|
Table of Content - Volume 11 Issue 3 - September 2019
A clinicomycological study of otomycosis in tertiary care institute
Shabana Mohamed Ali1, Vasanti Patil2*, Tushar Tajne3
Abstract Background: Otomycosis is a chronic or subacute, recurrent, non-contagious, persistent superficial fungal infection of the ear, usually located in the external ear. The management of otomycosis is dependent on knowledge of microbiology of potential pathogens and familiarity with clinical presentation. Aim: To study the commonest fungi causing otomycosis, most common mode of presentation and effect of various antifungal agents in diagnosed cases of otomycosis. Material and Methods: This cross sectional study included 256 patients diagnosed with otomycosis. Fungal culture and other investigations were done in microbiology laboratory and accordingly the treatment was given. Results: The predominant complaint of the patient was itching 100% followed by pain (188 cases, 73.44%), ear discharge (139 cases, 54.3%), hearing loss (125 cases, 48.83%). In total 229 (89.45%) cases were caused by Aspergillus species and 16(6.25%) cases were by Penicilium notatum, and rest 11(4.30) cases caused by Candida albicans. 1% clotrimazole ear drop was more effective with very good response in 78.82% of cases. Conclusion: Aspergillus is found to be the commonest etiological agent causing otomycosis, followed by Penicillium. Commonest mode of presentation of otomycosis is pruritis, otalgia and ear discharge. Most of the patients responded to clotrimazole. Key Words: Otomycosis, itching, Aspergillus, clotrimazole
INTRODUCTION Fungal infection of the external ear canal and auricle, is a common source of concern to the otolaryngologist as it is commonly found throughout the world. The prevalence of otomycosis is greatest in hot, humid and dusty areas of the tropics and subtropics. In Indian subcontinent, otomycosis has been consistently present in many cases presenting with discharging ears.1,2 Andral and Gaverret3 were the first to describe fungal infections of the ear. Although a widespectrum of fungi are involved, Aspergillus is the most common agent causing otomycosis. Among Candida species, Candida albicans is the most common isolate followed by Candida parapsilosis, Candida glabrata, Candida guilliermondii and Candida krusei. Other fungi like Penicillium, Mucor, Rhizopus, are also involved. The management of otomycosis is dependent on knowledge of microbiology of potential pathogens and familiarity with clinical presentation so that an accurate and timely diagnosis and management can be reached.7 In current study an attempt was made to study the commonest fungi causing otomycosis, most common mode of presentation and effect of various antifungal agents in diagnosed cases of otomycosis.
MATERIAL AND METHODS This cross sectional study included patients visited Otorhinolaryngology out-patient department at Tertiary Care Hospital. Investigations were done in central clinical laboratory and microbiology laboratory and accordingly the treatment was given. Sample size In a study of da Silva Pontes ZB et al,1 otomycosis was diagnosed in 19.4% of patients. With this information sample size was calculated by the formula: n=4pq/d2 (where, n=Sample size; d=Allowance error; p=Prevalence; q= 100- p) thus, n = 4 x19.4 x (100 -19.4)/25 = 250.18 In the present study period, we observed 260 patients of otomycosis and 256 patients gave consent for participating in the study, and all 256 patients were included in the study. Inclusion criteria
Exclusion criteria
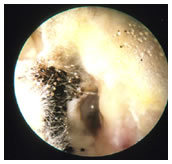
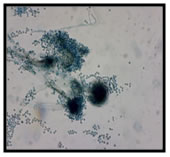
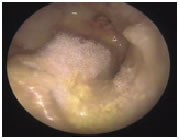
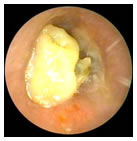
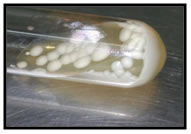
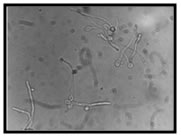
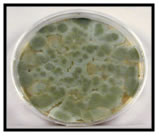
Statistical analysis Data was analysed using IBM SPSS version 20.0. Qualitative data was presented using frequencies and proportions, and quantitative data was presented using mean and standard deviation. To find association between two qualitative variables, chi square or fisher exact test was used wherever necessary. Significance was considered if ‘p’ value is less than 0.05. Methodology Detailed history of patients was taken including predisposing factors, signs and symptoms etc. All patients were undergone a detailed clinical examination in the Otorhinolaryngology outpatient department, to evaluate auditory canal and tympanic membrane by otoscope, otoendoscope and otomicroscope wherever required. Sterile ear swabs were taken and send to microbiology laboratory. Collection of samples Debris in the external auditory canal was collected using sterile swabs, after cleaning the pinna and adjacent areas with antiseptic solution. The collected specimen was sent to the lab promptly along with a proper requisition slip and processed within 30 minutes. No transport media was used. Processing of samples Direct Microscopy with 10% Potassium Hydroxide Mount was done followed by fungal culture by inoculated onto Sabouraud’s dextrose agar slopes in duplicate. All inoculated media were incubated at 25°C and were observed daily for upto 4 weeks to look for fungal growth. The fungal growth was then subjected to microscopic examination using LPCB, gram staining, germ tube test Evaluation of effect of antifungal agents Identification and elimination of predisposing factors were done and the debris in the external auditory canal was thoroughly cleaned by suction aspiration and dry mopped and treatment was given. Patients were offered treatment with topical antifungals and those who did not respond to topical antifungals (1% clotrimazole, 1% tolnaftate, cicloproxolomine creams) were given systemic antifungals. Follow up was done once weekly for one month and progress was noted in terms of reduction of symptoms and signs. Oral antifungal agent itraconazole was used in cases which didn't respond to topical antifungals and the progress was noted. RESULTS Photo 1: Aspergillus niger 1. Otoendoscopy 2. LPCB mount 3. Culture
1. Otoendoscopy 2. LPCB mount 3. Culture
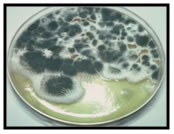
1. Otoendocopy 2. Germ tube test 3. Culture Photo 4: Penicillium notatum 1. Culture 2. LPCB mount
In present study patients having otomycosis in the age group of 11-60 years were included. The youngest patient was of 13 years and oldest patient was of 60 years. The mean age was 33.45 years with standard deviation 14.85 years. Maximum numbers of cases were between 11- 30 years of age (55.86%). 148 (57.81%) patients were female and 108 (42.19%) patients were male. The incidence of otomycosis was more among females as per present study. Out of total number of cases 228 (89.06%) patients had only one ear involvement. The right ear was involved in 122 (47.66%) cases and left ear was involved in 106(41.41%) cases. In 28 (10.94%) cases both ears were involved. Out of 256 cases, 117 (45.70%) were housewives, 57 were farmers, 46 were students, 21 were businessmen, 10 were teachers and 5 were security guard. In present study the incidence of otomycosis was high among housewives, and least among security guard. The comparative outpatient strength of housewives was higher when compared to other groups. In the present study the most common pre-disposing factor was injury to ear canal in 186 cases (72.66%) followed by use of ear drops in 178 (69.53%) cases. Associated systemic disease was observed in 26 (10.16%) cases, out of them 21 cases had diabetes and 5 cases had both HIV and TB. In the present study 37 (14.46%) cases had associated ear disease in the form of chronic otitis media, out of that 26 (10.16%) patients had unilateral chronic otitis media and 11 (4.13%) patients had bilateral chronic otitis media. In the present study pH of the canal was studied using universal pH indicator strips. In all cases the pH was alkaline. Most of the cases [143 (55.86%)] had pH level in the range of 7.6 to 8.0. 87 (33.98%) cases had pH level in the range of 8.1 to 8.5 and 26 (10.16%) cases had 7 to 7.5 pH level. In present study, the predominant complaint of the patient was itching 100% followed by pain (188 cases, 73.44%), ear discharge (139 cases, 54.3%), hearing loss (125 cases, 48.83%), ear blockage (75 cases, 29.3%) and tinnitus (34 cases, 13.28%). The least common complaint was tinnitus. Table 1: Mode of presentation
Commonest mode of presentation was with itching, pain and ear discharge which was seen in 58 (22.66%) cases, preceding to that in 42 (16.41%) cases itching and pain was seen and in 25 (9.77%) cases itching, pain, ear discharge and ear blockage was seen. Isolated presentation of itching was seen in 2.34% of cases.
Table 2: Fungal Species
In the present study, the swab material was cultured in Sabouraud’s dextrose agar and showed, 163 (63.67%) cases were caused by Aspergilus niger, 55 (21.48%) cases were caused by Aspergillus flavus, 16 (6.25%) cases were caused by Pencillium notatum, 11 (4.30%) cases were caused by Candida albicans, and 11 (4.30%) cases were Aspergillus fumigates. In total 229 (89.45%) cases were caused by Aspergillus species and 16(6.25%) cases were by Penicilium notatum, and rest 11(4.30) cases caused by Candida albicans. This difference in the improvement rate among the 3 drugs used namely 1% clotrimazole, 1% tolnaftate and 1% ciclopiroxolamine was statistically significant (p value<0.00001). In the present study, 1% clotrimazole ear drop was more effective with very good response in 78.82% of cases followed by 1% tolnaftate cream 58.14% of cases and 1% ciclopiroxolamine in 23.52% of cases.In 16 (6.25%) of cases who didn’t respond to topical antifungal, 11 (4.29%) cases were associated with diabetes mellitus and 5 (1.95%) cases were associated with chronic otitis media. All were given systemic antifungal agent itraconazole which was effective in all of them.
DISCUSSION Otomycosis is a disease frequently encountered by otolaryngologists and can usually be diagnosed by clinical and laboratory examinations. Fungal infections of the external ear are frequent in tropical countries, because of humidity and heat. Fungi could be mentioned as a normal microflora in the external auditory canal playing an important role in otomycosis. Various factors pave the way for such saprophytic organisms to gain a foothold in the external auditory canal. Fungal infections in the ear are increasing especially with indiscriminate use of topical antibiotic/steroid preparations and unhygienic habits. Treatment of otomycosis consists of adequate aural toilet, altering the pH of the external auditory canal with acidifying agents and topical anti-fungal agents. In the present study, the predominant complaint was itching (100%) and least common complaint was tinnitus (13.28%). This is comparable to other studies. In a study by Ali K et al,5 most common symptoms of otomycosis were pruritis (92.16%), and otalgia (50.98%), hearing loss (23.53%) and ear discharge (20.59%). In a study conducted by Prasad SC et al,6 itching was the predominant symptom seen in 73% of the otomycotic patients followed by ear blockage (38%), ear discharge (38%), ear pain (35%) and tinnitus (8%). In our study, commonest mode of presentation was with itching, pain and ear discharge which was seen in 22.66% of cases. In study by Fasunla et al,7 the commonest mode of presentation included aural pruritus (90.21%), otalgia (83.86%) and tinnitus (78.31%). In the present study, 89.45% cases were caused by Aspergillus genus, 6.25% of cases were caused by Penicilium and rest 4.30% of cases caused by Candida. Out of 89.45% of cases, 63.67% of cases were caused by Aspergillus niger species, 21.48% of cases were caused by Aspergillus flavus species, 4.30% of cases were Aspergillus fumigatus, 6.25% of cases were caused by Pencillium notatum and 4.30% of cases were caused by Candida albicans. This resembles studies by other authors. In a study by Prasad SC et al,6 Aspergillus (80%) was most common genus isolated, Penicillium (8%) was the second most common isolated, and Candida albicans constituting only 4%. Our study was comparable with a study done by Rao et al.8 In their study, Aspergillus niger (44.7%) was the predominant species isolated, Aspergillus flavus (29.8%) was the second most common species isolated. Aspergillus fumigatus (11.7%), Candida species (8.5%), Mucor (2.1%) and Penicillium species (2.1%) were the other species isolated by them. In a study by Ali K et al,5 Aspergillus niger (50.98%) was the most common isolated organism, followed by Aspergillus flavus (33.33%), and then by Candida species (14.7%). However, studies by Barati et al,9 Aspergillus flavus was the most common organism (49%), followed by Aspergillus niger (41.6%), Aspergillus fumigatus (5.5%) and Aspergillus nidulans (3.7%). In recent study by Sabz G et al,10 the most common isolated fungi were Aspergillus tubingensis. In their study, Aspergillus species were 77.92%, including 47.40% isolates of Aspergillus niger, 27.92% of Aspergillus flavus, 1.94% of Aspergillus terrei and 0.6% of Aspergillus fumigatus. After molecular sequencing, 28.57% out of 47.40% strains primarily identified as Aspergillus niger turned out to be Aspergillus tubingensis. Thus, they finally found 28.57% of Aspergillus tubingensis and 18.83% Aspergillus niger. Species of Candida constituted 8.5% of fungal isolates. Penicillium were not isolated from cases in their study. In the present study 1% clotrimazole drop was more effective with response seen in 83 cases (97.65%) out of 85 cases, followed by 1% tolnaftate cream in 81 cases (94.18%) out of 86 cases and 1% ciclopiroxolamine cream in 76 cases (89.41%) out of 85 cases. This correlates with previous studies by other authors. In a study conducted by Jimenez-Garcia L et al,11 they recorded, treatment with 1% clotrimazole resulted in 75% resolution and 45% resolution with treatment with 1% tolnaftate at one week of treatment. They concluded that treatment with clotrimazole is more effective than Tolnaftate for uncomplicated otomycosis. In a study by Paulose KO et al,12 they found improvement in range of 89% and 81% for clotrimazole and tolnaftate respectively. In the present study itraconazole was given to 6.25% of cases who didn’t show response to topical anti fungals, and found improvement in all cases. In a study by Vennewald I, Klemm E,13 they mentioned itraconazole was effective in cases with tympanic membrane perforation. Recently many reported Candida auris as a multidrug-resistant yeast that causes invasive infections. It was first described in 2009 in Japan, collected from external ear of a Japanese patient by K Satoh et al.14 It is an emerging serious public health threat with high mortality and morbidity that can range from mild superficial infections to fungemia. Candida auris is an emerging nosocomial pathogen with a high potential for multidrug-resistance. The global increase in reports of Candida auris, transmission in health care facilities, frequent relapse and treatment failures qualifies Candida auris as one of the top ten most serious fungal pathogens. Schwartz IS15 quoted that management of otomycosis and otomastoiditis caused by Candida auris is even less clear. Evaluations of the efficacy of ototopical agents against Candida auris have not been published and the options for multidrug-resistant isolates are limited. As per Rudramurthy SM16 in India, for instance, Candida auris already accounts for 5% of the isolates implicated in candidemia in intensive care units nationwide. Abastabar M et al17 recently reported a cases with Candida auris in Iran. Molecular methods like DNA sequence based fungal species identifications were not used in the present study because, they involve significant cost and phylogenetic expertise.
CONCLUSION In the present study, Aspergillus is found to be the commonest etiological agent causing otomycosis, followed by Penicillium. Habitual ear cleansing leading to trauma of external auditory canal has been found to be the most common predisposing factor. Commonest mode of presentation of otomycosis is pruritis, otalgia and ear discharge. Most of the patients responded to clotrimazole.
REFERENCES
|
|
 Home
Home