Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 - April 2019
Vidisha S Barua1, Pradnya Kulkarni2*
1Resident, 2Associate Professor, Department of Anaesthesiology, Department of Anaesthesiology, MGM Medical College and Hospital, N6 CIDCO, Aurangabad, Maharashtra, INDIA. Email: vidishabarua9@gmail.com
Abstract Background: Vocal fold paralysis refers to reduced or absent function of the vagus nerve or its distal branch, the recurrent laryngeal nerve. Kashima’s procedure is a lateralization procedure of the vocal cords performed for cordotomy using laser introduced by Kashima in 1989. Case Report: 50 y/o female - o/c/o Rt hemithyroidectomy with dyspnea (NYHA 2). Lt vocal cord palsy, Rt cocal cord sluggishly mobile. RS - Inspiratory stridor +Preoperatively, the patient in sitting position pharynx was anaesthetised with10./. Lignocaine spray and 2ml of 4./. Lignocaine nebulisation. Patient was induced with Inj.Propofol 50mg (+30mg+20mg+20mg) (in titrated doses) and Inj.Atracurium 25mg iv. Patient was intubated orally using a cuffed microlaryngeal tube number 5. Intraoperatively, patient was vitally stable. Analgesia was provided in the form of top ups of Inj.Fentanyl 20ug iv. Reversal given post -op and pt. extubated smoothly. Discussion: A microlaryngeal tube was used to secure the airway and patient was ventilated using a closed-circuit ventilator system. The advantage being smooth maintenance of airway throughout surgery and ability to provide oxygen at low concentrations. Anaesthesia was maintained using oxygen-air mixture with isoflurane (non-inflammable agent). Key Word: Kashima's Procedure.
INTRODUCTION Vocal fold paralysis refers to reduced or absent function of the vagus nerve or its distal branch, the recurrent laryngeal nerve.5The incidence of bilateral vocal fold paralysis is about 1/3rd of all vocal fold paralysis cases.5 The incidence of vocal cord paralysis is 42/10000 patients seen.4 Bilateral paralysis accounts for 25./. of cases of recurrent nerve paralysis.6 Classical representation of patients with bilateral vocal fold paralysis is reduction of the glottal area, leading to varying degrees of airway obstruction/stridor and can lead to respiratory distress and dyspnoea, with minimal voice change. 5,6Most common cause of this condition is iatrogenic, especially after thyroidectomy.6Kashima’s procedure is a lateralization procedure of the vocal cords performed for cordotomy using laser introduced by Kashima in 1989.1Anaesthesia for laser surgery of the airway comes with a variety of challenges and drawbacks. It is challenging as the airway is not only shared with the surgeon, but is also being operated upon.2 Keeping in mind the various complications, this high-risk case was successfully managed without any airway fires, the need of jet ventilation or tracheostomy.
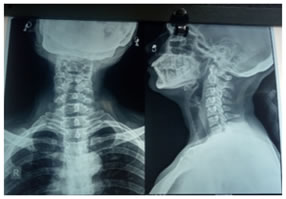
CASE REPORT A 50 YO female (60 kg) presented with complaints of breathlessness on exertion and hoarseness of voice for 6 months. She was an op/c/o Right hemithyroidectomy and Left subtotal thyroidectomy, in March 2018 and was diagnosed to have bilateral vocal cord palsy post operatively. Her breathlessness and respiratory discomfort would worsen on lying down. As per NYHA dyspnoea grading, she was grade 2. She was taking Tab.Thyronorm 100ug after surgery since 3 months. 70-degree scopy-Bilateral vocal cords in paramedian position. No pooling of secretions. Base of tongue, vallecula, epiglottis normal.AE folds, pyriform fossa clear. Indirect Laryngoscopy-Left vocal cord palsy. Rightvocal cord sluggishly mobile.Bilateral vocal cord median to paramedian position. Blood Investigations–Hb 13.8 Creatinine 0.7 FT3- 3.42 FT4-1.70 TSH-1.08 Serum calcium- 8.9 ECG- Within normal limits 2D ECHO- EF- 55-60. Normal sized cardiac chambers, good LV systolic function, no RMWA. CXR(PA)-NO ABNORMALITY DETECTEDX RAY NECK- AP/LATERAL-TRACHEAL NARROWING SEEN. PFT-severe obstruction with good post bronchodilator reversibility.
Patient was conscious, oriented and afebrile. PULSE RATE- 80/MINBLOOD PRESSURE- 122/86 MMHG SPO2- 99./ RESPIRATORY RATE-18/MIN CVS- S1S2 heard, no murmur RS- AEEBS, inspiratory stridor present. Patient was accepted for anaesthesia under ASA GRADE 3 HIGH RISK.PULSE RATE- 100/MIN BLOOD PRESSURE-136/90MMHG SPO2-99./. RESPIRATORY RATE-24/MIN Preoperatively, the patient in sitting position pharynx was anaesthetised with10./. Lignocaine spray and 2ml of 4./. Lignocaine nebulisation. Check Direct laryngoscopy was done before IV induction. Patient was premedicatedwithInj.glycopyrrolate 0.2mg and Inj.Fentanyl 60ug iv. Patient was induced with Inj. Propofol 50mg (+30mg+20mg+20mg) (in titrated doses) and Inj.Atracurium 25mg iv. Patient was intubated orally using a cuffed microlaryngeal tube number 5. Anaesthesia was maintained using oxygen and air (50:50) and Isoflurane (MAC 1-1.5./) Intraoperatively, patient was vitally stable. Analgesia was provided in the form of top ups of Inj. Fentanyl 20ug iv.
The procedure was completed within one hour. Patient was reversed with Inj. Glycopyrrolate 0.01mg/kg and Inj. Neostigmine 0.05mg/kg and extubated smoothly. Patient was shifted to recovery room and monitored. Inspiratory stridor decreased post operatively. Nebulisation 8 hourly Inj. Dexamethasone 8 hourly was advised
DISCUSSION Kashima’s procedure is a lateralization procedure of the vocal cords performed for cordotomy using laser introduced by Kashima in 1989.1Various anaesthesia techniques include no tube with spontaneous/controlled ventilation, jet ventilating the patient, protecting external surface of conventional tube, using non-combustible tubes to prevent fire hazards in the airway and lastly, tracheostomizing the patient.2 This patient had presented with complaints of breathlessness, respiratory discomfort and change in voice. Holmium Laser was used for this laryngeal laser surgery. Energy used was 0.8 Joules at rate 10 Pulses/sec (Hz) with Power 8 Watts. A microlaryngeal tube was used to secure the airway and patient was ventilated using a closed-circuit ventilator system. The advantage being smooth maintenance of airway throughout surgery and ability to provide oxygen at low concentrations. Anaesthesia was maintained using oxygen-air mixture with isoflurane (non-inflammable agent). The tube was not wrapped with silver foil as this would increase the diameter of the tube and reduce operative space. No tube with spontaneous/controlled ventilation technique was not applied because of the chances of inadequate maintenance of depth of anaesthesia, laryngospasm, hypoventilation/apnoea and mobility of vocal cords.2These possibilities were higher in this case as the patient had difficulty in breathing, stridor and severe obstruction as per PFT’s. Jet ventilation technique was also not applied given the complications associated with it, which are pneumothorax, barotrauma, abdominal distention, dehydration of mucosal surface, aspiration of resected material.2 Airway fires and explosions were prevented by keeping Fio2 low and avoiding use of N2O. Tracheostomy was not done for this patient as mask ventilation was adequate and intubation was possible.
REFERENCES
|
|
 Home
Home