Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 3 - June 2019
Relation of nasopharyngeal lymphoid tissue size and bacteriology in treatment of adult chronic rhinosinusitis without polyposis patients in a tertiary care hospital in south India
Rajarajeswari Nalamate*, Tambi Abraham Cherian**, Mary Kurien***, Meenu Khurana Cherian****
*Assistant Professor, ***Professor and Head, Department of ENT, Pondicherry Institute of Medical Sciences, Puducherry, INDIA. **, ****ENT Specialist, Thumbay Hospital, Ajman, UAE. Email: rajisampathporal@gmail.com
Abstract Background: Nasopharyngeal lymphoid hypertrophy (adenoids), a disease of children, is often overlooked and underestimated by underlying sinus and nasal pathology in adults with chronic rhinosinusitis. Objective: To document adenoid size and bacterial etiology in adults with chronic sinutis without polyps and to note the effect of medical treatment on adenoid size in these patients. Materials and Methods: Prospective study of patients over 18 years of age with chronic rhinosinusitis without polyps. Detailed endoscopic evaluation, including measurement of adenoid size, middle meatal culture and sensitivity and post medical therapy adenoid size measurements were documented. Results: There were 53 patients in this study, majority (60.4%) being males. Aerobic culture was positive in 45.2%, coagulase negative Staphylococcus being most common (26%). Nasopharyngeal lymphoid tissue was significantly enlarged in 56.6%. Univariate ANOVA test revealed it’s size in culture positive case was statistically significantly larger than those with cultures negative. Paired t test noted statistically significant reduction in post-treatment size in these patients. These clinically relevant issues have not been previously reported. Conclusion: Nasopharyngeal lymphoid hyperplasia is an indicator of infective aetiology in chronic rhinosinusitis without polyps. Endoscopic middle meatal, culture and sensitivity, an underrated investigation, plays a vital role for culture specific medical treatment in these patients. It is to be considered a mandatory pre-requisite for medical treatment is these patients, failing which surgical therapy can be planned. Key Word: nasopharyngeal lymphoid tissue.
INTRODUCTION Rhinosinusitis is a heterogeneous group of diseases affecting 5 to 15% of people, characterized by inflammation of the nasal and paranasal sinus mucosa and may include nasal congestion or discharge, facial pain or pressure, loss of the sense of smell, polyposis, mucopurulent discharge, and edema or obstruction of the sinuses and nasal cavity.1 While acute rhinosinusitis (ARS) and subacute rhinosinusitis involve the resolution of symptoms within 4 and 12 weeks, respectively, progression to chronic rhinosinusitis (CRS), characterized by symptoms persisting for longer than 12 weeks, occurs in up to 5% of the general population.2 Persistence of infection may be due to poor ventilation of sinuses, altered mucociliary mechanism, infection by virulent microorganisms and, or inadequate treatment. CRS is a debilitating condition, with effects on quality of life being equal to or greater than those with chronic bronchitis, asthma, peptic ulcer disease, chronic obstructive pulmonary disease, congestive heart failure, and angina.3 In addition to the physical burden on the individual, the annual economic burden of CRS is enormous (estimated to be $8.6 billion in health care costs in the United States)4,5. The upper respiratory tract, including the nasopharynx, is colonized by normal bacterial flora that includes potential pathogens capable of causing respiratory tract infections, including sinusitis. These potential pathogens can spread from the nasopharynx into the sinus cavity during respiratory infection and cause sinus infection.6 Although the exact etiology of the inflammation associated with CRS is uncertain, the presence of bacteria within the sinuses has been well documented. It is plausible that, in chronic sinusitis, mucociliary clearance and host defenses are impaired to the point that the sinus cavity loses its normal sterility and becomes colonized with nasal flora. Thus, chronic sinusitis may not truly be an infectious process but an aberration of the normal anatomy responsible for drainage and damage to the mucosa of the sinus cavity. Most clinicians believe that microorganisms play a major role in the etiology and pathogenesis of most cases of CRS and prescribe antimicrobial therapy.7 It has also been found that the most common bacterial isolates from adult patients with community-acquired chronic bacterial sinusitis are Staphylococcus aureus, Staphylococcus epidermidis and anaerobic gram negative organisms.8 Bacterial diversity and composition serve as predictors of the surgical outcome of CRS.9 The nasopharyngeal lymphoid tissue forms part of the Mucosa Associated Lymphoid Tissue (MALT). They are predominantly B cell organs. Immunoglobulins, mainly Ig G are produced in response to antigens like bacteria, viruses, fungi, air pollutants and allergens. The size of the nasopharyngeal lymphoid tissue varies with age, fully developed during seventh month of gestation, continue to grow till fifth year of life and regress after puberty. Acute upper respiratory infections result in hyperplasia with enlargement and multiplication of lymphoid follicle. Chronic rhinosinusitis can lead to persistent inflammation of the adenoids as the mucus drainage from sinuses sweep over the nasopharyngeal walls. This study has been conducted with an objective to find out relationship between adenoid volume, bacteriology and the treatment of adult chronic rhinosinusitis. MATERIALS AND METHODS Fifty three adult patients aged above 18 years with symptoms of sinusitis- at least 2 major factors (facial pain/ pressure, facial congestion, nasal obstruction, nasal discharge/postnasal drip, hyposmia/anosmia, purulent nasal secretions) or 1 major and 2 or more minor factors (headache, fever, halitosis, fatigue, cough, ear pain/pressure) for more than 12 weeks duration who visited our ENT department in Pondicherry Institute of Medical Sciences, Pondicherry over a duration of one year were included in the study. Patients with allergic rhinitis, tumours of nose, paranasal sinuses and nasopharynx were excluded. After obtaining Institutional Ethics Committee approval and Informed consent from the study participants, topical anaesthesia to nose and nasopharynx using nasal packed soaked with 4% lignocaine and 0.05% ephedrine nasal drops for 10 minutes were given. Diagnostic nasal endoscopy was performed and smear from the middle meatus was taken for aerobic culture and sensitivity to obtain the bacterial aetiology of CRS in individual patients. Endoscopic assessment of the size of the nasopharyngeal lymphoid tissue was made using 4mm 0 degree endoscope. The scope was passed along the floor of the nose to the posterior wall of nasopharynx and a marking was made over the scope at the level of the outer surface of the columella when the posterior wall was gently touched. Then the scope was withdrawn, the nasopharyngeal lymphoid tissue visualised, the tip of the scope was advanced to touch the anterior surface of the lymphoid tissue, and again a marking was made over the scope at the level of outer surface of the columella. The distance between the two markings was taken as the size of nasopharyngeal lymphoid tissue. Following treatment, size of the nasopharyngeal lymphoid tissue was measured after 3 months and reassessed. Paired t test was applied to detect any significant difference between pre-treatment and post-treatment nasopharyngeal lymphoid tissue sizes. 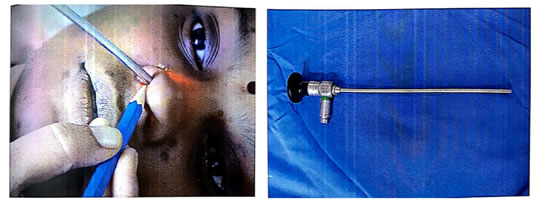
Figure 1: Measurment of Adenoid size using nasal endoscope; Figure 2: Markings on the Nasal Endoscope RESULTS Baseline characteristics of the study participants is represented in table 1 which shows that majority of the patients belong to age group of around 26-35 years of age affecting males (60.4%) more than females (39.6%). Table 1: Distribution of cases according to age and sex
The distribution of major and minor symptoms of CRS among the study participants as shown in table 2 explains that majority of the patients had nasal discharge (83%), nasal obstruction (73.6%) and headache (73.6%) as the major symptoms. Post nasal drip (30.2%) was also found to be a significant symptom of chronic rhinosinusitis. Symptoms of facial pain (15%), cough (17%) and ear block (13%) also was suggestive of chronic rhinosinusitis. Most of the patients were found to seek tertiary care medical advice when the duration of symptoms lasted for more than six months. Table 2: Distribution of symptoms-duration of chronic rhinosinusitis
The distribution of adenoid size in CRS patients before and after therapy is depicted in table 3. Nasopharyngeal lymphoid tissue of size less than 3mm was not considered significant as there was an angulation difference of the nasal endoscope while taking measurements. It was found that, about (56.6%) had nasopharyngeal lymphoid tissue which was measurably significant in size. As the adenoid size in normal adults could not be done since the invasive investigation of DNE was not ethically feasible, there was no baseline as to the adenoid size in normal adults. But 13.2% (7/53) patients had nasopharyngeal lymphoid tissue more than 10 mm size which was significant to cause choanal obstruction. Table 3: Distribution of adenoid size in chronic sinusitis before and after therapy
The actual change in the size of nasopharyngeal lymphoid tissue following medical or medical and surgical treatment in table 4 shows that 9 patients (17%) had significant reduction >3mm difference in adenoid size. Only one patient of the 53 cases showed an increase in size of 1mm. This could be an observational error as well.
Table 4: Distribution of post therapy reduction in nasopharyngeal lymphoid tissue size
Paired t test was applied to detect any significant difference between pre-treatment and post-treatment nasopharyngeal lymphoid tissue sizes.
The mean pre-treatment nasopharyngeal lymphoid size was found to be 6.94mm (S.D=3.55). The t value was 6.656 with “p” value 0.000 (95% confidence interval=0.84 to 1.57). Statistically, the difference between pre-treatment and post-treatment nasopharyngeal lymphoid tissue size was found to be highly significant. Bacteriology of the chronic rhinosinusitis was studied by gram staining of nasal secretions and subjecting the nasal swabs to aerobic culture medium namely Blood agar, Mac Conkey agar and Chocolate agar and incubated for 48 hours to know the type of bacteria involved in sinusitis. Table 5: Distribution of microbiological flora in chronic rhinosinusitis
36 patients (67.9%) smears showed gram positive cocci and gram negative bacilli. Of the 53 nasal swabs, 24 grew bacteria in aerobic culture. Most common organisms were coagulase negative Staphylococcus (26%) and Staphylococcus aureus (7.5%). Other organisms grown were Micrococci, Streptococcusviridians, Streptococcus pneumoniae, Proteus vulgaris, Klebsiella, Acinetobacter baumanii and Pseudomonas aeruginosa. Anaerobic culture was not done because of the difficulty in inoculating the medium with sparse nasal secretions, which were collected and also the high cost involved in the anaerobic culture methods. Even though smears showed organisms in 36 cases (67.9%), cultures were grown only in 24 cases (45.3%). There were no organisms seen in 17 cases and no growth on aerobic cultures in 17(32%) DISCUSSION Nasal discharge (83%) and nasal obstruction (73.6%) were most common symptoms of CRS followed by headache (73.6%), post nasal drip (30.2%), cough (17%), facial pain (15%) and ear block (13.2%). All these minor symptoms were considered as diagnostic for chronic rhinosinusitis, according to the Task Force on Rhinosinusitis in 199710. Rigid nasal endoscope to obtain middle meatal sample for culture and sensitivity which is considered as gold standard, less expensive and less morbid was used in this study. The pattern of sinusitis was different in various phases like during seven to ten days of onset, acute bacterial infection was caused by facultative aerobic bacteria namely Streptococcus pneumoniae, Hemophilus influenza and Moraxella catarrhalis whereas by three months, the anaerobic bacterial flora became predominant overtime. Talbot et al11 have obtained cultures from middle meatus endoscopically, and have found that the results had good correlation between cultures of middle meatus obtained by sinus aspiration. Studies like Jiang et al12 have shown that microbiology of bacteriology of chronic rhinosinusitis in maxillary and ethmoid sinuses comprised Staphylococcus aureus, Staphylococcus epidermidis, anaerobic and gram negative bacteria to predominate similar to the finding of coagulase negative Staphylococcal (26.4%) predominance in this study. Gram negative bacilli and gram positive cocci were seen in the smears but failed to grow on cultures, probably due to the high concentration of antibiotics in the patients from the treatment received before visiting the hospital. It could also be due to anaerobic infections which were not isolated as anaerobic culture methods were not employed in the study. The inoculation of the anaerobic medium with the sparse middle meatal secretions was difficult and also anaerobic culture methods were expensive. It is also possible that some patients had non-infectious secretions from the paranasal sinuses as the drainage was impeded due to inflammation of paranasal sinus mucosa. Pseudomonas aeruginosa, Proteus mirabilis and Klebsiella were some of the rare gram negative organisms isolated from the middle meatus of some patients in this study. Polymicrobial infection was also reported in two patients namely Acinetobacter baumanii and Pseudomonas aeruginosa in one patient and Streptococcus viridans and coagulase negative staphylococcus in other patient as described by Finegold et al.13 Nasopharyngeal lymphoid tissue enlargement in adults is usually seen in cases of allergic rhinitis. Significant enlargement of nasopharyngeal lymphoid tissue was seen in 30/53 (56.6%) cases of chronic rhinosinusitis and none of them had an allergic component. So nasopharyngeal lymphoid tissue enlargement in adults, could also be due to chronic rhinosinusitis. There were 7 patients who had highly significant nasopharyngeal lymphoid tissue enlargement to cause ¾ or full choanal obstruction which is similarly described by Kamel and Ishak et al.14 A significant reduction in nasopharyngeal lymphoid tissue size(>3mm), after treatment for sinusitis was seen only in 9/53(17%) cases. The nasopharyngeal tissue size increase may have been due to an inflammatory response of adenoids following sinusitis rather than actual hypertrophy, and so it’s reduction in size following treatment. The relation between adenoid microbiology, size of nasopharyngeal lymphoid tissue and maxillary sinus microbiology with both chronic sinusitis and adenoid hypertrophy was studied by Tuncer et al15 which showed no relationship between adenoid size and maxillary sinus culture positivity similar to the findings obtained in this study. There was a significant increase in nasopharyngeal tissue size who were culture positive compared to those who were culture negative (p value=0.000). However the size of nasopharyngeal lymphoid tissue size in normal adults in not available.
CONCLUSION Chronic rhinosinusitis adult patients commonly present with nasal discharge, nasal obstruction and headache with significant nasopharyngeal lymphoid tissue enlargement causing choanal obstruction. It is commonly associated with coagulase negative staphylococcal and Staphylococcus aureus infection with inflammatory pathology leading to the enlargement of lymphoid tissue. Nasal endoscopic guided sinus samples are a reliable method for smear collection from middle meatus and culture from chronic rhinosinusitis patients and are associated with less morbidity to the patients.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home
