Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Perspective study of bacteriological and antibiotics treatment of maxillary sinusitis in Telangana population
Arun Yellamilli1*, T Mounika2, Chintha Reddy Deepthi Reddy3
1Assistant Professor, Department of ENT, Mamatha Academy of Medical sciences, Bachupally-500090, Telangana, INDIA. 2,3Postgraduate in ENT Mamata Medical College and General Hospital, Khammam, Telangana–507002, INDIA. Email: arunyellamilli@gmail.com
Abstract Background- Maxillary sinusitis (MS) is a quite common infection and inflammation disease in adults. It affects mucosa of nose and PNS. Hence the therapeutic profile of people suffering from sinusitis and its clinical manifestation was studied because exact role of the microbes in the etiology of chronic sinusitis remain uncertain. Method- 92 adult patients aged between 19 to 60 years having complaint of MS were studied. X-ray of PNS and DNE was done to every patient. Antrum lavage was also done and fluid was sent for culture and sensitivity. Routine blood examination, CBC, ESR was also done to study associate clinical scenario. Efficacy of different antibiotics were also noted. Results-The clinical manifestation in MS patients was. 20(21.7%) had pain/ congestion, 11(11.9%) had Nasal blockage, 21(22.8%) had Nasal discharge, 35(38%) had purulence in Nasal cavity on examination, 5(5.14%) had hyposmia or Anosmia. Radiological study had 11 (11.9%) had clear view, 16 (17.3%) had Haziness, 13(14%) had opacity, 24(26%) had air- fluid level, 28(30.4%) had mucosal thickening. The types of fluids were 26 (28.2%) had clear fluid, 6(6.25%) had mucoid, 10(10.8%) had muco- purulent fluid. The efficacy of antibiotics was–90-96% was Amoxicillin clavulanate, 89-92% cefpodoxime, 85-90%, Levofloxacin, 80-88% was ciprofloxacin with Tinidiazole and least adverse effects were observed. Conclusion- The most common organism causing acute MS were S. Aureus, S pneumonia, Enterobacteriacea. H influenza and in chronic MS. Peptosreptococcus (Anaerobic) S. aures, Fusobacterium was observed. And Amoxicillin clavulanate- 90- 96% was effective antibiotic than other antibiotics. Key Word: MS= Maxillary sinusitis, DNE= Diagnostic Nasal Endoscopy, PNS= Para Nasal-air sinus Muco-Purulent, Antibiotics.
INTRODUCTION Para-nasal sinusitis is one of the disadvantages of the erect posture in human beings. Among Para-nasal sinuses maxillary sinuses is wider and large, hence more prone to get infected. It is reported that 15-20% of the population are commonly affected by maxillary sinusitis1. Despite of its prevalence the diseases of maxillary sinusitis (MS) remain with poorly understood origin. Pathogenesis and natural history play vital role. The etiology of chronic MS continues to be the focus of much debate and research in the field of rhinology2. The initial use of antibiotics and agents that, decrease mucosal edema, now surgical methods are employed in whom medical treatment fails. Although diagnostic criteria for acute sinusitis are well established yet the definition of chronic sinusitis is controversial with respect to the importance of bacteria in the initiation and prognosis of diseases chronic sinusitis has been considered to be chronic inflammatory condition rather than microbial infection. The role of bacteria in the pathogenesis of chronic MS is currently being reassessed3. The role of endoscopies has made it possible to determine the microbiology of MS with a lower probability of contamination4. Persistence of infection causes mucosal changes, such alsossofcilia, edema, polyp formation. Hence attempt was done to evaluate the clinical manifestation with radiological study, types of fluid, efficacy of different antibiotics.
MATERIAL AND METHODS 92 patients aged between 25 to 65 years regularly visiting to ENTOPD of Mamata Academy of health sciences, Hospital Bachupally Hyderabad -500090 (Telangana) were studied Inclusive criteria- The patients having clinical features of maxillary sinusitis Such as Nasal obstruction, nasal discharge, post nasal drip, head ache and facial pain, heavy headedness, purulent Secretion in thenasalcavity followed by fever, cough, and malaise were included in the study. Exclusion criteria – children (less than 10 years), pregnancy, lactating mother’s previous history of PNS surgeries, malignancy in PNS Head neck region, immune compromised patients were excluded from the study. Method-Every patient was examined clinically and x-ray of PNS (waters view) and DNE(Diagnostic Nasal Endoscopy) was done and Antrallavage was done, returning fluid was sent for culture and sensitivity, for acute maxillary sinusitis endoscopic guided middle meatus secretion were collected for microbiological examination followed by antral puncture under antibiotic coverage. Routine blood examination and CBC, ESR was also done to study the severity of infection and any associated clinical manifestations. The duration of study is from August 2018 to September2019 Statistical analysis- Various clinical manifestations associated sign and symptoms radiological findings, types of fluid observed, adverse effects of antibiotics were classified with percentage. The statistical data was studied in 2007 SPSS software computer. The ratio of male and females was 2:1. OBSERVATION AND RESULTS Table-1 –Clinical manifestations of maxillary sinusitis was 20(21.7%) had facial pain/ congestion, 11(11.9%) had Nasal obstruction (blockage), 21(22.8%)had nasal discharges(purulentordiscoloredpost-nasaldrip)35(38%)hadpurulenceinNasal cavity on examination, 5(5.43)had hyposmia oranosmia. Table 1: Clinical manifestations of maxillary sinusitis patients
Table-2 –Associated sign and symptoms were- 17(18.4%) had headache (heavy headedness), 19(20.6%) had pyrexia, 13(14%) had halitosis, 10(10.8%) had cough, 22(23.9%) had malaise, 11(11.9%) had dental pain. Table 2: Associated sign and symptoms in maxillary sinusitis patients
Table-3-Radiological study in maxillary sinusitis patients11(11.9%)had clear view, 16(17.3%) had Haziness, 13(14.1%) had opacity 24(26%) had air fluid level, 28(30.4%) had mucousal thickening. Table 3: Radiological study in maxillary sinusitis patients
Table-4- Types of fluid observed in maxillary sinusitis 26(28.2%) had clear fluid 6(6.52%) mucoid, 10(10.8%) had muco- purulent, 50(54.3%) had purulent. Table 4: Types of fluid observed in maxillarysinusitis
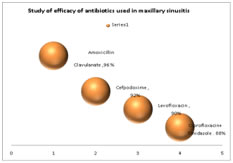
Table-5- Efficacy percentage of Antibiotics – Amoxicillin clavulanate 90-96% cefpodoxime 89-92% levofloxacin 85-90% ciprofloxacin + Tinidazole 80-88 %. Table 5: Study of efficacy of antibiotics used in maxillary sinusitis
Table-6- Study of adverse effects of antibiotics 5(5.43%) diarrhea was observed in Amoxicillin clavulanate 3% diarrhoea was in cefpodoxime 3% Nausea and vomiting, levofloxacin 5% Nausea and vomiting in ciprofloxacin + Tinidazole Table 6: Adverse effects of antibiotics given 92 to patientsof maxillary sinusitis
DISCUSSION InthepresentstudyofBacteriologicalandantibioticstreatmentofMSinTelangana population, the clinical manifestation was – 20(21.7%) Facial pain/ congestion, 11(11.9%) Nasal obstruction (Blockage), 21(22.8%) Nasal discharge purulence or discolored post-nasal drip 35(38%) purulence in nasal cavity on examination, 5(5.43%) Hyposmia or Anosmia, (Tabe-1). Associated sign and symptoms were 17(18.4%) headache, 19(20.6%) pyrexia, 13(14.1%) halitosis, 10(10.8%) cough, 22(23.9%) malaise, 11(11.9%) Dental pain (Table-2) Radiological study was, 11(11.9%) clear view 16(17.3%) Haziness, 13(14.1%) Opacity, 24(26.0%) Air-fluid level, 28(30.4%) mucosal thickening (Table-3) Types of fluid observed in MS was 26(28.2%) clear,6(6.52%) mucoid, 10(10.8%) muco-purulent, 50(54.3%) purulent (Table-4).The efficacy of antibiotics percentage was Amoxicillin+clavulanate 90-96%, cefpodoxime 89-92% levofloxacin 85-90% ciprofloxacin + Tinidazole 80-88% (Table5) the adverse effects of antibiotics were (5.43%) diarrhea in Amoxicillin + clavulanate 5(5.43%) Nausea and vomiting and 4(4.34%) metallic taste observed in ciprofloxacin + Tinidazole(Table-6). The most common organism in acute MS were S. Aureus (18.2%), S. pneumonia (7.60%), Enterobactiraceae(8.2%), H.influenza(5.25%). Anaerobic and S. aureus (10.12) and Fusobacterium (5.98%), Peptostreptococus. SPP (55%), P.acne (18%) and B fragitis (46%) s pyogens (5%) in chronic MS- These findings were more or less in previous studies5,6,7. It is reported that, secretions(Pathogenesis) are harvested in the middle meatus and ethmoid maxillary sinuses hence middle meatus is used in the routine investigation8. Middle meatus drains the anterior ethmoid, frontal and maxillary sinusitis. Hence middle meatusis the central place for bacteriological growth.9 The bacteriological study represents S. Aureus, S. Peptostreptococcus SPP and other negative bacteria. In the radiological study, it was noted that due to asymmetry of the paired sinuses will usually result in the smaller sinus appearing more opaque because of thicker bony wall and little amount of air. Rarely one maxillary sinusfails to develop al together and consequently them axilla looks denser on the plainx-ray film, post–operative changes suchas after Caldwell-luc procedure will also render the maxillary sinus opaque10. Cellulites with swelling of the cheeks produces clouding of the of the antralair space on water’s view and can mimic true clouding due to sinusitis. 90% MS responded to antibiotics and only few of acute complicated MS and chronic MS would require surgical treatment. Antrallavage with saline irrigation of the MS is both diagnostic and therapeutic procedure and is commonly performed in the chronic MS. It is an invasive procedure and is not without hazards11. The risk of membrane perforation increases, when anatomical variations are present such as maxillary sinus septum is present12. Hence radiological study plays vital role in invasive procedure in MS.
SUMMARY AND CONCLUSION In the present study of bacteriological and antibiotics, treatment in maxillary sinusitis. The commonly observed organisms are S. aureus, S pneumonia, Enterobacteriacae and common anaerobic are peptostreptococcus, The amoxicillin + clavulanate antibiotic has proved efficient to treat MS and radiological study is ideal way for invasive procedure were in chronic MS. But this study demands further pathophysiological, microbiological, genetic, nutritional, immunological study because exact pathogenesis of chronic MS is stillunclear. This research paper was approved by Ethical Committee of Mamatha Academy of Medical sciences, Bachupally-500090 (Telangana)
REFERENCES
|
|
 Home
Home