Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Outcome of reduction of hypertrophied inferior turbinate during septoplasty
Sushant Kumar1*, M K Bose2
1Senior Resident, Associate Professor2, Department of ENT, Darbhanga Medical College and Hospital, Bihar, INDIA Email: sushant.28@gmail.com
Abstract Deviated nasal septum towards one side is often associated with overgrowth of inferior turbinate, which occupies expansive space on contralateral nasal cavity. It is assumed that this counter balanced mechanism characterised by compensatory hypertrophy originates to protect the more patent nasal side from excess airflow with its drying and crusting effects. septoplasty alone can treat nasal obstruction in patients with deviated nasal septum ,to know whether hypertrophied turbinate needs to be addressed in patients with deviated nasal septum. And also to know the effectiveness of reduction of hypertrophied turbinate together with septoplasty for the treatment of nasal obstruction in patients with deviated nasal septum. Methods: It was prospective randomised clinical study based on nasal obstruction symptom evaluation scale (NOSE) for patient subjective evaluation of symptoms. 60 patients with septal deviation and contralateral inferior turbinate hypertrophy were recruited in the study. Study was conducted in the department of ENT, Darbhanga Medical College and Hospital during the period of 2018-2019. Results: The results of study showed that both following septoplasty and TRS post operative results were highly significant but among these two groups, patient who underwent septoplasty along with TRS had better result. Among different type of TRS Turbinectomy has the best results. Conclusion: we conclude that hypertrophied turbinate needs to be addressed in chronic cases of nasal obstruction with deviated nasal septum and contralateral turbinate hypertrophy. And in these patient TRS should be done in addition to septoplasty. Hypertrophied Turbinate reduction in addition to septoplasty are highly effective modality for the treatment of nasal obstruction in patients with deviated nasal septum. NOSE score can be used as an objective tool for symptomatic measurement of patients with nasal obstruction. Nasal spirometry can be used for objective measurement of nasal patency. Key Word: hypertrophied inferior turbinate.
INTRODUCTION Nasal obstruction is a common presenting symptom which an otorhinolaryngologists encounters in daily clinical practice. It affects 9.5-15% of general population.1There can be many etiology for chronic nasal obstruction like deviated nasal septum with or without turbinate hypertrophy, only turbinate hypertrophy, allergic rhinitis, vasomotor rhinitis, infective rhinitis, nasal polyposis, granulomatous disease or nasal tumours, adenoid hypertrophy.2,3 Among these etiology for nasal obstruction one of the most commonest is deviated nasal septum.2 Deviated nasal septum towards one side is often associated with overgrowth of inferior turbinate, which occupies expansive space on contralateral nasal cavity. It is assumed that this counter balanced mechanism characterised by compensatory hypertrophy originates to protect the more patent nasal side from excess airflow with its drying and crusting effects. The turbinates hypertrophy can be due to mucosal element or bony expansion.3,4 Many authors believes that once septoplasty is done compensatory hypertrophy regresses on its own.5 Inferior turbinate hypertrophy due to rhinitis is amenable to medical treatment. However long standing chronic cases associated with nasal septal deviation may become irreversible. This may be due to dilated submucosal venous sinuses becoming varicose and unresponsive to sympathetic stimulation or medical treatment or because of fibrosis or because bony expansion of turbinates. As such these patients are refractory to medical management and complains of persistent symptoms.6,7 Despite its well known clinical occurrence this intriguing phenomenon has received little attention in the literature. Furthermore, the available studies lack quantative and qualitative information regarding the composition and typical histological features of hypertrophic turbinate compared to normal ones. Likewise, there are not enough studies or data to substantiate whether these changes are permanent or reversible. Many otorhinolaryngologists perform septoplasty with or without turbinate reduction surgery and surgical methods relies largely on clinical judgement, as the effectiveness of procedure is relatively unknown, the indications and technique applied vary considerably.
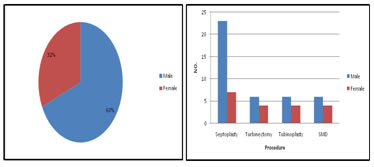
METHODS Source of data: Patients presenting to ENT outpatient department of A J Institute of Medical Sciences Mangalore. Inclusion criteria: All patients above 18years of age presenting to ENT outpatient department with history of nasal obstruction for at least 3months and clinically diagnosed to have deviated nasal septum with inferior turbinate hypertrophy. Exclusion criteria: Patients with nasal obstruction diagnosed to have allergic rhinitis, vasomotor rhinitis, infective rhinitis, nasal polyps, granulomatous disease or nasal tumors or those patients unfit for surgery. Method of collection of data: 60 patients with septal deviation and contralateral inferior turbinate hypertrophy were recruited in the study. Detailed history and clinical examination was done. After taking informed consent, Patients were asked to fill questionnaires relating to severity of their symptoms using Nasal Obstruction Symptom Evaluation(NOSE) scale. Patients were then randomly divided into two groups. In group A, reduction of inferior turbinate was performed to treat hypertrophied inferior turbinate together with septoplasty. In group B, only septoplasty was done. Post-operative patient's symptoms were again evaluated using Nasal Obstruction Evaluation Scale (NOSE) at 1, 3 and 6 months. Nasal airway was objectively evaluated using nasal spirometry. Data was analysed using tables, graph, percentage. And test of significance like paired t-test, student t-test, one-way anova was used. SPSS Microsoft software version.16 was used for test of analysis. Nose Score- Used for subjective measurement of symptoms- Scores taken pre-operatively,1month post-operatively,3months post-operatively,6months post-operatively. Total 5 symptoms, each symptoms is given points from 0 to 4 depending on severity of symptom.0 minimum severity,4-maximum severity. So total maximum points 5x4=20. Total point=Q1+Q2+Q3+Q4+Q5.This is divided by 20 and multiplied by 100,to get score out of 100.i.e Total Score= Q1+Q2+Q3+Q4+Q5x100 20 Total score from 0 to 100. 0-minimum severity 100- maximum severity. Change in pre to post operative at 1, 3 and6 months is compared between group Ai. eSeptoplasty + TRS and group B-Septoplasty only. Each group consists of 30 patients. Among TRS+ septoplasty group further subdivided into 3 groups of 10 each undergoing SMD+ Septoplasty,Turbinoplasty+septoplasty,Turbinectomy+septoplasty. Different TRS are compared among themselves. Nasal Spirometry-used for objective measurement of the nasal obstruction .It was done pre-operatively,1month post-operatively,3months post-operatively. SPIROMETRY APPARATUS Modified Endotracheal tube. Objective assessment of nasal patency was done using Spirometry apparatus in the pulmonary medicine department. Endotracheal tube (ET) was used to check the patency in each nostril by ET of size No.8 alternatively. The mouthpiece of the spirometer and the endotracheal tube were connected by using an air-tight seal light body condensation silicone prosthetic material. RESULTS Figure 1: Sex distribution; Figure 2: Sex Distribution For different surgeries
Table 1: Mean NOSE Score
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 2: Mean Changes In Nose Score
symbol * and ** indicates significant values at p<0.05 and p<0.01
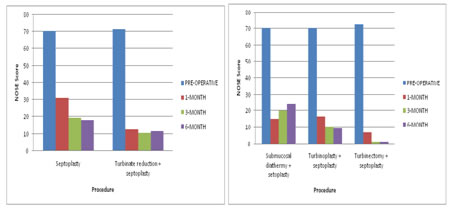
Figure 3: Mean NOSE score Septoplasty VS TRS+Septoplasty Analysing patient symptomatic improvement using NOSE score following observations were made (table1andtable2):
From above observation we can conclude both following septoplasty surgery alone andthose undergoing TRS with septoplasty had highly significant post-operative improvement (p<0.001) at 1month and 3monthsand6months There was highly significant (p<0.001) difference in patients undergoing combined TRS and septoplasty to those undergoing septoplasty alone at post-op 1and 3months with difference of19.5 and 10.17 respectively. Significant difference was observed at 6months with difference of 7. So patients undergoing TRS with septoplasty has more symptomatic relief compared to those undergoing septoplasty alone. But the difference which was significantly higher at immediate post-op1 month of 19.5 which was reduced to 10.17 at 3months and 7.5 at 6months, which was however still significant So patients undergoing septoplasty alone gradually shows symptomatic improvement over the period of 6month,whereas patient undergoing septoplasty with turbinate reduction definitely had overall greater improvement symptomatically compared to septoplasty alone, but their high post-op improvement remained static and did not improve over the period. Comparing data among turbinate reduction surgeries-
Patients undergoing submucosal diathermy together with septoplasty had similar symptomatic improvement compared to those undergoing turbinoplasty along with septoplasty at 1month with minimal difference of 1.5 in favour of SMD, but when compared to patient undergoing turbinectomy together with septoplasty ,they had less improvement with significant difference of 10 (P<0.05) in favour of patient undergoing turbinectomy with septoplasty. But in patients undergoing SMD improvement gradually decreases over a period of 6months with change in score of 50.5 and46 respectively at 3 and 6months, scoring value of which was 5 and 9 less compared to 1st month. So patients undergoing SMD had maximum improvement at 1month and then the symptoms detoriated at 6month but still they had significant improvement in NOSE score at 6months. Patients undergoing turbinoplasty with septoplasty has showed slight gradual improvement over 6months which was 14.5 greater than SMD with septoplasty and9.5 less than those undergoing turbinectomy with septoplasty at 6month. Patients undergoing turbinectomy with septoplasty had highest improvement in NOSE score compared among all 3 turbinate surgeries with difference of 10 and 11.5 scoring value at 1month compared to SMD +septoplasty and turbinoplasty+septoplasty, which gradually over 6month showed significantly (p<0.05) greater difference of 25 compared to SMD+septoplasty. And almost static difference of 9.5 compared to turbinoplasty+septoplasty. Compared to mean among these 3 TRS it has 11.17 point difference: So we can conclude maximum symptomatic relief is provided by patient undergoing turbinectomy+septoplasty and minimum with SMD+septoplasty.
Table 3: Mean Symptom-wise NOSE score-Septoplasty
symbol* and** indicates significant values at p<0.05 and P<0.01
Table 4: Mean Symptom-wise NOSE score -Turbinate Reduction
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 5: Mean Symptom-wise Change in NOSE score-Septoplasty
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 6: Mean Symptom-wise Change in NOSE score-Turbinate Reduction
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table7: Mean Symptom-wise NOSE score-Turbinectomy
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 8: Mean Symptom-wise NOSE score-Turbinoplasty
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 9: Mean Symptom-wise NOSE score-Submucosal Diathermy
Table 10: Mean Symptom-wise Change in NOSE score-Turbinectomy
symbol * and ** indicates significant values at p<0.05 and p<0.01 Table 11: Mean Symptom-wise Change in NOSE score-Turbinoplasty
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 12: Mean Symptom-wise Change in NOSE score-Submucosal Diathermy
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 13: FEV-1 Comparison
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 14: Change FEV-1 Following Surgery
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 15: Finfv comparison
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 16: Change FINFV Following Surgery
symbol * and ** indicates significant values at p<0.05 and p<0.01 FINFV
Table 17: MVV Comparison
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 18: Change MVV Following Surgery
symbol * and ** indicates significant values at p<0.05 and p<0.01
MVV
Table 19: Comparison in Mean change in NOSE score with change in FEV-1
symbol * and ** indicates significant values at p<0.05 and p<0.01 Table 20: Comparison in Mean change in NOSE score with change in FEV-3
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 21: Comparison in Mean change in NOSE score with change in FINFV
symbol * and ** indicates significant values at p<0.05 and p<0.01
Table 22: Comparison in Mean change in NOSE score with change in MVV
symbol * and ** indicates significant values at p<0.05 and p<0.01\ DISCUSSION Nasal obstruction is one of the most common complaints by patient which an otorhinolaryngologists encounters in day to day practice. It’s affecting 9.5-15% of general population1.Nasal septum deviation and associated turbinate hypertrophy is one of its most frequent causes. The present study was carried out to know whether septoplasty alone can treat nasal obstruction in patients with deviated nasal septum, to know whether hypertrophied turbinate needs to be addressed in patients with deviated nasal septum. And also to know the effectiveness of reduction of hypertrophied turbinate together with septoplasty for the treatment of nasal obstruction in patients with deviated nasal septum. In this study NOSE score was used for subjective evaluation and nasal spirometry for evaluating objectively. The present study showed highly significant result for post operative improvement for both septoplasty and septoplasty + turbinate reduction. According to NOSE score patients undergoing TRS with septoplasty has more symptomatic relief compared to those undergoing septoplasty alone. Patients undergoing septoplasty alone gradually shows symptomatic improvement over the period of 6months, whereas patient undergoing septoplasty with turbinate reduction definitely had overall greater improvement symptomatically compared to septoplasty alone, but their high post-op improvement remained static and does not improved over the period but at 6 month it was still significantly greater than septoplasty alone. The results of our study is concomitant with majority of studies which favours TRS in addition to septoplasty. The study by Devseren N, Ecevit MC, Erdag TK, Ceryan Kin 2010-11 on 42 patients with deviated septum and compensatory contralateral turbinate hypertrophy ,concluded that the subjective symptoms were better in patients undergoing TRS in addition to septoplasty, in this study acoustic rhinometry and rhinomanometry tests were conducted for an objective evaluation of nasal patencyanda visual analog scale (VAS) was applied for the subjective evaluation of nasal obstruction complaints8. In a study done by Jun BC J, Kim SW, Cho JH, Park YJ, Yoon HR in St.Mary’s hospital ,South Korea computed tomography of sinuses of 20 patients was done, the volume of the inferior turbinate was measured from the three-dimensional reconstruction, it was concluded that, the inferior turbinate on the concave side had a significantly greater volume and hence septoplasty and concomitant inferior turbinate surgery to manipulate conchal bone and soft tissues are necessary for treatment of those patients with unilateral nasal septal deviation and compensatory hypertrophy of the contralateral inferior turbinate9. In a study done by Gilead Berger, lan Hammel, Rachel Berger, Shabtai Avraham, Dov Ophir to know the histopathology of inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum, it was found that , the inferior turbinate bone underwent a twofold increase in thickness, result supported the decision to excise inferior turbinate bone at time of septoplasty because of significant bony expansion and relative minor role of mucosal hypertrophy4. But in another study by P. Illum, No influence of turbinate surgery was detectable11.In a study done by Nunez DA, Bradely also showed Contralateral inferior turbinectomy does not add to the relief of nasal obstruction beyond that attained by septal surgery in these patients13. The study by Stewart et.al also has used NOSE score for subjective evaluation, as was used in our studyand they concluded, in patients with septal deformity, nasal septoplasty results in significant improvementin disease-specific quality of life, high patients satisfaction, and decreased medication use11. Similar to majority of above mentioned studies our study also conclude that TRS in addition to septoplasty offers greater symptomatic relief compared to those undergoing septoplasty alone. Other studies where no significant improvement was found when TRS was added to septoplasty are in favour of longer follow up. Similar to present study, according to Stewart et.al NOSE score can be used for subjective measurement of nasal obstruction, which can be used for pre to post operative improvement and also for comparison among different surgeries. In a study by Jones AS, Wight RG, Kabil Y, Buckingham E, It has been suggested that submucosal diathermy would not be effective in a group of patients developing hypertrophic rhinitis where the nasal submucosal is infiltrated with fibrous tissue rendering it incapable of decongestion .This may be due to fibrosis. In a study by J Richardson ,it was concluded that long standing swelling may become irreversible. This may be due to dilated submucosal venous sinuses becoming varicose and unresponsive to sympathetic nervous system stimulation or medical treatment7. In a study by Jones and Lancer showed that although submucosal diathermy provides good relief from nasal obstruction in the short term, but if patients who do not have concurrent medical treatment in most the inferior turbinates rehypertrophy within15 months and subjective obstruction returns14. In a study Wight, Jones and Clegg showed anterior trimming of the inferiorturbinate, whilst being an objective success in decreasing nasal resistance, frequently failed to produce a significant fall in subjective obstruction in the first 2 months15.In a study by Mabry in 1982,He found the major difference between total turbinectomy and inferior turbinoplasty was the flap of tissue left behind in the latter procedure to form a neoturbinate. He postulated the functional difference in the two procedures is explained by the presence of the inferior neoturbinate acting as a baffle to preserve a more normal airflow16. In a non-randomised trial of inferior turbinoplasty and septoplasty versus septoplasty alone Hilberg et al.found that two-thirds of patients who underwent contralateral turbinoplasty plus septoplasty reported satisfaction with the patency of the nasal cavity that had hadturbinate hypertrophy whereas none who underwent septoplasty alone reported satisfaction with the patency of this nasal cavity17. In Hooper RC study individuals with and without nasal symptoms underwent forced inspiratory nasal flow–volume (FINFV) curve measurements. Similar to this study FINFV was used as one of nasal spirometry parameter18. Moore M and Eccles R study reviews why there is no normal range of nasal patency available when assessing nasal obstruction and also the factors that influence nasal patency they concluded population is better defined with nasal anthropometric measures such as nasal index. In our present study also, we could not detrmined normal range of nasal spirometry parameters, as it varies on size of nasal cavity which is different for different individual and depends on age ,sex, height, weight, race. And to find out normal range we have to stratify into groups depending upon above factors and probably a larger sample size is required for significance19. In another study by Moore M. andEccles, they reviewed on the objective evidence for the efficacy of surgical management of the deviated septum. They concluded that septal surgery improves objective measures of nasal patency and that improved nasal airflow20. Fyrmpas G, Kyrmizakis D, Vital V and Constantinidis J studied the role of bilateral simultaneous nasal spirometry (BSNS) in the preoperative selection of patients for septoplasty. They concluded that, this test offers valuable information along with clinical assessment of the nasal airway in the preoperative assessment of candidates for septoplasty when other objective methods are not available21. In a study by Harar R, Kalan .A, Kenyon.G, the reproducibility of nasal spirometry was assessed, concluded that FEV1 as their derived variables of flow-volume loops can be used in the assessment of nasal patency. In our present study also FEV-1 was used as one of the nasal spirometry parameter22. Similar to our study the above mentioned studies shows that nasal spirometry can be used as effective ,simple tool for measuring nasal patency in patient with complaints of nasal obstructionand can be used for comparing results pre to post operative improvement and hence for comparing objective improvement among different types of surgery, finally to conclude which modality of surgery is better. In our study we concluded TRS when done in addition to septoplasty has better objective improvement as measured by nasal spirometry. The present study proved that although both groups of patient i.e those undergoing septoplasty alone and those undergoing TRS in addition to septoplasty had highly significant post –operative improvement. But those undergoing TRS had the best result, hence TRS should be done in addition to septoplasty and turbinectomy is the best modality among TRS. This study also showed the correlation between both symptomatic and objective improvement as assessed by NOSE score and nasal spirometry respectively. In a study by Fairley JW, Durham LH, Ell SR also showed subjective sensation of nasal patency is strongly correlated with objective nasal patency. The present study results are comparable to previously published data. However longer follow up, larger sample size can be considered for further studies.
CONCLUSION The results of study showed that hypertrophied turbinate need to be addressed in chronic cases of nasal obstruction with deviated nasal septum and contralateral turbinate hypertrophy. And in these patient TRS should be done in addition to septoplasty.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home