Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Turbinectomy In Chronic Inferior Turbinate Hypertrophy- A Safe Surgical Alternative
Roshan Marie Thomas1, Jishana Jamaldeen2*, Mary Kurien3, Shilpa Divakaran4
1Cochin Hospital, Kochi, Kerala, INDIA. 2,3Department of Otorhinolaryngology, Pondicherry Institute of Medical Sciences, Pondicherry, INDIA. 4Specialist ENT Surgeon, New Medical Centre, New Medical Centre Hospital, WAY 4202, MBD EAST RUWI, Muscat, OMAN. Email: jishana.j@gmail.com
Abstract Background: Inferior turbinate hypertrophy due to various diseases is a common cause of troublesome nasal symptoms. Turbinectomy has been widely used in patients who are refractory to medical management. We aimed to describe the outcomes following turbinectomy for inferior turbinate hypertrophy. Methods: This was a descriptive observational study on 70 patients with symptomatic inferior turbinate hypertrophy admitted to Pondicherry Institute of Medical Sciences. All patients underwent diagnostic nasal endoscopy and responded to the Sino-Nasal Outcome Test (SNOT) questionnaire prior to and at 1, 3 and 12 weeks following turbinectomy for determining the changes in symptoms and quality of life as a result of the procedure. Results: Majority (78%) of the patients were male. The most common cause for inferior turbinate hypertrophy was allergic rhinitis (88%). All patients had improvement in symptoms following turbinectomy at 1, 3 and 12 weeks as evidenced by significant change in the overall SNOT score from 56.3 (SD – 17.06) to 16.09 (SD – 12.30). There was also significant improvement in the quality of life of all patients. Crusting was present in 92.8% at 1 week following surgery; however, at 12 weeks none had crusting. At 12 weeks, 97.7% of patients had patent airway. Conclusion: Inferior turbinectomy is a safe and reliable technique for patients with chronic inferior turbinate hypertrophy refractory to medical management. Key Word: inferior turbinate, turbinectomy, turbinoplasty, allergic rhinitis, SNOT 22.
INTRODUCTION Inferior turbinate hypertrophyis a common cause of nasal obstruction affecting the patient’s quality of life. Different diseases of the nose are responsible for inferior turbinate hypertrophy, altering the nasal physiology such as perennial allergic rhinitis, vasomotor rhinitis, chronic hypertrophic rhinitis and rhinitis medicamentosa. Turbinate enlargement in these patients is usually bilateral and is caused by thickening of mucosa with or without hypertrophy of the underlying structures. Chronic inflammation of nasal mucosa causes irreversible changes in structure of the turbinate leading to deposition of collagen in the submucosal tissue or bone remodelling. Medical and surgical treatments have been used to relieve these symptoms. However, many patients are refractory to medical treatment and nasal obstruction prevails due to dilatation of venous sinuses or fibrosis. In such cases surgical approach is recommended. Several surgeries like partial or total inferior turbinectomy, submucosal resection, submucosal diathermy, inferior turbinoplasty, laser turbinectomy and radiofrequency ablation have been widely used, each with merits and limitations. Turbinectomy is very commonly employed among these. However, the outcomes following turbinectomy have not been consistent across studies.1,2 This study was undertaken to evaluate the outcome of turbinectomy in relation to relief of nasal obstruction and other associated symptoms.
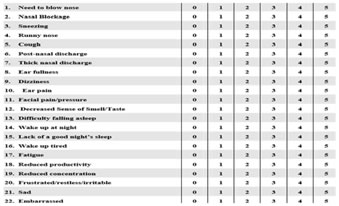
METHODOLOGY This was a descriptive study conducted in the Department of Otorhinolaryngology at the Pondicherry Institute of Medical Sciences, a tertiary care teaching hospital, between October 2014 and April 2016. Seventy adults with symptomatic inferior turbinate hypertrophy secondary to perineal allergic rhinitis, vasomotor rhinitis and rhinitis medicamentosa and chronic hypertrophic rhinitis who were not responsive to medical management for at least 4 weeks were included in this study. Patients with asymptomatic turbinate hypertrophy, acute respiratory infections, associated gross septal deviations, nasal polyposis with or without chronic rhinosinusitis, tumours of the nose and paranasal sinuses and associated comorbid conditions like uncontrolled diabetes, bleeding diathesis were excluded. Approval from the institute ethics and research committee was obtained (IEC: RC/14/71). After obtaining informed written consent, complete history was obtained and patient sunder went thorough ENT examination. Symptom severity and quality of life were assessed using the Sino-Nasal Outcome Test 22 (SNOT 22) (Figure 1). This is a simple, subjective questionnaire which comprises 22 questions with symptoms scoredon a scale of 0-5 (0 being no problems and 5 being maximal problems). All patients underwent a preoperative diagnostic nasal endoscopy to assess the size of turbinate and severity of obstruction and also to rule out other nasal pathologies. Routine blood investigations like complete blood count, urine routine, blood glucose levels, blood urea, serum creatinine, coagulation profile and serology were done. All patients underwent inferior turbinectomy under general anaesthesia. In turbinectomy, a curved haemostat was placed over the turbinate and clamped following which resection was done. Haemostasis was achieved by regular anterior nasal packing. Post operatively all patients received oral antibiotics and analgesics. All patients were discharged on day 2 following nasal pack removal. Patients were followed up at the end of 1 week, 3 weeks and 12 weeks for subjective improvement of symptoms, with the help of SNOT 22, clinical examination and objective assessment by diagnostic nasal endoscopy at all 3 visits. Size of turbinate, haemorrhage, infection, crusting, synechiae formation or any other complications related to surgery were observed. Nasal patency was assessed by cold spatula test and cotton wool test.
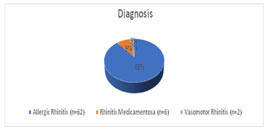
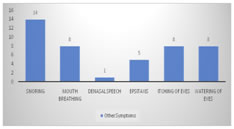
Figure 1: Sino-nasal Outcome test (SNOT 22) used for the assessment of symptoms severity and quality of life in this study3. RESULTS Of the 70 patients in this study, 50 (78%) were males and 20 (22%) were females. 37 (52.8%) of patients were between 18 to 30 years of age. 62 out of 70 (88.6%) patients had allergic rhinitis while 6 out of 70 (8.6%) patients had rhinitis medicamentosa (Figure2). All 70 patients had nasal obstruction as the predominant symptom. 51 (72.9%) patients had bilateral nasal obstruction. Figure 2 Figure 3 Figure 2: Causes of inferior turbinate hypertrophy among the patients (n = 70). 14 (20%) patients had snoring and8 (11.4%) patients complained of mouth breathing (Figure3); Figure 3: Distribution of symptoms among the patients with inferior turbinate hypertrophy (n = 70).
The baseline nasal endoscopy findings are summarised in table 1. Table 1: Nasal endoscopy findings at the beginning of study (n = 70).
Analysis of symptoms by SNOT 22: The mean score of patients who complained of persistent need to blow nose prior to surgery was 3.37 (SD – 0.80). Following surgery this reduced to 2.785, 2.02 and 1.34 at one week, three weeks and 12 weeks respectively. The pre opmean score for sneezing prior to surgery was 3.14. The post-operative scores at 1, 3 and 12 weeks were 2.51, 1.83 and 1.04 respectively. This change in symptom score after surgery was statistically significant (p< 0.001). Table 2 depicts the pre and post-operative symptom scores pertaining to other common problems such as cough, post nasal drip and thick nasal discharge associated with turbinate hypertrophy. All changes were statistically significant. Table 2: Mean scores of cough, post-nasal drip and thick nasal discharge among patients pre-operatively and at 1, 3 and 12 weeks post-operatively.
Analysis of Quality of Life Symptoms: To evaluate quality of life, we used the following parts of the SNOT 22 questionnaire: difficulty falling asleep, waking up at night, lack of good night’s sleep, waking up tired, fatigue, reduced productivity, reduced concentration, feeling sad, restlessness and feeling embarrassed. Individual components of this quality of life section also showed statistically significant improvement from baseline following surgery at 1, 3 and 12 weeks (Table 3). Analysis of overall SNOT 22 score: In the preoperative subjective assessment of SNOT score, the mean total score was 56.3 (SD – 17.06). Following surgery the SNOT score values reduced significantly to 41.13 at one week, 27.24 at 3 weeks and 16.09 at 12 weeks. All patients had significant reduction in SNOT score at the end of 3 months. Serial Endoscopy Findings: Follow up nasal endoscopy showed that one week following surgery, most patients had crusting (92.8%). Dried blood stains were seen in 20 patients. Synechiae were noticed in 11.4% of cases following surgery. At three weeks postoperatively, crusting had reduced to 77.1%. Mucoid discharge was found in 31.4 % of cases. Synechiae was seen in 5 patients while 31 patients had patent airway. Twelve weeks following surgery, 97.7% of patients has patent airway, synechiae was seen in 3 patients (4.2%). Some patients had mucopurulent secretions (2.8%) and others had mucoid discharge (17.1%). Table 3: Scores on SNOT 22 for the symptoms related to quality of life of patients before and at 1, 3 and 12 weeks after surgery (n = 70).
DISCUSSION Nasal obstruction secondary to inferior turbinate hypertrophy is mostly due to allergic rhinitis. It significantly affects the quality of life4. The treatment of choice varies from oral anti-histamines, oral or topical decongestants, oral or topical steroids. In many patients medical therapy alone fails to achieve symptomatic relief and in such patients surgical therapy is advocated4. Since the beginning of the 19th century, over 13 techniques have been described for surgical management of inferior turbinate hypertrophy5. Hartmann was one of the pioneers of turbinate surgery.6 Various techniques are practised all over the world. Major aetiologies of inferior turbinate hypertrophy in our patientswere allergic rhinitis, vasomotor rhinitis and rhinitis medicamentosa. This pattern is comparable with other studies5, 7,8.Most patients in our study aged from 18 to 60 years, majority of them being between 18 to 30 years. Baig M et al also reported that majority of such patients were in the age group of 10 to 30 years7 Descriptive studies such as those done by Ophir et al9 showed that 80% of patients reported improvement in nasal breathing following surgery. A recently conducted study by Gomaa et al10 also showed dramatic improvement in nasal obstruction in as less as two weeks following inferior turbinectomy. In this study of 70 patients with symptomatic inferior turbinate hypertrophy, we noted that all patients had nasal obstruction as the major complaint. Most of them had bilateral obstruction, and many had diurnal variation of symptoms. There was a significant improvement in the symptom severity in all patients following turbinectomy as evidenced by the changes in mean scores for individual symptoms as well as overall score of the SNOT 22 questionnaire. Besides, the quality of life of all patients at 1, 3 and 12 weeks showed a remarkable improvement from baseline. Studies such as those by Fradis et al11 showed that 10 % of patients had crusting following surgery. In contrast, a study conducted by Mathai J in 2004 concluded that none of the patients had crusting when followed up to 2 years following inferior turbinectomy8. Percadoni et al also documented similar results on children after turbinectomy12. In our study, post operatively, at one week following surgery, about a quarter of the patients had dried blood in nasal cavity while 92.8% had crusting which reduced to 77.1% at three weeks. The crusts were cleared using endoscopic assisted suctioning and patients were also started on nasal douching. At the end of 12 weeks none of the patients had crusting. Rakover Y et al compared inferior turbinectomy with cryosurgery which showed that 100 percent of cases had no crusting following turbinectomy. In this study, good functional results were seen in 77% of patients following inferior turbinectomy as compared to cryosurgery (35%) over long term follow up13. In our study, synechiae was seen in 11.4 % of the patients at one week following surgery. These patients underwent synechiae release as an outpatient procedure at the third week of follow up by suction clearance and placement of gel foam between synechiae. At the end of 12 weeks, 4.2% of the cases had minimal, persistent synechiae. The study by Mathai J also had a similar outcome with 3% of patients having synechiae at routine follow up8. In our study, post-operative patent nasal airway was noted in 44.2% and 97.7% patients at three weeks and 12 weeks respectively. In contrast, Saleem M et al on his series of patients reported that 84 % of patients had patent airway at two weeks post operatively14.Our study like the study done by Ophir et al refutes the fact that inferior turbinectomy leads to the formation of atrophic rhinitis.9 The overall success rate of inferior turbinectomy for inferior turbinate hypertrophy in our study of 70 patients was 100% both in terms of SNOT score and individual scores. In another study conducted by Talmon et al on 357 patients over a 6 year period, it was concluded that even in a hot and dusty climate, total inferior turbinectomy is an effective and safe procedure15. Faulcon et al in their retrospective analysis of 50 patients who underwent inferior turbinectomy after 24 months of follow up reported no cases of atrophic rhinitis, with 80 % improvement in breathing, good nasal re-permeabilization with significant reduction of rhinorrhoea and post nasal drip16. Serrano E et al showed that after a follow up of one year, 81.7% of patients had improved by surgical intervention17. Baig et al in their study on 116 patients reported superior results following inferior turbinectomy as compared to submucus diathermy (94.7% vs 75%)7. A computational study that uses virtual surgery to investigate the changes in aerodynamics follow turbinate surgery showed that inferior turbinectomy yields good increase in nasal airflow17. Our study has noted that inferior turbinectomy is a relatively simple and reliable surgical technique for the treatment of inferior turbinate hypertrophy. Its benefits include being an inexpensive technique with short learning curve and lack ofserious complications such as atrophic rhinitis. Its proven advantage is its long-term results unlike other techniques. Disadvantages may include bleeding at the time of surgery (controlled by routine nasal packing that follows rhinology surgeries) and synechiae formation which is seen in other procedures as well. Studies conducted to date provide insufficient evidence to adopt an ideal measure for turbinate reduction. Some reasons for this include combination of allergic and non-allergic patients and non-randomised distribution of patients into groups. There is an urgent need for randomised control trials to evaluate the role of inferior turbinate surgery in the treatment of chronic inferior turbinate hypertrophy that is refractory to medical treatment. Rigorously designed study that includes subjective and objective measurements with control groups and long term follow up must be considered. In addition, selecting a particular technique need to take into account the experience of surgeon and informed patient choice.
CONCLUSION We conclude that turbinectomy for inferior turbinate hypertrophy is an effective, simple and relatively safe procedure as evidenced by significant relief of all symptoms postoperatively. It can also improve the quality of life of patients with symptomatic inferior turbinate hypertrophy.
REFERENCES
|
|
 Home
Home