Evaluation of bacteriology with their sensitivity and resistance status in chronic suppurative oititis media
Paparaja S1, Madhukar M2*
1Assiatant Professor, Department of ENT, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, Karnataka, INDIA.
2Assistnat Professor, Department of ENT, Kanachur Institute of Medical Sciences, Mangalore, Karnataka, INDIA.
Email:dr.madhukargowda@gmail.com
Abstract Background: Chronic Suppurative Otitis Media (COM) is one of the major ear disorders. The severity and symptoms in COM is depends on the microorganism. Antimicrobial agents are commonly prescribed to treat COM. The present study planned to screen the type of microorganism with its sensitivity and resistance status. Materials and Methods: This study was conducted in the Department of ENT, tertiary care hospital for a period of one year from January 2018 to December 2018. 30 patients with COM were included in the study. The patients with ear discharge and not used any antibiotics, ear discharge samples were collected from each patient and used for analysis. Results: In 30 patients most of them were diagnosed with mucosal disease. Gram negative organism was maximum number. Most of the organisms showed resistance. Conclusion: Analysis of microorganism profile with resistance and sensitivity plays important in the treatment of COM. Knowing microbial resistance can improve the patient’s treatment outcome.
Keywords: Infection, Microorganism, Chronic Otitis Media, Sensitivity, Resistance, Gram negative bacteria
INTRODUCTION
Chronic Otitis Media (COM) is one of the major problems facing the developing countries. This can be developed any age and both gender. Peoples staying in dust environment and not properly maintaining the ear hygiene will be prone to the COM1,2. When the balance between the disease progression and healing will change can lead the development of disease. The manifestations of disease are depends on the area and microorganism affected ear. COM is commonly known as long term inflammatory disease affecting the middle ear mucosal lining. Based on the disease symptoms and area affected it is classified in to two types (Mucosal and squamous)3. In both types the bacterial etiology and resistance status will be different. Mucosal mainly incomplete/recurrent cases, in these mainly resistant microorganisms will be observed. In second type newly infected patients4. The symptoms in both cases are different due to infection of various types of microorganisms. Normally COM is treated with various micro-organisms. In that sulfonmamides, aminoglycosides and macrolide antibiotics are most commonly used. But due to wide spread use of antibiotics, various organisms developed the resistance against common anti-biotics5. The preset study aimed to find out the microbial profile with resistance and sensitivity in patients suffering with Chronic Otitis Media.
MATERIALS AND METHODS
Study settings: This study was conducted in department of ENT at teaching hospital.
Inclusion criteria
- Single/both ear discharge last 4 months
- Ear discharge with tympanic membrane perforation.
- Mucosal subtype of COM
- Squamous type of COM
- Patents willing to give inform consent
Exclusion criteria
- Already on systemic/local antibiotic usage.
- Contaminated ear discharge samples.
- Childers
- Not willing to give inform consent
- Not willing to give ear swab sample
Procedure
A total of 30 patients were selected in this study. They were selected randomly based on inclusion and exclusion criteria. All patients were explained study procedure in their understandable language. All the patients’ demographic and clinical data was collected. Ear discharge samples were also collected under aseptic conditions. The samples were subjected to microbiological examination.
Statistical analysis
The data was expressed in number and percentage. Chi square test applied to find the statistical significant between the groups. P value less than 0.05 considered statically significant at 95 % confidence interval.
RESULTS
Males (n=22) and females (n=8) were included in this study. Maximum males compared to females. 18 patients showed age between 20-25 years. Less number (n=5) of patients showed complained ear discharge compared to other patients (n=25). In the 25 most of them showed middle ear infection compared to others. Pseudomonas aeruginosa is the most commonly identified microorganism in this study. S. aureus, klebsiella and proteus are the other microorganisms isolated in this study. Most of the antibiotics showed resistance.
Table 1: Demographic data of study population
Observation |
Number |
Percentage (%) |
Age (Years) |
|
|
20-25 |
22 |
73.33 |
26-30 |
6 |
20.00 |
31-35 |
2 |
6.67 |
Gender |
|
|
Male |
22 |
73.33 |
Female |
8 |
26.67 |
Ear discharge |
|
|
Yes |
5 |
16.67 |
No |
25 |
83.33 |
Site of ear infection |
|
|
Middle part |
25 |
83.33 |
Other parts of ear |
5 |
16.67 |
Table 2: Distribution of patients based on the microorganism isolated
Microorganism |
Number |
Percentage (%) |
Pseudomonas aeruginosa |
20 |
66.67 |
Staphylococcus aureus |
5 |
16.67 |
Klebsiella |
3 |
10.00 |
Proteus |
2 |
6.66 |
Table 3: Sensitivity pattern of antibiotics against Pseudomonas aeruginosa
Antibiotic |
Sensitivity |
Gentamicin
|
15 |
Ceftriaxone |
14 |
Ciprofloxacin |
12 |
Amikacin |
8 |
Cefotaxime |
6 |
Cefuroxime |
7 |
Ampicillin / Amoxicillin |
10 |
Ofloxacin |
15 |
Cefoperazone |
16 |
Ceftazidime |
17 |
Table 4: Sensitivity and resistance pattern of antibiotics against Staphylococcus aureus
Antibiotic |
Sensitivity |
Ampicillin / Amoxicillin |
4 |
Cefoxitin / Oxacillin |
3 |
Ceftazidime |
2 |
Chloramphenicol
|
4 |
Ceftriaxone |
5 |
Gentamicin |
4 |
Ciprofloxacin |
4 |
Amikacin |
4 |
Cefotaxime |
3 |
Cephalexin |
2 |
Cotrimoxazole |
4 |
Erythromicin |
2 |
Cefoperazone |
2 |
Cefuroxime |
5 |
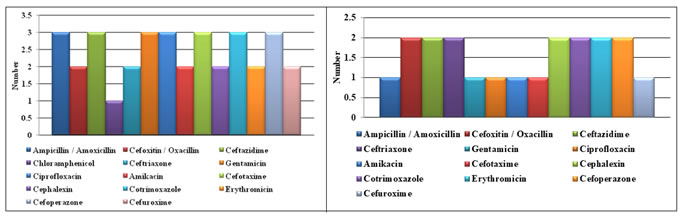
Figure 1 Figure 2
Figure 1: Sensitivity and resistance pattern of antibiotics against Klebsiella; Figure 2: Sensitivity and resistance pattern of antibiotics against Proteus
DISCUSSION
COM is the most common disease associated with decreased hearing and discharge. Early diagnosis and incitation of treatment can prevent the hearing loss patients with COM. Treatment outcome in patients with COM is depend on the progression of disease and anti-biotic used. Antibiotics are the most commonly used drugs for COM. The effect of drugs is depends on the sensitivity and resistance of micro-organism. Vijaya D et.al., and Srivastava et.al., studies showed more males than females6,7. The present study results showed more males than females. Gram-ve microorganism was common in this study. The study done by Poorey VK showed gram-ve micro-organisms are common class compared to others. In this study P. aeruginosa is the commonest microorganism isolated8. Tanmoy D et.al., study also showed similar results. They also observed that S. aureus is the next common organism isolated in this study9. Fliss DM study also showed S. aureus is the next commonest microorganism compared to others10. In the present study, the organisms isolated shows maximum sensitivity to Gentamicin followed by Ciprofloxacin, Amikacin, Cefotaxime and is comparable with studies done by Atanu Nandy et.al., in a bacteriological study of CSOM, out of total 146 cases of CSOM and out of total 192 isolates, total bacteria put for antibiotic sensitivity tests showed susceptibility towards Gentamicin followed by Chloramphenicol (31.3%) and Ampicillin (14.8%)10. Rao et.al., in a study of CSOM-A prospective study, random selection of 120 cases of CSOM were investigated for bacterial and fungal isolates. Total of 145 bacterial isolates were identified and their susceptibility to various antibiotics was tested. The majority of the bacterial isolates showed multiple drug resistance. Gentamicin was the drug of choice in treating the causative strains of either Gram positive or Gram negative bacteria and tetracycline was found to be the least effective11. Kabir MS, In a study pattern of CSOM, Among antibiotics, most effective was Amikacin, then Gentamicin, Ciprofloxacin, Ceftazidime, Ceftriaxone12. Tanmoy Deb et al in 2012, suggested Ciprofloxacin due to ease of availability, least ototoxicity and cost effectiveness, is an important tool in active CSOM management13. A Yousuf et al in 2012, did a study on bacteriological profile of ear discharge and their antibiotic sensitivity in CSOM and showed that 72% isolates were sensitive to Gentamicin, 55% to ciprofloxacin, 36% to Cephalosporins (Cetazidime, Ceftriaxone). For P. aeruginosa 72% isolates were sensitive to Piperacillin / Tazobactum, 48% to Ciprofloxacin and 32% to Ceftazidime / Ceftriaxone. Ciprofloxacin and Gentamicin has the highest susceptibility rate among the topical antibiotic ear drops14. F. Ricciardiello et al in 2009, studied on Microbiology of cholesteatoma suggested that the most effective antibiotics are Fluoroquinoles (Ciprofloxacin or Levofloxaxin). In children, it is advisable to use third generation Cephalosporins or a combination of Amoxicillin and Clavulanic acid15.Maji P.K et al in 2007 showed that P.aeruginosa to be the most prevalent oganism and showed that the most sensitive antibiotic was Amikacin against CSOM16. Saini. S et al in 2005 suggested the usage of Cefotaxime, Cefuroxime or Gentamicin for gram negative bacilli and Clindamycin, Cloxacillin or Cefuroxime for S.aureus³³. BM ahmad et al in 2003, in a retrospective study of 206 patients with CSOM, Antibiotic sensitivity result showed that Gentamicin (88.5%), Cefuroxime (63.7%) and Cephalexin (61.7%) were active against majority of the isolates17. In the present study, P.aeruginosa is highly sensitive to Gentamicin followed by Ciprofloxacin, Ceftriaxone, Cefotaxime, Amikacin, Cefuroxime and is comparable with the studies done by Atanu Nandy et al in 1991, which also showed P.aeruginosa susceptibility towards Gentamicin followed by Chloramphenicol (31.3%) and Ampicillin (14.8%)18. The presser study results are similar to other studies.
CONCLUSION
COMs are the most common ear infection. Gram-Ve micrograms are common. Early diagnosis and treatment will improve the disease condition. Improve the disease progression by treating with sensitive microorganisms rather than resistance agents.
REFERENCES
- Gupta V, Gupta A, Sivarajan K, CSOM - an aerobic microbiological study. Indian J Otol 1998;4:79-82.
- Poorey V.K, lyer A. Study of bacterial flora in CSOM and its clinical significance. Indian J Otolaryngol Head Neck Surg 2002;54(2):91-5.
- Schuknecht HF. Pathology of the Ear. Lee and Febiger: Pennsylvania: 1993(2):31-46.
- Ballantyne J, Groves J. Scott Brown’s diseases of the ear, nose and throat. Butterworth and Co: London; 1979 4(2):1-100.
- Wright A. Anatomy and ultrastructure of the human ear. In: Gleeson M.Ed. Scott Brown’s Otolaryngology, Butterworth Heinemann: Oxford;1997(6):10-50.
- Vijaya D. Aerobes, Anaerobes and Fungi in CSOM. Indian J Otol 2000;6(3):55-8.
- VK Srivastava, SK Agarwal, GK Malik. CSOM in children. The Indian J of Pediatrics. 1979; 46(10):363-7.
- Deb T, Ray D. A study of the bacteriological Profile of CSOM in agartala. Indian J Otolaryngol Head Neck Surg 2012; 64(4): 326-9.
- Fliss DM, Dagan R, Meidan N, Leiberman A. Aerobic Bacteriology of CSOM without Cholesteatoma in Children. Ann Otol Rhinol Laryngol 1992;101(54):866-9.
- Atanu Nandy, PS Mallya, K Sivarajan. CSOM – A bacteriological study. Indian J Otol 1991;43(3):136-8.
- Rao BN, Reddy MS. CSOM – A prospective study. Indian J Otolaryngol Head Neck Surg 1994;46(2):72-7.
- Kabir MS, Joarder AH, Ekramuddaula FM, Uddin MM, Islam M, Habib MA. Pattern of CSOM. Med J 2012;21(2): 270-5.
- A Yousuf, M Malik, IU Shamas, Z Beigh, S Kumari, PRA Pampori. Bacteriological Profile of Ear Discharge and their Antibiotic Sensitivity in CSOM in Kashmir, India. Bangladesh J of Med Sci 2003;11(3): 59-63.
- F Ricciardiello, M Cavaliere, M Mesolella, M Lengo. Microbiology of cholesteatoma: clinical findings and treatment. Acta Otorhinolaryngol Ital 2009; 29(4):197-02.
- Maji PK, Chatterjee TK, Chatterjee S, Chakrabarty J, Mukhopadhyay BB. The investigation of bacteriology of CSOM in patients attending a tertiary care hospital with special emphasis on seasonal variation. Indian J Otolaryngol Head Neck surg 2007;59:128-31.
- Saini S, Gupta N, Aparna, Seema, Sachdeva OP. Bacteriological study of pediatric and adult CSOM. Indian J Pathol Microbiology 2005;48(8):413-6.
- BM Ahmad, MT Kudi, CSOM in Gombe, Nigeria. Nigerian J of Surg Research. 2003;16(5):120-3.
- Atanu Nandy, PS Mallya, K Sivarajan. CSOM – A bacteriological study. Indian J Otol 1991;43(3):136-8.