation of flap during implant placement is also important factor in determining the amount of marginal bone loss following implant placement. The present case report compares the effect of flap and flapless implant placement on crestal bone level during healing phase and following prosthesis placement.
MATERIAL AND METHOD The present pilot study is a randomised clinical trial comparing two implant placement approaches based on clinical radiographic and implant stability outcomes. The study was conducted between September 2016 and September 2017at the department of Periodontology of Manav Rachna Dental College. Study Population: Four patients from the patients referred for implant placement to the Department of Periodontology were enrolled in the study. The sample population comprises 1 male and 1 female in flap technique and 1male and 1 female in flapless technique with an age range from 18 to 40.All patients read and signed an appropriate informed consent document prior to participation in the study and agreed to attend all scheduled follow-up appointments. Inclusion Criteria: To be included in the study, all subjects had to be > 18years of age, periodontally healthy and partially edentulous, missing one or more teeth which was/were planned to be restored with fixed implant supported restorations bone architecture without undercuts, and at least 5mm width of keratinized tissues were also required. Implants were placed in extraction sites after at 3 months of postextraction healing. Exclusion Criteria: Subjects with systemic diseases affecting the healing process (eg. Uncontrolled diabetes mellitus) were excluded from the study. Smokers (> 10 cigarettes/day ), Pregnant lactating women, individuals who used antibiotics the last 3 months and patients requiring guided bone regeneration for implants placement and parafunctional habits present and any psychiatric problem were also excluded. Surgical technique: The implants were placed under local anesthesia with 2% lidocaine. All patients received a loading dose of 1 g amoxicillin 1 h before the implant surgery and rinsed preoperatively for 60s with a 0.12% chlorhexidine solution to reduce the total mouth bacterial load. All implants were placed at the bone level according to the manufacturer’s instruction. Healing abutments were inserted at the surgical procedure. In the control group (flap) intrasulclar incisions were made on the buccal and lingual surfaces of the adjacent teeth and midcrestal incisions were carried on the edentulous areas. Full – thickness mucoperiosteal flaps were elevated, exposing the underlying bone. After healing abutment insertion, the flaps were sutured with 4/0 vicryl (Ethicon FS -2 ) Amoxicillin (1g three times/day for 1 week ) were prescribed postsurgically. Patients were instructed to rinse twice daily with a 0.12% chlorhexidine mouthwash for 15 days sutures were removed after 1 week. In test tube (flapless)-The thickness of the soft tissue at the site of implant was measured with the help of periodontal probe by punching it at the implant site. Surgery was performed under local anesthesia. The implant site was prepared with standard drills. To ensure primary stability, the drilling protocol included under preparation of the implant site without screw tapping or countersinking. Implant was placed at the bone level according to the manufacturers instruction. with minimum insertion torque of 35 Ncm. After healing abutment was inserted at the end of the surgical procedure, Immediately following the healing abutment placement a standardized RVG with XCP holder was taken. Amoxicillin (500mg three times per day, metronidazole 150 mg three times a day for 1 week postoperatively was prescribed. RFA Measurements: The first time Generation Osstell Instrument (Osstell Gothenburg, Sweden) was available. The ISQ value were recorded immediately after implant placement (surgery, baseline = ISQ 1) at 3 weeks (ISQ-2) after period of 3 months (ISQ 3) before functional loading with the temporary crown and final reading after 12 months (ISQ 4) of implant placement before the functional loading with the final ceramic crown. The transducer was always mounted in the bucco lingual direction that is in the right angle to the jaw. Equal values should be reached by three times testing. If the differences between the three records were more than two values, the measurements were repeated after a short waiting period. Radiographic evaluation: A baseline digital periapiacal radiograph was taken immediately after implant placement with the parallel technique, using a customized silicon biteblocks for each patient. The bite block were saved and reused for the radiograph which was taken 3 months postoperatiely and final radiograph after 12 months postoperatively. The implant fixture healing abutment interface was utilized as a reference point for bone level measurements. Crestal bone loss was measured by DSR (Digital Subtraction Radiograph). Prosthetic Protocol: Three months after the surgical procedure, the patient received a abutment and prosthetic restoration. Transfer copings were inserted into the internal hexes of the implant with a seating instrument and secured with abutment screw. An impression was made with a polyether material using an individual impression tray. The temporary crown was cemented and maintained in full contact in centric occlusion. The patient followed a soft diet (avoiding bread and meat) for 3months.Placement of the Definitive Prosthesis-Six months after implant placement, the temporary crowns was removed. Definitive metal ceramic restoration were than cemented onto the definitive abutment after 12 months from the baseline. RESULTS Table 1: Intergroup comparison of mean isq value of implant stability at baseline, 1 month, 3 month and 12 months.
Mann-whitney U test # Non-significant difference
Table 2:
Mann-whitney U test * Significant difference
Table 3: Intergroup comparison of mean values of mesial bone loss
Mann-whitney U test * Significant difference
Table 4: Intergrop comparision of mean value of distal bone loss
Mann-whitney U test, * Significant difference
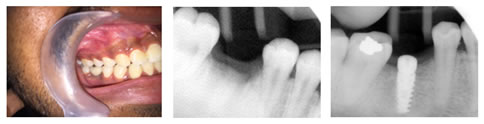
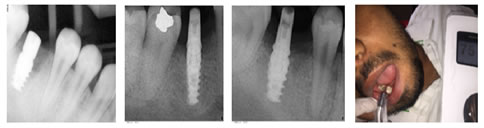
Figure 1: Figure 1a: Figure 2a: Figure 2b: Figure 3a: Figure 3b:
Figure 4a: Figure 4b: Figure 5:
Figure 6: Figure 7: Figure 8: Figure 8b: Figure 9: Figure 10: Figure 11:
Legend Figure 1a: Intraoral view of pre-operative molar site; Figure 2b: Flapped implant placement technique; Figure 3c: Healinf Abutment Figure 4d: Abutment; Figure 5e: Temporary Crown at 3 months; Figure 6f: Permanent crown at 12 months; Figure 7g: Radiograph of preoperative site; Figure 8h: Radiograph of implant immediately after implant placement; Figure 9i: Radiograph of implant 3months after implant placement; Figure 10j: Radiograph of implant 12 months after implant placement; Figure 11k: Clinical measurement of Implant Stability using RFAResonance Frequency Analysis
The statistical analysis were performed using SPSS (Statistical Package for Social Sciences) version 21.0 and Epi- info version 3.0. Statistical significance was considered for p0.05. The mean ISQ value in the Flapless group was observed to be 63.007.071, 64.001.414, 72.503.56 and 79.500.707 at the time of insertion, 3 weeks, 3 months and 12 months respectively.(Table-1). The mean ISQ value in the Flap group was observed to be 67.002.828, 56.506.364, 65.0014.142 and 79.504.950 at the time of insertion, 3weeks, 3 months and 12 months respectively. (Table2). The comparison of mean RFA was compared between FLAPLESS implant placement technique and FLAP implant placement technique at 0 month, 3 weeks, 3 months and 12 months using the (Mann Whitney U test). There was no significant difference in mean RFA at 0 month, 1 month, 3 months and 12 months. The comparison of mean difference in RFA from 0-3 months, 3-12 months and 0-12 months was done between FLAPLESS implant placement technique and FLAP implant placement technique using the (Mann Whitney U test). There was no significant difference in mean difference in RFA from 0-12 months between FLAPLESS implant placement technique and FLAP implant placement technique. The mean difference in RFA from 0-3 months was significantly more among Flapless implant placement technique and mean difference in RFA from 3-12 months was significantly more among Flap implant placement technique. The mean mesial and distal bone loss around Flapless group during the healing phase i.e (0 to 3 months) was measured to be 0.000.00 and 0.100.14 following the prosthetic loading (3months to 12 months) the loss was 0.500.707mm and 0.500.70mm and 0.500.707mm and 0.600.849mm respectively from the time of insertion till the end of study i.e. (0 to 12 months).(Table-4). The mean mesial and distal bone loss around Flap group during the healing phase i.e (0 to 3 months) was measured to be 0.650.77 and 0.400.56, following the prosthetic loading (3months to 12 months) the loss was 0.200.14mm and 0.250.35mm with a overall loss of 0.850.63mm and 0.650.91mm respectively from the time of insertion till the end of study i.e. (0 to 12 months). (Table-4). There was no significant difference in mean difference in DISTAL BONE LOSS from 0-12 months between FLAPLESS implant placement technique and FLAP implant placement technique. The mean difference in DISTAL BONE LOSS from 0-3 months was significantly more among Flap implant placement technique and mean difference in DISTAL BONE LOSS from 3-12 months was significantly more among Flapless implant placement technique. There was no significant difference in mean difference in MESIAL BONE LOSS from 0-12 months between FLAPLESS implant placement technique and FLAP implant placement technique. The mean difference in MESIAL BONE LOSS from 0-3 months and 0-12 months was significantly more among Flap implant placement technique.
DISCUSSION The goal of the present study was to compare the placement of flapped vs. flapless dental implants utilizing in addition to custom clinical and radiograph outcomes. The results demonstrated that flapless implant placement yielded improved clinical (Implant stability) and radiographic outcomes compared with flapped implantation. Successful osseointegration is dependent on the implant stability which is achieved into two different stages: Primary and Secondary.3 The primary implant stability is measured at the time of implant placement and depends upon the amount of bone to implant contact area, apart from other factors. A decrease in RFA ISQ value (primary stability) was observed at 3 weeks which can be the result of the dynamic nature of bone healing round the implant. It has been suggested by Robert WE that this decrease can be attributed to callus formation and lamellar compaction within the woven bone with resultant reduction in primary contact.4 These results are in accordance with the study done by Barewal RM et al (2003)3 where they found the lowest ISQ at 3 weeks after implant placement. A flapless procedure could have a positive effect on the early bone remodelling process, because during the surgical procedure, the bone remains covered by the periosteum. It can be assumed that raising a muco- periosteal flap and having the bone denuded during a certain time causes a postsurgical reaction and may have an impact on the bone remodeling around the implant5. Preservation of the crestal bone surrounding the osseointegrated implant is of at most importance in determining the long term implant survival and is the integrated part of the evaluation of implant patient and recall visits. The blood clot acts as a physical matrix that induces and amplifies the migration, proliferation, and differentiation of various types of cells, subsequently leading to fibroplasia and angiogenesis. In this context, it must be pointed out that both stabilization of the blood clot and early angiogenesis were considered to be important factors strongly influencing wound healing. Experimental studies in animals have indicated that formation of blood capillaries precedes the formation of new bone because osteogenic cells were observed to arise from pericytes adjacent to the connective tissue of small blood vessels. Neovascularization of the blood clot and subsequently new bone formation appeared to start from open bone marrow spaces of the adjacent defect borders6. With flapless procedure, blood clot fills the intrabony defect and provides a seal between the gingival flap and the implant surface. Plasma proteins, primarily fibrinogen, imposed onto the internal aspect of the gingival surface and the implant surface provide the initial basis for an adherence of stable fibrin clot. The uninterruptedmaturation of the fibrin clot is essential for the formation of a new connective attachment rather than the junctional epithelium, because intact fibrin clot blocks apical migration of the epithelium. Flapless surgery allows minimum disruption of periimplant tissues, thereby reducing changes in crestal.6 bone levels, probing depth, and inflammation. In addition, flapless surgery has also been reported to preserve circulation of the peri-implant tissues and accelerate recuperation, thereby allowing the patientto resume regular oral hygiene maintenance immediately after implant placement. Periimplantitis bone loss is a crucial parameter affecting implant success (Hermann et al 1997)7. Many studies have investigated the factors that potentially increase bone to implant contact and decrease bone resorption, mainly focusing on implant design or treatment of the implant surface. However, an aften underestimated factors affecting bone loss around implants is flap design. In a canine model, You et al (2009)8similarly reported mean bone resorption of 0.2 +- 0.3mm in the flapped group 3 months after implant placement and no bone loss in the flapless group. Similar resorption patterns were reported by Job et al (2008)9 more specifically, the radiograph evaluation 3 months after implant placement indicated 0.4mm bone loss in the flapped group and 0.06mm in the flapless group. Based on the findings of the present clinical study and the existing relevant literature, bone loss is apparently minimal or even non-existent around flapless implants during 3-months after implant placement. Other studies on flapless implants with longer follow up periods indicate that there is no significant additional bone loss after implant loading (Becker et al 2009, Jeong et al 2011)10. In addition, both flapped and flapless implants seem to respond similarly after loading (De Bruyn et al 2011)11. A flapless procedure could have a effect on the early bone remodelling process because during the surgical procedure, the bone covered by a periosteum. This could be assumed that raising a muco-periosteal flap and having the bone denuded during a certain time causes a postsurgical reaction and may have an impact on the bone remodelling around the implant. The reaction of the periimplantitis tissue to a flapless implants placement was recently investigated histomorphometrically in female mongrel dogs. One author reported of enhanced osseointegration of the flapless implants (70% BIC ) compared with the implants inserted with a flap (60% BIC ) and bone height of 10mm versus 9mm.12 Another author suggested that a flapless procedure increase vascularity of the periimplantitis mucosa, which furthermore appeared to be free from signs of inflammation. A histological analysis of the mucosa of flapless implants revealed that the junctional epithelium was located 1 mm less apically and reduced crestal bone resorption around the implants was observed13.
CONCLUSION In the present study an adverse effect of the flapless technique for implant placement was not observed in selected patients. Implant stability was observed in slight favour of the flapless method and crestal bone loss was less in flaplessimplant placement technique.
REFERENCES
|
 Home
Home