A comparison of graft uptake and hearing improvement in endoscopic cartilage tympanoplasty and endoscopic emporalis fascia tympanoplasty
P K Purushothaman1, Shruthi Sreekumar2, Dhanyan Harshidan3*
1Professor and HOD, 2PG, 3Assistant Professor, Department of Otorhinolaryngology, SRM Medical College Hospital and Research Centre, SRM Nagar, Chennai, Tamil Nadu, INDIA.
Email: shruthi_sreekumar@yahoo.co.in
Abstract AIM: To compare the hearing improvement and reperforation if any between, cartilage tympanoplasty and temporalis fascia tympanoplasty in inactive cases of chronic suppurative otitis media with a follow-up period of 3 months. Materials and Methods: A Randomized control study, involving 70 patients with Chronic Otitis Media, was conducted in the Dept. of ENT , SRM medical college hospital and research centre , kattankulathur, to compare reperforation if any and or hearing improvement following Tympanoplasty performed with the use of cartilage composite graft and Temporalis fascia graft from 2018 to 2020 with follow up upto 3 months. Result: (1) The patients’ ages ranged from 18 years to 60 years with a mean of 38 years; 31patients (44%) were female and 39 patients (52%) were male. In Group A, the patients who underwent cartilage tympanoplasty, 17 patients (48.6%) were female and 18 patients (51.4%) were male, and in the group B, who underwent temporalis fascia myringoplasty, 14 patients (40%) were female and 21 patients (60%) were male. The age and sex distribution were not found to be statistically significant (p>0.05). (2) Graft acceptance and no failure in the form of reperforation was achieved in 32 patients (91.4%) who underwent temporalis fascia tympanoplasty, whereas it was achieved in 28 patients (80%) in the cartilage tympanoplasty group. This difference was not statistically significant according to the chi-square test (p>0.05). (3) Ear discharge was noted in one patient who underwent cartilage tympanoplasty and in none from the temporalis fascia group this difference was not statically significant according to Fisher exact probability test (P>0.05) .(4) From Post-op improvement in Hearing (average air-bone gap in Db) assessment for Group A and Group B, it is clear that the mean air-bone gap in Group B has gone down post - op (17.51), which is slightly higher than that for Group A post-op (16.11). Indicating improvement in hearing postoperatively is slightly higher for Group B When compared to Group A. Conclusion: Chronic otitis media is a major health problem in a developing country like India leading to significant social handicap in terms of hearing loss. Various types of grafts and techniques are used to close the perforation of the tympanic membrane. Tympanoplasty by cartilage and temporalis fascia yielded near to equal graft uptake rates.
Key Words: Cartilage, Temporalis fascia, tympanoplasty
INTRODUCTION
Chronic otitis media (COM) as it is termed now, is a permanent abnormality of the pars tensa / flaccida, mostly as a result of an earlier AOM, negative middle ear pressure or otitis media with effusion, with classical presentation of otorrhoea, perforation in the pars tensa or pars flaccida, hard of hearing and ear pain for a period of more than 3 months1
According to WHO the Western Pacific and South-east Asian regions contribute about 85–90 % of the global burden from Chronic otitis media COM is one of the most common ear diseases in many of the developing countries.2 The COM is prevalent in the lower socioeconomic group. Various etiological causes have been enumerated as probable causes ultimately leading to COM. Namely ET Dysfunction, GERD, Craniofacial abnormalities, immunodeficiency. And the factors influencing the activity of COM are infection and URI. Acute otitis media and otitis media with effusion from childhood can lead to the development of permanent changes in the tympanic membrane. This causing histological degeneration of various layers of the tympanic membrane may result in the loss of elasticity of the tympanic membrane making it more susceptible to chronic perforation or retraction. COM can present with otorrhea, Otalgia and Hard of Hearing as the main complaints the basic investigations, including an oto endoscopic examination and radiographic examination helps in arriving at the diagnosis of COM. The primary aim of surgery for COM is to eradicate infection and disease and make the ear safe and dry. The success after tympanoplasty is only partly determined by a surgeons surgical skill. Other factors play an important role such as biological and technical factors.3 The basic principles of the surgical procedure were described by “Wullstein in 1952, with a free skin graft, and Zollner in 1955, using a pedicle graft .4 A number of grafts can be used for reconstruction of the tympanic membrane since then. Like temporalis fascia, tragal cartilage, choncal cartilage, vein graft etc. Cartilage and temporalis fascia tympanoplasty are two of the frequently done procedures. By far temporalis fascia graft has remained ideal with a high success rate in terms of hearing improvement as well as successful graft take up. However, in complex cases such as, and cases wherein failure rates are considered higher like as in Eustachian tube dysfunction, retraction pocket, adhesive otitis media, and subtotal or total perforation cartilage has been considered to be a better choice of graft especially in terms of graft take up. This is a study conducted in the Dept. of ENT, SRM medical college, Hospital And Research Centre, kattankulathur, to evaluate the effectiveness of composite cartilage versus temporalis fascia graft tympanoplasty with respect to improvement to hearing, uptake of graft, and any re-perforation of the neotympanum, if any, in patients who fulfil the inclusion criterion and give consent for the study. The graft materials used in this study were - Tragal cartilage, sliced to a thickness of 0.5 mm and Temporalis fascia, in group A and group B respectively.
MATERIALS AND METHODS
This Randomised control study was conducted in the Department of ENT SRM medical college hospital and research Centre. Kattankulathur -603203, from DEC 2018 TO JULY 2019. A total of 75 patients with chronic otitis media who were admitted in the Department of ENT were analysed during the study period. Cases diagnosed as chronic otitis media mucosal type, with anterior perforation, central perforations, Eustachian tube dysfunction with at least 3weeks of dry ear were included in the study. Patients below 18 years of age and those diagnosed with chronic otitis media, squamous disease, and with active ear discharge were excluded from the study. All cases underwent a thorough history taking, detailed clinical examination, oto-endoscopic examination, routine blood investigations, Computed Tomography scan of the Temporal bone and Pure Tone Audiometry were done. After getting anaesthetic fitness and consent for surgery and participation in the surgery, the cases were randomised in two groups using random allocation software (version 1.0 May 2004), and the sequence generation was done by independent software. Following which the cases in Group A underwent Typanoplasty with cartilage graft and Group B underwent Tympanoplasty with Temporalis Fascia graft. The pateints were given post op antibiotics for 6 days and on Eight post-operative day suture removal was done and aural pack removed. Antibiotic ear drops, at a dosage of night two drops for two weeks was initiated from the 7th postoperative day i.e. after suture and pack removal. Patient is advised to avoid head bath and entry of water into the ear for one month postoperatively. A pure tone audiogram was taken 3rd month of the postoperative period during follow up. During the follow-up postoperatively for 3 months, the patient was reviewed at regular intervals and was assessed for graft take up , ear discharge and reperforation if any and hearing improvement.
RESULTS
The final analysis included 35 patients in cartilage tympanoplasty group (Group A ) 35 patients in temporalis fascia graft group (Group B ).The patients’ ages ranged from 18 years to 60 years with a mean of 38 years; 31patients (44%) were female and 39 patients (52%) were male. In Group A, the patients who underwent palisade cartilage myringoplasty, 17 patients (48.6%) were female and 18 patients (51.4%) were male, and in the group B, who underwent temporalis fascia tympanoplasty, 14 patients (40%) were female and 21 patients (60%) were male. The age and sex distribution were not found to be statistically significant (p>0.05).
Table 1: AGE DISTRIBUTION
Age groups |
Cartilage graft |
Temporalis fascia graft |
Number |
% |
Number |
% |
11 – 20 years |
3 |
8.6 |
1 |
2.8 |
21 – 30 years |
6 |
17.1 |
9 |
25.7 |
31 – 40 years |
13 |
37.1 |
11 |
31.4 |
41 – 50 years |
4 |
11.4 |
8 |
22.9 |
51 – 60 years |
7 |
20.0 |
3 |
8.6 |
61 – 70 years |
2 |
5.8 |
3 |
8.6 |
Total |
35 |
100.00 |
35 |
100.00 |
Table 2: GENDER
Sex |
Group A |
% |
Group B |
% |
Chi Square |
P Value |
Male |
18 |
51.42 |
21 |
60 |
|
|
Female |
17 |
48.57 |
14 |
40 |
0.521 |
0.315 |
Total |
35 |
100 |
35 |
100 |
|
|
In all patients, a pure tone audiogram from 250 Hz to 8 KHz was obtained preoperatively. The follow up period was three months postoperatively. Graft acceptance and no failure in the form of reperforation was achieved in 32 patients (91.4%) who underwent temporalis fascia tympanoplasty, whereas it was achieved in 28 patients (80%) in the cartilage tympanoplasty group. This difference was not statistically significant according to the chi-square test (p>0.05).
Table 3: Reperforation of graft (During the 3 months Post op)
Reperfornation(3 months Post op) |
Group |
Chi Square Test |
P Value |
Group A |
% |
Group B |
% |
|
|
Present |
7 |
20 |
3 |
8.58 |
1.867 |
0.153 |
Absent |
28 |
80 |
32 |
91.42 |
|
|
Total |
35 |
100 |
35 |
100 |
|
|
Ear discharge was noted in one patient who underwent cartilage tympanoplasty and in none from the temporalis fascia group, this difference was not statically significant according to Fisher exact probability test (P>0.05) . Seven graft failures were observed in the patients who underwent cartilage tympanoplasty, but three graft failures were observed in the temporalis fascia tympanoplasty group in the form of reperforation and retraction and ear discharge. In both graft failures, a small perforation developed at the central part of the tympanic membrane.There were no significant complications such as graft lateralization. In each group, the postoperative results were satisfactory.
Table 4:
Ear discharge (3 months post op) |
Group |
Fisher exact probability test |
P Value |
Group A |
% |
Group B |
% |
|
|
Present |
1 |
2.86 |
0 |
0 |
1.014 |
0.500 |
Absent |
34 |
97.14 |
35 |
100 |
|
|
Total |
35 |
100 |
35 |
100 |
|
|
From Post-op improvement in Hearing (average air-bone gap in Db) assessment for Group A and Group B, it is clear that mean air-bone gap in Group B has gone down post - op (17.51), which is slightly higher than that for Group A post op (16.11). Indicating improvement in hearing postoperatively is slightly higher for Group B When compared to Group A. However when analysed statistically using UnPaired T test, the difference of mean of Improvement in Hearing (average air-bone gap in Db) of Group A and B was found to be statistically insignificant (p>0.05) Also, a comparison of the paired t test of air-bone gap changes between the two groups fascia group (15.329) and cartilage group (10.992) shows that reduction in air-bone gap is slightly significant among temporalis fascia graft group. Though Audiologic results between the two groups did not reveal any statistically significant differences.
Table 5: Pre-op versus Post-op PTA (average air bone gap in Db)Group A - Cartilage graft
Air Bone gap PTA in Db |
Group |
Paired t test |
P value |
Mean |
SEM |
|
|
Pre op |
47.51 |
0.89 |
10.992 |
0.0001 |
Post op |
31.40 |
1.52 |
|
|
Table 6: Group B Temporalis fascia graft
Air Bone PTA in dB |
Group |
Paired test |
P Value |
Mean |
SEM |
|
|
Pre op |
47.49 |
084 |
15.392 |
0.0001 |
Post op |
29.97 |
0.96 |
|
|
Improvement in hearing in terms of the difference between pre and post-operative average air-bone gap in dB, between the two groups at the end of 3 months follow up.
Table 7:
Group |
Improvement |
Paired t test |
P Value |
|
Mean |
SEM |
|
|
Group A |
16.11 |
1.47 |
-0.754 |
0.453 |
Group A |
17.51 |
1.14 |
|
|
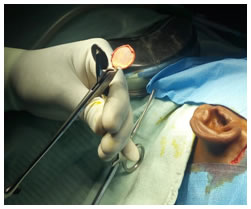

Figure 1: Temporalis fascia and Tragal cartilage harvesting
DISCUSSION
Though the usage of cartilage is experiencing a renaissance in tympanoplasty surgery it appears to offer an extremely reliable method for reconstruction of the tympanic membrane, mainly, in cases of advanced middle ear pathology and Eustachian tube dysfunction. Various types of cartilage grafts have been used like shield graft, palisade graft and cartilage grafts can either be harvested from tragal or conchal cartilage. Cartilage can also be used for ossicular reconstruction. While some studies have shown better improvement with sliced cartilage with a thickness of 0.5mm others prefer not slicing for the fear of graft curling. Cartilage from cartilage banks were in cartilage harvested from cadavers are stored in approximately 70% alcohol can be used however there are risks of pirion diseases in such grafts.
In this short-term study, patients with retraction with central/subtotal perforations, an intact ossicular chain, and at least a one month’s dry period was included. The graft acceptance without failure in terms of reperforation was 80% for the patients who underwent a cartilage tympanoplasty and 91.4% for the patients who underwent temporalis fascia myringoplasty; this difference was not statistically significant. Our results were comparable to other studies. For example, “Haitham A. Alnori and colleagues conducted a study among 40 patients 18 of them receiving temporalis fascia graft (first group) and 22 received palisade cartilage as graft (second group),6 Surgical success rates for the first and second groups werev77.78% and 95.45%, respectively. There is19.4 dB improvement in mean hearing threshold in fascia group, compared to 15.2 dB improvement in cartilage group he concluded that there was no significant difference either in surgical success rate or in hearing gain between the two groups. Neumann and colleagues reviewed 84 cases of patients who underwent palisade technique, with mixed pathologies such as retraction with perforation, adhesive processes and chronic mesotympanal otitis, and found an overall graft acceptance rate of 97.6%. No perforations were found in patients following palisade cartilage myringoplasty, whereas there were four perforations in the patients who underwent temporalis fascia myringoplasty.7 In our study, auditory function in cartilage myringoplasty patients was not statistically different when compared to the gains observed in the patients who underwent temporalis fascia myringoplasty. However, comparing the paired t test, temporalis fascia graft shows significant improvement when compared with that of cartilage graft group. Other studies in the literature have also reported slight upper hand for temporalis fascia graft over cartilage graft.” “Rakesh and colleagues conducted a study involving 20 patients each in group A and B receiving temporalis facia and cartilage as graft respectively and concluded that 80% of the patients operated with temporalis fascia showed air-bone gap up to 20dB. 75% of the patients operated with tragal perichondrium showed air-bone gap up to 20dB. Mean improvement in hearing temporalis fascia is 09.5 Db. Mean improvement in hearing using tragal perichondrium is 09.0 Db . Mean improvement in hearing using tragal perichondrium is 09.0 Db.” “Kirazli and colleagues also found no significant difference between the audiologic results after cartilage perichondrium and temporalis fascia myringoplasty.8Similarly, a study by Cabra and colleagues observed no relevant differences between the functional results of the two procedures (composite cartilage tympanoplasty and temporalis fascia tympanoplasty).9 The ideal acoustic thickness of cartilage should be approximately 0.5 mm. The full thickness is 0.7 to 1 mm. However, reducing the thickness of cartilage makes it difficult for reconstruction due to the inevitable twisting of the cartilage.10 We applied full thickness cartilage in our procedure. Experimental histopathologic studies have shown that cartilage is stable because of the fibrile structure of the matrix, which is independent of the survival of cellular elements. Reconstruction of the tympanic membrane using the cartilage technique in myringoplasties allowed us to achieve good anatomic and audiologic results that were at least similar, if not better than traditional methods of reconstruction in high-risk cases.
CONCLUSION
Chronic otitis media is a major health problem in a developing country like India leading to significant social handicap in terms of hearing loss. Various types of grafts and techniques are used to close the perforation of the tympanic membrane. Tympanoplasty by cartilage palisade and temporalis fascia yielded near to equal graft uptake rates. Improvement in hearing is was slightly better with temporalis fascia as graft when compared to cartilage palisade graft. However cartilage tympanoplasty may be specifically used in cases with Eustachian dysfunction and advanced disease like recurrent perforation and tympanic membrane Atelectasis.
REFERENCES
- Gleeson, M.J. (Ed.), Clarke, R.C. (Ed.). Scott-Brown’s otorhinolaryngology: Head And Neck Surgery 7Ed.London:Holder Arnold :2008.III.part19.B.237b.3396
- WHO library cataloguing in-Publication Data Chronic Suppurative otitis media: Burden of illness and management options. Geneva: WHO; 2004. p. 19.
- PL Dingra, Shruti Dhingra, Deeksha Dingra ,Elsevier,a division of Reed Elsevier India Pvt.Ltd.,5th edition 2010,I:2,18.
- A.Julianna Gulya, Lloyd B. Minor, Dennis S. Poe , Glasscock-Shambaugh Surgery of the Ear,6th edition, Peoples’ Medical publishing house.28-466-467
- R. K. Mundra, Richi Sinha, and Richa Agrawal, Tympanoplasty in Subtotal Perforation with Graft Supported by a Slice of Cartilage: A Study with Near 100 % Results, Indian J Otolaryngol Head Neck Surg. 2013 Dec; 65(Suppl 3): 631–635.
- Haitham A. Alnori, Ali A. Muttalib Mohammed, Raghdan M. Alhamdani, Khalid D. Hamad, Temporalis Fascia Versus Cartilage Graft in Myringoplasty,2014 Mar,J Med J 2014; Vol. 48 (2):113- 120.
- Mahmood Shishegar, Abolhasan Faramarzi, and Ayeh Taraghi, A Short-term Comparison Between Result of Palisade Cartilage Tympanoplasty and Temporalis Fascia Technique, Iran J Otorhinolaryngol,2012;24(68): 105–112.
- Tayfun Kirazli, Rasit Midilli, Hearing results after primary cartilage tympanoplasty with island technique, Otolaryngology Head and Neck Surgery, 2995 Jul,132(6):933-7.
- Cabra, Jesús; Moñux, Alfonso, Efficacy of Cartilage Palisade Tympanoplasty: Randomized Controlled Trial, Otology and Neurotology: June 2010 - Volume 31 - Issue 4 - p 589-595
- Kumar Subhanshu, Rohit Sharma, Vinit K Sharma, Temporalis muscle fascia and cartilage palisade technique of type 1 tympanoplasty: A comparison,205,21:3,165-169.