Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 - November 2019
Surgical management of vallecular cyst in a young infant: C- MAC to the rescue
Rajarajeswari N1, Mary Kurien2, Vikram Mohanraj3, Glynis4, Mamie Zachariah5 Sivakumar Segaran6, Vishnu Bhat7, Jaya Madhav Reddy8, Lakshana Deve9
{1Associate Professor, 2Professor and HOD, 3,10Assistant Professor, 4Resident, Department of ENT}{6Professor, 7Associate Professor, Department of Anaesthesiology}{8Professor, 9Resident, {Department of Paediatrics} Pondicherry Institute of Medical Sciences, Puducherry, INDIA. Email: rajisampathporal@gmail.com
Abstract Vallecular cyst, a rare cause of respiratory distress and failure to thrive in infancy, has also been associated with sudden airway obstruction resulting in death. Symptoms usually develop in the first week of life along with a muffled cry. Diagnosis is almost always by transnasal awake flexible nasopharyngo-laryngoscopy. Securing the airway for surgical intervention is indeed a challenge to the anaesthesiologists. Furthermore, availability of suitable instruments for this infrequent surgical procedure in the very young is an additional major concern to the attending ENT surgeon. We report the successful management of a vallecular cyst using C-MAC, in a two month old, 3.5 kg baby from a tertiary academic centre in a developing country. Key Words: Infant vallecular cyst, respiratory distress, failure to thrive, C-MAC,
INTRODUCTION Vallecular cyst is an uncommon laryngeal lesion, generally asymptomatic. However, in neonates, it can cause respiratory and feeding difficulties which can lead to significant morbidity and mortality 1. Symptoms may mimic more common benign lesions in neonate like laryngomalacia. Hence it is important to have a detailed clinical and endoscopic evaluation by the otolaryngologist especially from the tongue base to the cricopharyngeal area in addition to the larynx.2,3
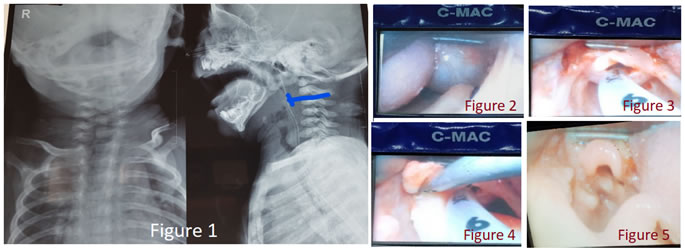
CASE REPORT A two and half month baby boy was admitted under paediatrics with noisy breathing from a week after birth and failure to thrive. He was a full term baby by normal vaginal delivery, third child to his parents with no family history of neonatal respiratory problems in other siblings. There was no cyanotic episodes, cough or aspiration while feeding. However, he had difficulty in continuously sucking for more than a minute at a time. He had not gained weight since birth. Clinical examination revealed a grossly underweight infant (3 kg) with no dysmorphic features. He had significant suprasternal and subcostal retractions with no postural variations. X ray neck soft tissue (AP and lateral views) showed radio-opaque shadow at the level of tongue base, obscuring air shadow completely. Tracheal airway appeared normal (figure 1). Flexible nasopharyngolaryngoscopy revealed a large smooth surfaced pale mass endoscopically suggestive of a cyst at the base of tongue, obscuring view of epiglottis and anterior two thirds of the laryngeal inlet. Posterior one third of the vocal cords which were visualised, were normal and mobile. Blood investigations including TSH were normal. With a clinical diagnosis of vallecular cyst, management details were discussed with baby’s parents, pediatric and anaesthetic teams. Informed consent was taken from hisparents regarding procedural complications including airway obstruction, risk to life and tracheostomy. Anticipating difficult intubation, at the onset, oxygen was delivered continuously using nasal cannula with size 3.0mm ID endotracheal tube, tailored to the distance from the nasal alae to the angle of mandible. The initial plan of approach by the anaesthetist was fibreoptic intubation under inhalational anaesthesia with spontaneous ventilation. However, this could not be done as the large cyst obscured glottic opening causing dynamic airway obstruction during respiration, and scope was non-negotiable beyond the cyst. Intubation with C-MAC videolaryngoscope was attempted next, but this was also not possible due to the cyst obscuring glottis opening in addition to the heavy nature of the C-MAC blade. Finally intubation was done successfully with Miller blade size1, by paraglossal technique and 3.5 mm PVC uncuffed endotracheal tube was secured. Throughout the procedure the baby was maintained on spontaneous ventilation with 100% oxygen and sevoflurane, titrated to effect. Due to non-availability of neonatal/ infant rigid laryngoscope, C-MAC (with pediatric blade), being available with the anaesthetist, was then used as a preliminary step to visualise the lesion. It was very well seen (figure 2) and about 0.8ml of clear mucoid fluid was aspirated. Following the collapse of the cyst (figure 3), using the same instrument, cyst wall was marsupialized with cold instruments and redundant mucosa with then excised (figure 4) Baby was kept intubated for 48 hours to protect airway in the event of post operative oedema. Nasogastric feeding was given for 5 days to allow the local area to heal well. Immediate follow up showed baby with normal cry, no respiratory distress or feeding difficulty. One week later, C-MAC examination under IV sedation revealed healing vallecular mucosa with mild oedema and no evidence of recollection (figure 5). Baby had also gained weight of 200 grams over a week, with normal oral feeding. Histopathological examination of the cyst wall showed features of a benign cyst lined by stratified squamous epithelium with subepithelial lymphohistiocytic infiltrate.
Figure 1: Radio-opaque shadow at the level of tongue base, with near total obstruction of air shadow; Figure 2: C-MAC with paediatric blade, showing the lesion clearly; Figure 3: collapsed cyst following aspiration; Figure 4: Left vallecular following removal of redundant mucosa; Figure5: Post-op one week, healing left vallecular DISCUSSION Vallecular cyst is an uncommon pharyngo-laryngeal lesion that accounts for 10.5% of all laryngeal cysts and generally asymptomatic in adults. However, presentation depends largely on the size and age of presentation. In infancy, it causes stridor, respiratory distress, feeding problems and failure to thrive 4,5. These symptoms require great attention by the attending paediatrician, as missing such cases can lead to disastrous consequences 3,6. The differential diagnoses include hemangioma, cystic hygroma, lymphangioma, tertoma, hamartoma, dermoid cyst, thyroid remnant cyst and thyroglossal duct cyst 5,7. Histologically, vallecular cyst is lined by squamous epithelium and contains respiratory epithelium with mucous glands 7,8. In cases where foetal vallecular cyst is suspected on antenatal ultrasound, a fetal MRI can be done, which will conclude the diagnosis and plan for perinatal intervention and parental counselling 7.There are two pathological hypothesis for the development of these lesions in neonates, either ductal block of mucous glands or embryologic defect of their lymphatic drainage 2, 3. Flexible nasopharyngolaryngoscopy in awake baby is the most important investigation in neonatal stridor as it can demonstrate the lesions. CT scan and MRI prior to surgical management shows the extent of the lesion, vascularity and differentiates it from more common laryngeal lesions in this age group.2,3 However, in our patient, these imagings were deferred as the baby was already in airway obstruction and further sedation for the above procedures was contraindicated. Direct laryngoscopy and marsupialisation or excision of the cyst is the treatment of choice which clearly demonstrates the cystic nature of the lesion, its origin and extent [9]. Other modalities for marsupialisation in addition to cold steel techniques with microlaryngoscopic instruments are CO2 laser, coblation, electrocautery and microdebrider techniques 5,6. In our patient the additional concern was the lack of specific instruments in this life threatening emergency. CMAC was thus considered as an alternative and used successfully. This is the first case report of its kind.
CONCLUSION C-MAC monitor (flexible intubation video laryngoscope) which is primarily used by anaesthetist for difficult airway intubation, was used in our patient successfully for marsupialisation of vallecular cyst and excision of redundant mucosa. C-MAC with its larger working channel and ergonomic design for optimal manoeuvrability, appears to be an exceptional alternative instrument for neonatal oropharyngeal emergency procedures.
REFERENCES
|
|
 Home
Home