Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Conventional versus endoscopic septoplasty: Our experience in a tertiary care hospital
Jolene Alokkan1*, Prashanth R Reddy2
1Assistant professor, Department of ENT, East Point College of Medical sciences, Virgo Nagar Post, Avalahalli, Bengaluru- 560049, Karnataka, INDIA. 2Senior Consultant, ENT & Endoscopic surgeon, BGS Global Hospital, Bengaluru, Karnataka, INDIA. Email: dr.jolenealokkan@gmail.com
Abstract Objective: To compare the outcome, symptom relief and complications amongst patients who underwent conventional versus endoscopic septoplasty in a tertiary care hospital over a period of nine months. 40 patients who had symptomatic nasal septal deviation were divided into the two groups. Results: Comparison of the symptom relief between the two groups was insignificant. However, conventional septoplasty was associated with more number and type of complications. Conclusion: Endoscopic septoplasty is easier to perform especially in cases where concurrent sinus surgery is indicated. It is also associated with fewer complications and has the advantage of being a teaching tool for the junior surgeons. Key Word: Conventional septoplasty, Endoscopic septoplasty.
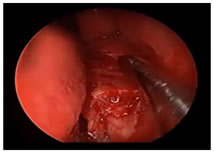
INTRODUCTION Nasal obstruction is a very common symptom for which patients visit the ENT OPD of a hospital. One of the common causes of unilateral or bilateral nasal obstruction is deviated nasal septum (DNS). The correction of a deviated nasal septum is surgical. DNS surgeries have undergone several modifications over the years: starting with submucosal resection which was radical and associated with complications to septoplasty which is conservative and has fewer complications 1. With the advent of endoscopes in surgeries of the nose and paranasal sinuses, endoscopic septoplasty has rapidly become more common and widely used, especially when combined with paranasal sinus surgery. As the surgeon has the endoscopes all set up and ready to go, there seems little sense in using headlight to perform an operation that is straight forward to perform with the endoscope. Endoscopes also allow better visualization, thereby reducing the risk of mucosal tears and better addressing of purely posterior deviation. In addition, performing the surgery using monitor allows all observers in the theatre to view the surgery and has significant advantage of allowing the surgeon to teach the operative steps to junior surgeons 2.
OBJECTIVEObjective of the study is to compare the outcome (symptom relief) & complications of conventional Vs endoscopic septoplasty in a group of patients in a multidisciplinary tertiary care hospital.
METHODThe study was conducted over a period of nine months at BGS Global Hospital, Bangalore between July 2015 to March 2016. 40 patients, who presented to the ENT OPD with complaints of nasal obstruction primarily and who were diagnosed to have deviated nasal septum with or without turbinate hypertrophy or sinusitis, were selected to undergo conventional or endoscopic septoplasty. Endoscopic septoplasty was preferred for such patients who also needed FESS. Patients younger than 12yrs and older than 70yrs were excluded from the study. All patients underwent diagnostic nasal endoscopy and CT scan of the nose and paranasal sinuses during the pre-operative work-up. Patients who needed FESS in addition to septoplasty were preferred for endoscopic septoplasty. Rest of the cases were assigned to the conventional or endoscopic group based on simple randomization. All surgeries were done under general anesthesia. The conventional steps of septoplasty were followed for the procedure among the patients undergoing conventional septoplasty. In the patients subjected for endoscopic septoplasty limited incision in front of the deviation was preferred wherever the deviation was limited or in cases of spur. Only cases where there was a mucosal tear intra-op, nasal splinting was done using silicon intra-nasal splint. These intra-nasal splints were removed at the 1week post-operative follow-up. Cases which had excessive bleeding intra-op were subjected to post-operative nasal tampon packing which was removed after 24 hrs. in case of only septoplasty and after 48hrs in cases which underwent septoplasty with turbinectomy. No suturing of the incision was done in any of the cases. All cases were followed-up in OPD on day 7, day 14 and at 1month post-op. RESULTSSample size of 40 patients was decided based on review of similar studies in the past. 40 patients included in the study were aged between 16 to 58 yrs. The youngest patient in the conventional septoplasty group was aged 18yrs and the oldest was 55yrs, while the youngest patient in the endoscopic septoplasty group was aged 16yrs and the oldest was 58yrs. Amongst the conventional septoplasty group, 12 patients underwent septoplasty alone as a single procedure, 4 patients underwent septoplasty with B/L turbinectomy and 4 patients underwent septoplasty with U/L turbinectomy. In the endoscopic septoplasty group, 8 patients underwent septoplasty as a standalone procedure, while 5 patients underwent septoplasty with FESS and 7 patients underwent septoplasty with FESS and turbinectomy. All 40 cases included in the study, were evaluated for the symptom relief. They were also subjected to nasal endoscopy on 7th post-op day to evaluate the healing and complications, if any. Pre-operative symptoms of all patients were recorded and compared with the post-operative symptom relief. The results were compiled and evaluated using chi-square test. In the conventional septoplasty group, there was a significant improvement in the nasal obstruction amongst the patients. Although 4 patients continued to have post-nasal drip following the surgery, none of them reported further episodes of epistasis and only 3 patients continued to experience headache.
Amongst the endoscopic septoplasty group, there was significant improvement in nasal obstruction, headache and post-nasal drip. None of the patients had recurrence of epistasis.
Comparison of the post-operative symptom relief between the two groups, showed better improvement in symptomatology like nasal obstruction, headache and post-nasal drip amongst the patients who underwent endoscopic septoplasty than amongst those who underwent conventional septoplasty. This can probably be attributed to the combination of endoscopic septoplasty with FESS at the same sitting with helped in better resolution of the associated sinusitis in cases with deviated nasal septum. The post-operative complications like delayed wound healing, residual deviation and septal perforation were seen only in the conventional septoplasty group. Intra- and post-operative hemorrhage and mucosal tears were also more frequent amongst the conventional septoplasty group. However, we found equal number of cases which developed post-operative synechiae amongst the two groups.
DISCUSSIONEndoscopic septoplasty was initially described by Stamberger&Lanza et.al in 1991. It is a minimally invasive technique that helps to correct deformity of septum under excellent visualization. Endoscopic septoplasty not only helps relieve obstructive symptoms, but also improves surgical access to middle meatus as an adjunct to endoscopic DCR & ESS 3. In the present study we compared the symptom relief and complications of conventional versus endoscopic septoplasty in a group of 40 patients with 20 patients in each group. The youngest patient to undergo conventional septoplasty, in our study, was 18 yrs. old, while the youngest to undergo endoscopic septoplasty was 16 yrs. old. However, septoplasty can be performed even in children as young as 4yrs old in case of clear indications 4. Conventional septoplasty as a single procedure was done is 12 patients while in 4 patients each it was combined with U/L or B/L turbinectomy. Endoscopic septoplasty was done a single procedure in 8 patients while in 5 patients endoscopic septoplasty was done along with FESS and in 7 patients endoscopic septoplasty was done along with FESS and turbinectomy. In 2005, Bayiz U et al concluded that septoplasty alone can be adequate treatment of chronic rhinosinusitis with septal deviation.5 However, with the extensive use of endoscope in ENT surgeries, septoplasty combined with FESS has shown better symptom relief 6. Hence the logical ease of combining FESS with endoscopic septoplasty. Comparison of post-operative symptom relief amongst the two groups in this study supports this fact, with better relief of headache in cases that underwent endoscopic septoplasty because of the combined FESS procedure that these patients underwent. In the present study, we found that intra-operative complications like mucosal tear and perforations were seen in conventional septoplasty and hence the need for splinting was also more in cases of conventional septoplasty. Another significant difference was that there was higher intra-op blood loss in patients undergoing conventional septoplasty necessitating post-operative nasal tampon packing (35% in conventional septoplasty group Vs 10% in endoscopic septoplasty group). Complications like delayed wound healing, residual deformity and perforation were seen only in the conventional septoplasty group, indicating that endoscopic septoplasty is safer and more efficacious than conventional septoplasty. Other similar studies also indicate superiority of endoscopic septoplasty compared to conventional septoplasty with complication rates around 14% in conventional group and close to 0% complication rate among the endoscopic septoplasty group.
CONCLUSIONBased on the above study, we conclude that endoscopic septoplasty is an easier, safer, faster and more conservative technique for treatment of symptomatic DNS and to provide access for other endoscopic nasal surgeries. It is associated with fewer complications and also helps teaching the steps of procedure to the training surgeon.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home