Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 - April 2019
Manisha M Jadhav1, Sudhir V Bhise2*, P M Hippargekar3, Shankar Kothule4
1Resident,2Associate Professor, 3Professor and Head, Department of ENT, SRTR Government Medical College, Ambajogai, Maharashtra. Email: jadhavm779@gmail.com, bhisesudhir13@gmail.com, pmhippargekar@yahoo.com, kothule1986@gmail.com
Abstract The use of rigid endoscope in the management of dry central perforation of the drum represented a significant advance in middle ear surgery. The present study was undertaken to asses and evaluate the feasibility, advantages, disadvantages of endoscopic transcanal myringoplasty in tubotympanic type of chronic suppurative otitis media. Present study was conducted on 50 cases attending ENT opd having tubotympanic type of chronic suppurative otitis media with dry central perforation of small, moderate or large size. Majority cases are from the age group of 16 to 50 years. Postoperatively at the end of 6th month, graft acceptance was seen 84 % patients. All sizes of perforation were healed equally well within significant differences. Postoperative hearing improvement was seen 80% patients having air bone gap less than 20db, 76%patients having air bone gap less than 10 db. The endoscopic approach of transcanal myringoplasty is less invasive, time taken for surgery is less, duration of hospitalization is less and has excellent cosmetic result. Key Word: transcanal, myringoplasty.
INTRODUCTION Myringoplasty is the repair of a perforation of the tympanic membrane when middle ear space, its mucosa and the ossicular chain are free of disease. Since modern tympanoplastic procedures were described by Wullstein and Zollner in the 1950. The present study was undertaken to asses and evaluate the endoscopic transcanal myringoplasty in csom patients in terms of feasibility, advantages, disadvantages and complications following the procedure.
AIMS ANDOBJECTIVES To study the feasibility, advantages and result of endoscopic transcanal myringoplasty.
MATERIALS AND METHODS Source of Data: Adult patients attending ENT OPD in rural tertiary care center, who were medically fit and selected in this study from the period June 2015- June 2017. Type of Study: Prospective Study. Sample Size: Total 50 cases were included the cases were randomly selected using a periodic random number method to avoid bias in the selection of cases. Inclusion Criteria: Adult patients who were medically fit for surgery included in the study, all the patients of safe/tubotympanic type csom having dry central perforation of tympanic membrane with intact and mobile ossicular chain. Patients had deafness attributable to perforation of tympanic membrane and patients who have given written and informed consent. Exclusion Criteria: Patients with marginal and attic perforation, cholesteatoma, granulation or flakes, wet central perforation, patients undergoing revision myringoplasty, ossicular chain discontinuity, patients not willing for the surgery. Method of Collection of Data: Patients attending ENT OPD with central dry perforation of tympanic menbrane were selected for endoscopic transcanal myringoplasty using a random number method. Written and Informed consent were taken from all the patients. for all patients tuning fork tests was done with 256 hz, 512 hz and 1024 hz tuning forks. Pre-operative pure tone audiometry done by the audiologist for all patients and recorded. During surgery, various parameters were noted including duration of surgery and hospitalization. These patients were followed through a period of 6 months and assessed using pure tone audiometry. After selection of patient tympanic membrane status was assessed, patient was admitted a day before surgery and a detail history was recorded and the clinical evaluation of ear, nose and throat was done. Written consent taken. Puretone Audiometry, X-ray mastoid and routine blood investigation done. Surgical Technique –Supine position given to patient with head tilted 120 degree to opposite site of operating ear, cleaning, painting and draping done. Inj. 2% xylocain with 1:30,000 Adrenaline infiltrated post aurally, over tragus and in each at 12, 3, 6 and 9 o’clock position. Procedure started with permeatal or transcanal approach. Tragal or temporalis fascia graft harvested. Freshening of margins of perforation done. Incision taken over posterior canal wall in 12 and 6 o’ clock position and tympanomeatal flap elevated. Placement of graft under freshened margin of perforation around 360 degree done and tympanomeatal flap reposited. Gelfoam pieces kept for support, skin incision sutured with -0 silk and small dressing given. Patient discharge the following day. average operating time was between 80-120 mins. Follow up taken at the end of 1 st week then 1st 3rd and 6th month and postoperative audiometry done after 3rd and 6th month. The patients were studied for the following parameters-visualization of tympanic membrane and middle ear structures, operability of endoscopic approach, graft acceptance at 6 month – healed tympanic membrane, graft failure, postoperative hearing assessment at 6 month. Post-operative air bone gap was considered as the objective method to asses the improvement in hearing threshold, time taken for surgery, duration of hospitalization, cosmetic results at 6 month. Postoperative complications were looked for and treated.
RESULTS AND OBSERVATIONS Out of 50 patients 30 (i.e. 60%) patients were in the age group of 16-29 years. Out of 50 patients 23 are males (ie.46%) patients and 27 are females (i.e. 54%). Female: male ratio is 1.17:1.mean-28.1, mode-28, median-28. 12(24%) patients required < 80 minutes for surgery, 28 (56%) patients required time between 80-100minutes and 20 (40%) pts required > 100 minutes for surgery duration of hospitalization, Out of 50 patients, 40 patients (ie.80%) was admitted in hospital for 2 days, 6 patients (12%) for 3 days, and 4 patients (8%) for 4 days. Average 2-3 days. Subjective cosmetic result-at the end of six month, all 50(100%) patients in the study group rated their cosmetic result are excellent. Objective analysis of cosmetic result was done by us at the end of six month and revealed that none of the patient had visible scar.
Table 1: Duration Of Surgery
Table 2: Duration Of Hospitalization
Table 3: Percentage of Graft Uptake with Size of Perforation
In present study small perforations showed very good healing tendency (95.65%), moderate perforation showed healing tendency 77.77% where less healing tendency (66. %) was observed in large perforation. Cases with successful healing after six months of follow up, out of 23 male patients 19 (82%) patients have healed tympanic membrane; out of 27 female patients 23(85.18%) have healed tympanic membrane.
Table 4: Total no. of Cases with Successful Healing
Out of 50 patients, 42 (84%) have healed tympanic membrane after six month of follow up, out of 23 male patients 19 (82%) patients have healed tympanic membrane out of 27 female patients 23(85.18%) have healed tympanic membrane.Healing of perforation in relation of disease in contra lateral ear, out of 8 patients who has b/l disease, only 5 patients (62.5%) showed good graft uptake, where as in unilateral disease the percentage of graft uptake was 88.09%.
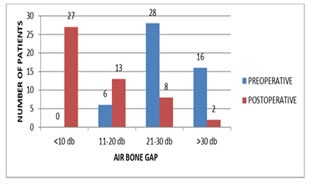
Figure1: comparison between pre and postoperative air bone gap in db Graph shows comparison between pre and postoperative Air-Bone gap in dB. Preoperatively out of 50 none of patients has air bone gap less than 10dB ,6 patients has Air – Bone gap between 11-20 db .28 patients has Air Bone gap between 21-30 db and 16 patients has Air-Bone gap more than 30db. Postoperatively out of 50 patients 27 patient has Air-Bone gap < 10 db, 13 patients has Air-Bone gap between 11-20 db , 8 patients has Air-Bone gap between 21-30 dB and 2 patient has Air Bone gap > 30 dB . 40 patients (80%) has Air-Bone gap less than 20 db and 27 patients (54 %) has Air-Bone gap less than 10 db Table shows air-bone gap distribution in postoperative intact tympanic membrane 27( 54%) patients has air- bone gap less than 10db, 13 patients ( 26%) has air-bone gap between 11-20 db. , 2 patients ( i.e. 4 %) has air – bone gap between 21-30 db. and none patient has air- bone gap more than 30 db
POSTOPERATIVE RESULTS a) Graft Uptake: in this study out of 50 patient 42(84%) has very good graft uptake at end of 6 months out of 23 males and 27 females, 19 (82.64%) and 23 (85%) respectively has successful graft uptake. b) Hearing Improvement: pure tone audiometry was used to assess average air bone gap preoperatively and postoperatively in all cases. preoperatively none of the patient has air bone gap below 10db but postoperatively at 6th month27 patient having improved a-b gap less than 10 db and 13 patient has a-b gap in the range of 11-20db. preoperatively 28 patients had air bone gap in the range of 21-30 db, whereas this range levels was found in 8 cases and 2 cases has found –a-b gap more than 30 db postoperatively. at the end of 6tn month 40 patients (84%) had a-b gap less than 20 db 27 patients (64.28%) having a-b gap less than 10 db and 8 patients (16%) still having a-b gap between 21-30 db. Mean improvement comes out to be 13.64, standard deviation was calculated to be 7.35 and its p value came out to be less than 0.0001 using paired t test. Its significantDISCUSSION In present study patients were in the age group 16-50 years, 46% (23) were males and54% (27) were female. Similar age group 19-50 years was selected in a study by Yadav et al. in this age group there is less chance of upper respiratory tract infections and presbycusis.in present study the operative time among the 50 ears was 60- 120 minutes. In a study by Ghaffer et al he mean operative time was 62.85 minutes among 34 patients who underwent endoscopic tympanoplasty. in a study by Huang et al the mean operative time of endoscopic approach was 50.4 min. in our institution endoscopic transcanal myringoplasty procedure was started first time and these 50 patients are first 50candidate of this procedure. A higher level of experience can shorten the duration of time. In present study duration of hospital stay was 2 days for 40(80%) patients, 3 days for6(12%) patients, 4daysfor 4 (8%) patients, average is 2.3 days. In the study by Harugop et al subjects who underwent endoscopic surgery took an average of 2.4days to return to daily routine while this was 5.4 days in subjects who underwent conventional surgery. All 50 (100%) patients in the study group rated their cosmetic result as excellent. similar cosmetic result after endoscopic transcanal myringoplasty. in study of harugop et al. Results of surgery in myringoplasty are usually expressed in terms of graft take - up rate and hearing improvement. graft status in present study out of 50 patients, 42 (84%) patients had a successfully repaired tympanic membrane. Males had a success rate of 82.60% whereas in females it was 85.18%. The sex thus does not seem to significantly affect the rate of healing. The take up rates were less than those described by EI Guiny and Raj and Meher but better than those reported by Kurhuketo and Usami.
Graft Uptake
Bilateral perforation had low success rate in view of graft up take, similar observation made in study of Adkins and White. Hearing Assessment
In present study, 11 patient’s external auditory canal were narrow or/ protruded. During examination and surgery even though narrow or/protruded external auditory canal, endoscope was easily introduce in ear canal without difficulty and endoscopic view shows the entire image of tympanic membrane in one field and clear visualization of the margins of perforation. Endoscopes facilitated reliable refreshing of the perforation edges and grafting procedures. The tympanic cavity could also be observed through the perforation in the endoscopic wide view. Fine structures were also visible through large perforations such as the incudostapedial joint, orifice of the tube, round-window niche, ossicular chain, and tympanic isthmus. Endoscopy revealed no pathology of the tympanic cavity in this study. The endoscope’s wide field of view allows observation of the entire circumference of the perforation and approaching the edge of the perforation reveals the under surface of the tympanic membrane. Harugop et al reported that the tympanic annulus was not completely visualized with a microscope in 20% of patients and these patients required canaloplasty. Similar observation done by Takatoshi Fukurawa et al the wide angle of zero-degree endoscope visualizes the entire tympanic membrane in one frame. There is no need to frequent adjust the patients head or do canaloplasty there by saving operative time. Similar observations were made in two separate studies by Tarabhachi M and Usami set al similar observation by Raj, Meher et al. When exploring the middle ear the endoscope approach provide more information regarding the orifice of the tube, the incudostapedial joint, and the round window niche. The endoscopic approach is less invasive (no skin incision and canaloplasty are required). Using a thin, rigid endoscope, a surgeon can perform minimally invasive procedure with protection of the anatomy, which allows functional reconstruction during surgery. So reduce postoperative bleeding and pain and achieve superior cosmetic result. Iin addition, minimal damage of healthy structure is likely to minimize postoperative adverse reaction locally and generally. With increasing use of minimally invasive surgery, Kurhuke to et al. point out that using an endoscopic approach could fulfill the goal of causing the least amount of trauma to normal tissues. In addition to the abovementioned quantitative aspects related to the surgical outcome, endoscopic myringoplasty offers some practical advantages to the surgeon. The mobility of the endoscopic camera is much better than a microscope with its fixed heavy stand. It gives a continuous movie camera type of picture by moving easily to the site of interest in contrast to static vision of the microscope. The angled scopes help in increasing the visibility and accessibility to difficult areas like canal wall, anterior recess, anterior perforation and eustachian tube and the ossicular chain. This is helpful while shifting from one area to the other like in elevation of flap. There is no need of repeated adjustments like in the microscope with the endoscope. Vision beyond the shaft of the instruments is possible so instruments do not interfere with the vision like in the microscope. The magnification is very high through the T.V. monitor. Physical posture of the surgeon is also better because of the monitor. Communication between the surgeon and assistants, peers and students are also better as everyone sees the same image. Recording is possible which is useful for medico-legal and teaching purposes. Advantages of endoscopic transcanal myringoplasty ease of operation, wide angle view of operative field, easy to get close up view of middle ear spaces, good surgical outcome. Excellent cosmetic results. Good hearing improvement, duration of hospitalization is less, post-operative complications are less, ease of documentation. In present study, there was no immediate surgical complication, One female patients developed middle ear and tympanic membrane inflammation fifteen days after the surgery, which subsequently had recurrence of discharge from the middle ear and the graft failed to take up. Out of 50, one patients had late post operative complication (i.e.2%) of tm inflammation. No immediate postoperative complication and less late postoperative complication. Despite the benefits, there are still several disadvantages to the endoscopic approach that need to be over-come. The endoscope lacks sufficient magnification and focus, also this approach requires the surgeon to perform with one hand, holding the endoscope in one hand and other instruments or suction in other hand. In the endoscopic approach, instruments crowd the ear canal, and at the time of excessive bleeding it become extremely difficult to operate as only one hand is free. More over blood soils the tip of microscope which obscures the surgical field. Thus tip of endoscope has to be cleaned frequently. Similar observation was made in studies of Tarabich and Karhunketo TS, Ilomaki JH, Puhakka HJ, Yadav et al. Potheir DD was made observation in study that meticulous haemostasis is essential as a drop of blood can obscure the field. So while performing endoscopic myringoplasty meticulous haemostasis is must for doing smooth surgeries. By developing stand for endoscope, which can fix the scope in desired position so both hands are free to operate. Endoscopic surgery offers 2D images and 2D images lack the depth perception, thus lifting the graft to make contact with the edge of the perforation will difficult. So one has to be extra careful, while close to vital structures and positioning of the graft. Similar observation made by Mohindra S et al. Other criticisms of endoscope use in otologic surgery refer to the delicate nature of surrounding structures, with potential risk of mechanical and thermal trauma. This difficulty may be overcome by experience. Savlon is used as a defogging agent for endoscope, studies on effect of savlon on middle ear mucosa and inner ear are not sufficient, thus safety of savlon is yet to be established. However, improvement in full high definition camera system can provide much more delicate endoscopic views with better contrast to minimize these problems. CONCLUSION Results were evaluated in terms of hearing improvement, graft uptake, duration of surgery, duration of hospitalization, cosmetic results and post-operative recovery. Postoperatively at the end of 6th month, 42(84 %) patients has showed good graft uptake. all sizes of perforation were healed equally well with insignificant differences. Postoperative audiometry revealed 40(80%) patients with air bone gap less than 20db. less than 10dB air bone gap was seen in 27(54%) patients. 16% patients had graft uptake failure. No immediate post-operative complications seen. We were able to achieve good access to and visualize whole tympanic membrane, margins of perforations, least accessible nook and corners of middle ear cavity like sinus tympani, facial recess etc. with the endoscope even in narrow canals and overhangs. The endoscopic approach was less invasive and achieved best cosmetic results. In addition to minimal damage to healthy structure, it minimized post-operative adverse reactions locally and generally. Loss of depth perception, one handed technique, crowding of instruments in the ear canal and frequent contamination of tip of the endoscope with blood were the limitations of the endoscope that can be easily overcome with haemostasis and practice. According to present study endoscopic approach is less invasive and has best cosmetic results, minimal damage to healthy structures so minimize post-opeartive complications. It has good access to visualize middle ear spaces or structures, safe and feasible procedure, with good success rate for tympanic membrane perforation closure and recovery of hearing thresholds.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home