Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 1 - October 2019
Follicular variant of papillary carcinoma of thyroid with metastasis to mandible
Ruchika Jain1*, Tapan Nagpal2, Nirali Chauhan3, Ravina Jain4, Tosha Shah5
1,4,5Resident, HOD & Professor, 3Professor, Department of Otorhinology Dhiraj Hospital, Vadodara, Gujrat, INDIA. Email: ruchika0315@gmail.com
Abstract Metastatic papillary thyroid carcinoma (PTC) is uncommon and usually occurs in regional lymph nodes of neck, mandibular metastasis is a rare event. Few cases have been reported until now. A case of 50 year old female having follicular variant of papillary carcinoma with secondary metastasis in left ramus of mandible. Patient came with complaints of midline neck swelling since 15 years and swelling over left mandibular ramus since 2 years. The diagnosis of papillary thyroid carcinoma (PTC) with mandibular metastasis was made after radiological and cytological examination of both the lesions. Patient is treated with total thyroidectomy with left hemi mandibulectomy. Key Words: Papillary thyroid carcinoma, mandibular metastasis
INTRODUCTION Papillary thyroid carcinoma (PTC) accounts for approximately 80% of all thyroid cancers 1 many histopathologic variants of papillary carcinoma have been recognized; few of these are of prognostic significance. The presence of distant metastasis indicates poor prognosis associated with a decrease in survival rates.2 It is generally an asymptomatic, slow-growing nodule with desirable prognosis.3 Patients with differentiated thyroid carcinoma have a 10 year survival rate of 80-95%. However, when distant metastases are present, the overall 10 year survival rate is below 40%. Initial mandibular metastases are extremely rare with few cases reported in the literature.4
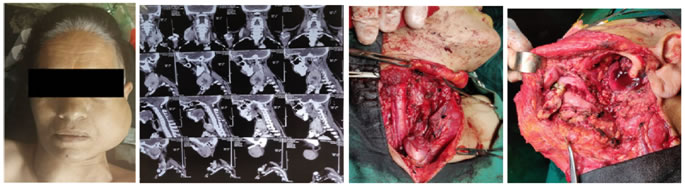
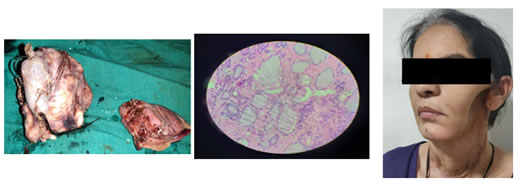
CASE REPORT A patient 50 year old female came to our institute with complaints of midline neck swelling since 15 years and swelling over left mandibular ramus since 2 years. On examination she had a diffuse midline neck swelling of size 15*8*5 cm which is firm non tender move with deglutination and overlying skin is normal. She also had left mandibular swelling of size 5*5 cm involving the ramus of mandible and restricted mouth opening. CT scan of patient revealed both lobes of thyroid grossly enlarged shows heterogeneous enhancement. Mass abutt bilateral sternocleidomastoid muscles, internal jugular vein, and causes compression of upper trachea. Large expansile lucent lesion was involving ramus of left mandible causing bony erosion and destruction. Fine needle aspiration cytology shows thyroid carcinoma with metastasis in mandible. The patient underwent total thyroidectomy with left hemi mandibulectomy under general anesthesia. Excised specimen was sent for histopathological examination suggestive of follicular variant of papillary carcinoma stage 4b (T4b Nx M1) which shows cells arranged predominantly in papillary pattern with central fibro vascular core. Cells shows round optically clear nuclei, grooving and moderate amount of cytoplasm. There is presence of wide fibrous band incompletely dividing tumor into lobules .Patient is on regular follow up with no postoperative complication. No further radiotherapy/chemotherapy given. Figure 1: Pre op picture Figure 2: CT scan images Figure 3: Total thyroidectomy Figure 4: Left hemimandibulectmy
Figure 5: Resected specimen Figure 6: Histopathology appearance Figure 7: post op picture
DISCUSSION Thyroid cancer represents 1.5% of all cancers. But it is the commonest endocrine cancer accounting for 92%.5. DeLellis defined papillary carcinoma as a well differentiated malignant epithelial tumor characterized by formation of papillary structures, psammoma bodies and a set of distinct nuclear features such as grooves, pseudo inclusions and ground glass appearance. 6 The mean age for well-differentiated thyroid cancer is 40 years for papillary type and 50 years for follicular type; so, it spends the time to metastasize to other regions.7 The metastasis in Papillary thyroid carcinoma commonly occurs to regional nodes only. Bone metastasis is rare in a patient with papillary thyroid carcinoma and it is seen in older patients. 8 Papillary thyroid carcinoma metastasis to the jaw is extremely rare and it accounts for about 3.85% of all jaw metastases of all head and neck carcinoma 9 The predilection of metastasis to the ramus and angle of the mandible reflects the rich blood circulation in the medullary cavity of these regions 10. The majority of papillary thyroid carcinoma (PTC) cases comprise classic papillary (C-PTC) and follicular variant (FV-PTC) histologic sub-type. Although several rarer subtypes of PTC (e.g., diffuse sclerosing, tall cell and columnar cell) are established indicators of poorer prognosis, FV-PTC and CP-PTC were historically believed to be low-risk subtypes that were essentially therapeutically and prognostically equivalent 11 Papillary carcinomas are diagnosed by the characteristic nuclear features. These include optically clear nuclei also known as “orphan annie” nuclei, nuclear grooves, intranuclear inclusions, and nuclear overcrowding. These features are enough to suggest papillary carcinoma even if the papillary pattern is absent in the tumor 12 Recent studies on the mechanism by which cancer metastasizes to bone have shown that cancer cells alter the physiologic balance between bone resorption and bone formation. Breast cancer metastases are frequently osteolytic and this has been attributed to overexpression of osteoclasts, inducing factors such as parathyroid hormone–related protein, interleukin (IL)-8, and 11.13 Predominantly osteoblastic metastasis is mediated by osteoblast-mediating factors, such as bone morphogenetic proteins, Wnt family ligands, endothelin 1, and platelet derived Growth factors (PGDF). Furthermore, the release of matrix embedded growth factors, such as insulin-like growth factors and transforming growth factor-beta upon osteolysis promotes the induction of osteoclast-promoting factors.14 Radiation exposure is one of the well‑known risk factors for PTC. Other risk factors include genetic factors preexisting nodular disease, and association with genetic syndromes such as familial adenomatous polyposis syndrome. 15
CONCLUSION Despite of classical PTC being more common FV-PTC cases is increasing in recent times. Their clinical behaviors are unique and represent an intermediate entity with clinical features that are between C-PTC and FV-PTC. Surgery is the main line of treatment with good prognosis and low recurrence rate.
REFERENCES
|
|
 Home
Home