Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Tubercular lesions in otorhinolaryngology
Anchal Gupta1*, Padam Singh Jamwal2
1Senior Resident, 2Professor, Department of ENT, Head and Neck Surgery, SMGS Hospital, Government Medical College, Jammu, Jammu and Kashmir, INDIA. Email: anchalsachit@gmail.com
Abstract Background: Tuberculosis constitutes the major burden of diseases in India. Materials and methods: The current study was conducted at Department of ENT, SMGS Hospital, Government Medical College, Jammu, from October 2017 to March 2019. This was a retrospective study of diagnosed cases of extrapulmonary tuberculosis which included patients of all age groups and both the sexes. The patients with signs and symptoms suggestive of TB of otorhinolaryngeal region underwent thorough clinical examination. Detailed history was taken from all the patients. Endoscopic evaluation was done in required cases. Appropriate investigations such as serological tests and tests to confirm the diagnosis of tuberculosis were carried out including a Fine Needle Aspiration Cytology or biopsy as required in the case. Pulmonary tuberculosis was ruled out by careful history, examination and investigations. Results: 40 patients who visited the ENT and Head Neck Surgery department of our institute with otorhinolaryngologic manifestations of tuberculosis were studied. There were 19 male and 21 female patients. Majority of the patients presented with tuberculous cervical lymphadenopathy i.e. 28(70%) patients. Of these 12(42.85%) were males and 16(57.15%) were females. Tubercular laryngitis was seen in 5(12.5%) patients. Interarytenoid area was most commonly involved seen in 3(60%) patients followed by epiglottis seen in 1(20%) patient and vocal cords seen in 1(20%) patients. Tubercular retropharyngeal abscess was seen in 3(7.5%) patients. Tubercular otitis media was seen in 3(7.5%) patients Tubercular infection of preauricular sinus was seen in 1(2.5%) patient. All the patients after confirmation of diagnosis were started on anti tubercular therapy and showed good response to treatment. Drugs used were isoniazid, ethambutol, rifampicin and pyrizinamide. Conclusion: Early diagnosis and treatment of tuberculosis can reduce the morbidity and mortality associated with the disease. Key Words: Fine needle Aspiration Cytology, lymphadenopathy, tuberculosis.
INTRODUCTION Tuberculosis (TB), one of the oldest diseases in man, is, even today, a leading cause of human suffering and loss of life.[1] Tuberculosis, a chronic inflammatory bacterial infection caused by Mycobacterium tuberculosis is a common disease especially with increasing incidence of AIDS and HIV infestation. Tuberculosis is known to affect almost every organ in the body, and it should be a concern of each and every medical practitioner .Though pulmonary tuberculosis remains the commonest manifestation of the disease, incidence of extrapulmonary tuberculosis is approximately 20% with tuberculous lymphadenopathy being the commonest one in children and pleural tuberculosis being the commonest extrapulmonary manifestation in adults.2,3 In the ear, nose, and throat (ENT) area specifically, the most frequent location is the cervical lymph nodes, involving approximately 95% of the cases. The remaining locations (such as larynx, ear, nostrils, pharynx, tonsils, mastoids, salivary glands or cavum) each represent less than 1% of all the TB cases.4 The diagnosis of TB is mainly based on a positive mycobacterial smear and culture or the histopathological presence of a chronic/ caseating granuloma. Since there are number of differential diagnoses to a clinical presentation of tuberculosis of the otorhinolaryngeal region, the present study was undertaken to assess the incidence and different manifestations of TB of ear, nose and throat in patients.
MATERIALS AND METHODS The current study was conducted at Department of ENT, SMGS Hospital, Government Medical College, Jammu, from October 2017 to March 2019. This was a retrospective study of diagnosed cases of extrapulmonary tuberculosis which included patients of all age groups and both the sexes. The patients with signs and symptoms suggestive of TB of otorhinolaryneal region underwent thorough clinical examination. Detailed history was taken from all the patients. Endoscopic evaluation was done in required cases. Appropriate investigations such as serological tests and tests to confirm the diagnosis of tuberculosis were carried out including a fine needle aspiration cytology or biopsy as required in the case. Pulmonary tuberculosis was ruled out by careful history, examination and investigations. Clinical presentation There were a variety of cases with following presentations Cervical lymphadenopathy Neck swelling for a prolonged period not responding to antibiotic therapy. There were single or multiple matted non tender swellings palpable on one or both the sides of neck. FNAC was done in all the patients. In patients were FNAC was inconclusive, histopathological examination was done. Laryngeal tuberculosis Presenting symptoms were hoarseness, odynophagia, dysphagia, loss of weight and loss of appetite. Indirect laryngoscopic examination/ videolaryngoscopy revealed diffuse erythema/edema of vocal cords with irregular surface with white tubercles occasionally. Biopsy was done to establish the diagnosis and rule out malignancy. The patients were subjected to microlaryngoscopy and biopsy under general anesthesia. Specimen was sent for histopathology. Tuberculosis of middle ear Presenting symptoms were chronic ear discharge not responding to antibiotic therapy and variable degree of conductive hearing loss. Otoscopic examination revealed multiple perforations in pars tensa of tympanic membrane with pale granulation tissue. The patients with pale exuberant middle ear underwent mastoid exploration and specimens were sent for histopathological examination. Tubercular retropharyngeal abscess Presenting symptoms were dysphagia to solids (progressive), neck pain, recurrent sore throat, loss of weight, night sweats. X ray soft tissue neck revealed widening of prevertebral shadow at the level of C6 and C7 vertebra with normal body of vertebra and disc space. Tubercular infection of preauricular sinus Patient presented with recurrent swelling in the preauricular region with discharge. Incision drainage followed by excision of sinus was done which when sent for histopathological examination revealed tuberculosis. On confirming the diagnosis, all the patients were treated by antitubercular drugs. Few patients needed conservative surgery followed by antitubercular treatment. The patients were followed up and evaluated at regular intervals.
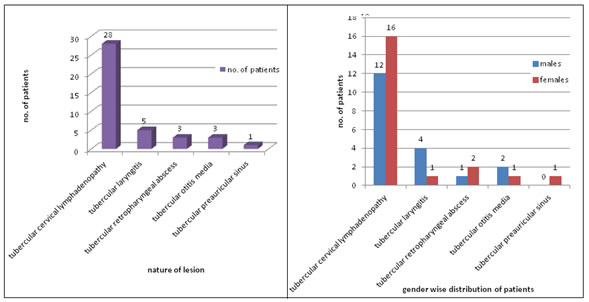
OBSERVATIONS AND RESULTS Over a period of 17 months, 40 patients who visited the ENT and Head Neck Surgery department of our institute with otorhinolaryngologic manifestations of tuberculosis were studied. Figure 1 and Figure 2 show the distribution of patients according to nature of tubercular lesion. There were 19 male and 21 female patients with male: female ratio of 0.90:1. Majority of the patients presented with tuberculous cervical lymphadenopathy i.e. 28(70%) patients. Of these 12(42.85%) were males and 16 (57.15%) were females. Incidence of tuberculosis was higher in females as compared to males. FNAC was done in all the cases to confirm tuberculosis except in 4 cases were histopathological examination of excised lymph node was done. Tubercular laryngitis was seen in 5(12.5%) patients. Of these only 1(20%) was female. Hoarseness and odynophagia were the commonest complaints. Interarytenoid area was most commonly involved seen in 3(60%) patients followed by epiglottis seen in 1(20%) patient and vocal cords seen in 1(20%) patients. All the patients underwent microlaryngoscopic examination and biopsy was taken and sent for histopathological examination which confirmed tuberculosis. Tubercular retropharyngeal abscess was seen in 3(7.5%) patients. All the patients presented with dysphagia to solids, odynophagia and neck pain. Their X ray soft tissue neck revealed widening of prevertebral shadow. Other investigations like montoux test, ESR were raised in these patients Tubercular otitis media was seen in 3(7.5%) patients 2(66.6%) of which were males.1 patient presented multiple tympanic membrane perforations with pale middle ear mucosa along with granulation tissue and marked conductive hearing loss. 2 patients had serous discharge not responding to antibiotics associated with pale granulation tissue. Biopsy was taken from granulation tissue and sent for histopathological examination which revealed tuberculosis. Tubercular infection of preauricular sinus was seen in 1(2.5%) patient. This patient present with recurrent preauricular abscesses followed by incision and drainage. The patient was posted for sinus tract excision which on histopathological examination revealed tubercular infection. All the patients after confirmation of diagnosis were started on anti tubercular therapy and showed good response to treatment. Drugs used were isoniazid, ethambutol, rifampicin and pyrizinamide. The duration of treatment was 6 months. All the patients were seen at regular intervals for noting the response to treatment. Figure 1: Distribution of patients according to nature of lesion Figure 2: Genderwise distribution of patients according to nature of lesion DISCUSSION Tuberculosis still remains a challenging clinical entity throughout the developing world despite efforts being made at every level to control this disease. India being a developing country has a large number of patients with variety of manifestations of this disease. Poor sanitation, overcrowding, low standards of living and rising number of HIV cases are the main causes for this. Pulmonary tuberculosis is most common form of the disease but extrapumonary manifestations are sen in 20% patients. In our study, 70% patients presented with tubercular cervical lymphadenopathy which coincides with the findings by Mulay and Hiranandani[5], Younus et al. [6]and Khan et al. 7 Laryngeal tuberculosis needed to be differentiated from other granulomatous diseases like leprosy, fungal infections and non infective diseases like malignancy, sarcoid or Wegner’s disease. The diagnosis was confirmed by biopsy from lesion. In our study tubercular laryngitis was seen in 5(12.5%) patients. Of these, 80 % patients were males which is similar to the observations made by Hunter et al 8 and Fang et al. 9. Interarytenoid area i.e posterior part of larynx, was most commonly involved seen in 3(60%) patients followed by epiglottis sen in 1(20%) patient and vocal cords seen in 1(20%) patients which is similar to findings by Desa[10] and Kakar et al.11 In our study tubercular otitis media was seen in 3(7.5%) patients 2(66.6%) of which were males.1 patient presented multiple tympanic membrane perforations with pale middle ear mucosa along with granulation tissue and marked conductive hearing loss. 2 patients had serous discharge not responding to antibiotics associated with pale granulation tissue. These findings were similar to study by Yaniv12 who stated that chronic ear discharge not responding to routine antimicrobial therapy was the common complaint. Fine Needle Aspiration Cytology proved to be reliable investigation especially for cases with cervical lymphadenopathy similar to findings by Khan et al[7] and Lau et al.
CONCLUSION Tuberculosis is still a rampant disease in India with extrapulmonary forms of the disease on the rise. TB lymphadenitis remains the most common manifestation in the head and neck region. Various efficient diagnostic techniques such as FNAC are available for the diagnosis of these lesions. Rare occurrence and lack of characteristic symptoms of head and neck tuberculosis often leads to misdiagnosis.
REFERENCES
|
|
 Home
Home