|
Table of Content - Volume 13 Issue 2 - February 2020
Conventional adenoidectomy v\s endoscopic assisted micro-debrider adenoidectomy: A tertiary health care center study
Jolene Alokkan1*, Niveditha Gowda2, Prashanth R Reddy3, Ravikiran4
1Assistant professor, Department of ENT, East Point College of Medical sciences, Virgo Nagar Post, Avalahalli, Bengaluru- 560049. INDIA. 2Department of ENT and Endoscopic surgeon, Consultant at Brindavan Areion Hospital, Chamrajpet, Bangalore, INDIA. 3Department of ENT and Endoscopic surgeon, Senior Consultant, BGS Gleneagles Hospital, Kengeri, Bangalore, INDIA. 4Statistician, East Point College of Medical sciences, Bangalore, INDIA. Email: drjolenealokkan@gmail.com
Abstract Background: Adenoidectomy is a surgery which is routinely done in ENT. It is usually done by using the curettage method, either by itself or as a part of adenotonsillectomy. The present article is to study the use of endoscopy assisted micro-debrider as an alternative for adenoidectomy. Methods: Fifty cases requiring adenoidectomy were randomized into two groups of twenty-five each. Group A underwent conventional adenoidectomy using the curettage method and Group B underwent endoscopic assisted micro-debrider adenoidectomy. The parameters that were included were, intra-operative time, intra-operative bleeding and completeness of resection, collateral damage, post-operative pain and recovery time Conclusion: Endoscopic powered adenoidectomy was found to be a safe and effective alternative for adenoidectomy. The study parameters for endoscopic powered adenoidectomy fared better in completeness of resection, lesser post-operative pain and relatively faster recovery time. On the other hand, conventional adenoidectomy scored better in terms of lesser operative time and lesser intra-operative bleeding. Key Words: Adenoidectomy; Endoscopic assisted microdebrider adenoidectomy
INTRODUCTION Adenoidectomy is a valuable treatment option in management of obstructive sleep apnoea, middle ear pathologies, pediatric chronic rhino-sinusitis and recurrent adeno-tonsillitis. It is usually performed using the curettage method. The most common complication of this method is the injury to the Eustachian tube opening. The completeness of the removal of the adenoid by this method, cannot be guaranteed. The introduction of endoscopes has made this area more accessible and more procedures are presently performed using nasal endoscopes. Canon et al.1 popularized Endoscopic Assisted Adenoidectomy (EAA) calling it “a natural progression of endoscopic technology to allow a more complete adenoidectomy”. Microdebriders are powered instruments which provide an excellent, safe and thorough technique in endoscopic nasal surgery. They provide relatively atraumatic dissection with minimal bleeding which enables decreased surgical time and faster postoperative healing 2. Koltai et al. 3 have published the use of microdebrider for adenoidectomy using visualization by a laryngeal mirror. When both these methods are combined and endoscopic assisted microdebrider adenoidectomy performed, advantages of both techniques should get pooled. The present study was designed to compare the endoscopic assisted microdebrider adenoidectomy versus conventional adenoidectomy and collect the required study data.
MATERIAL AND METHODSThis study was carried out in a tertiary care teaching hospital over a period of one year. To achieve the objectives of our study, a prospective randomized trial was designed. Fifty cases between the ages of 4-14 years and requiring adenoidectomy for various indications were included in the study. On admission, the subject underwent a baseline evaluation including nasal endoscopy. The grade of adenoid hypertrophy was assessed using the scale described by Clemens and Mcmurray4 where Grade I has adenoid tissue filling 1:3 the vertical height of the choana, Grade II up to 2:3, Grade III from 2:3 to nearly all but not complete filling of the choana and Grade IV with complete choanal obstruction . All the patients were randomized into two groups consecutively - Group A consisted of cases undergoing conventional adenoidectomy using the traditional curettage method and Group B undergoing endoscopic powered adenoidectomy. All surgeries were performed under general anesthesia, using endotracheal tube and a laryngeal pack. In the conventional technique, adenoidectomy was done using the adenoid curette. In the endoscopic technique, the endoscope was used along with a microdebrider with saline irrigation using speeds up to 3000 rpm to curette and shave off the adenoid tissue using adenoidectomy blades. Nasal packing using gauze was used to control the bleeding. The procedure was visualized using 2.7mm nasal endoscope through the ipsilateral nostril. The intra-operative parameters studied were operative time, primary bleeding, completeness of removal of adenoid and collateral damage. Post-operative parameters were assessment of post-operative pain and recovery time.
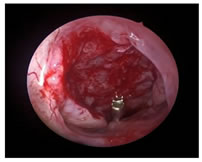
Figure 2: End of procedure showing complete removal of adenoid mass
Intra operative time was defined as the time taken for completion of the procedure from the time patient was handed over by the anesthetist and included setting up of instruments, operative steps, packing and securing the bleeding. The time keeping ended when the patient was handed back to the anesthetist. In cases where tonsillectomy was also combined, the time taken for tonsillectomy and haemostasis was deducted. The amount of primary bleeding was assessed by a rough measure. For the conventional adenoidectomy group, the number of 3×3-inch gauze pieces, used for packing the nasopharynx, were counted and each gauze was assumed to a corresponding blood loss of 10 ml. In the endoscopic method, the blood loss was assessed by whatever came into the suction, minus the irrigation solution and the number of gauze pieces used. After the surgery, the completeness of adenoid removal was seen by doing a diagnostic nasal endoscopy in both groups. A less than 25% residual adenoid was regarded as complete removal, 25-50% as partial and more than 50% residual as incomplete removal. Post operatively, the patient was assessed for post-operative pain using a six-point faces scale (where 0= no pain and 5= intolerable pain). The recovery time was defined as the number of days taken to return to normal activity as told by the patient / parents during the routine post-operative follow-up visit at seven days. The data so obtained was compared in each group and analysed using Chi-square test to obtain p-value. All subjects including their parents were counselled about the nature of the study and informed consent taken.
RESULTSThe mean age of the patients in Group A was 7.8 years, while that of Group B was 7.5 years. The kind of surgical procedure done is shown in Table 1. Table 1: Type of surgical procedure performed
Recurrent adenotonsillitis was the single most common diagnosis seen in the patients (Table 2). On doing nasal endoscopy pre-operatively, a Grade 3-4 adenoid hyperplasia was seen in both the groups.
Table 2: Indications for adenoidectomy
The operative time, in Group A patients, varied from 20-40 mins, the mean being 30.5 mins. The operative time, in Group B patients, varied from 30-50 mins, the mean being 41.7 mins (Table 3). T-test analysis of the results gave a significant p-value.
Table 3: Operative Time
The blood loss in Group A was in the range of 10-50 ml with a mean of 28.8 ml. The blood loss in Group B was in the range of 10-70 ml with a mean of 45.2 ml (Table 4). T-test analysis of the results gave a p-value which was significant.
Table 4: Blood loss
Nasal endoscopy done after the surgery showed that the adenoid resection was complete using the endoscope and microdebrider. But in Group A, 10 cases showed about 50% adenoid tissue remaining. The nasal endoscopy done after the surgery also showed there was no collateral injury after the surgery in either of the groups. As the study sample included some patients who also had undergone tonsillectomy along with the adenoidectomy, these patients were excluded from the post-operative pain evaluation as the post tonsillectomy pain might not be differentiated from the post adenoidectomy pain. So effectively, we were left with 5 patients in Group A and 15 patients in Group B for this particular parameter. In Group A, the mean pain score was 2.8, and in Group B the mean pain score was 1.2 (Table 5). Chi-square analysis of the results gave a significant p-value. Table 5: Post-operative pain
In the follow-up phase, the recovery period was assessed in both groups. Group A had a mean of 3.8 days, while Group B had a mean of 3.3 days.
DISCUSSIONThis study aimed to compare the conventional curettage method with the newer endoscopic powered technique. Patients were randomly divided into 2 groups. There is an increasing trend to perform adenoidectomy in isolation rather than combine it with adeno-tonsillectomy 5. This trend was somewhat seen in our series where 40% of the cases (20) were operated for adenoids alone. This is in contrast to conventional teaching of combining adenoidectomy with tonsillectomy. The indications of surgery were varied and included recurrent adenotonsillitis, snoring and otitis media with effusion. Though the precise steps of the adenoidectomy would only take 10-15 minutes, the correct assessment of the operative time should include all steps including setting up of instruments, packing and securing the bleeding and checking for haemostasis. The overall operative time may be on the higher side as post procedure endoscopy was performed in all cases. The increase in the operative time in the newer technique is probably due to increased set-up time for instrumentation, endoscopic visualization, bit by bit removal of the adenoid tissue and time consuming haemostasis. Our findings are in contrast to those by Stanislaw et al. 6 who have reported powered adenoidectomy to be 20% faster than curette adenoidectomy. In their study they have used a 45° angled shaver blade through the oropharynx and not the nose. The visualization was with a laryngeal mirror and not using endoscopes. The micro-debrider is potentially a dangerous instrument which should be used under direct and close vision as that provided through an endoscope. The time taken for setting up the instrumentation is also reduced in their study. The present study, however, showed a statistically significant increase in the operative time of endoscopic powered adenoidectomy versus conventional curettage adenoidectomy. Intra-operative blood loss was higher in Group B patients. As the endoscopic surgery is a bit by bit approach, the raw bleeding surface is exposed for a longer time. An increased operative time would also lead to increased bleeding per se. The blood loss in the series by Feng et al. 7 was more in the conventional adenoidectomy group though it was not statistically significant. Stanislaw et al. 6 however reported a significant reduction in blood loss following endoscopic adenoidectomy. It has often been noted that the extent of resection following conventional adenoidectomy has been incomplete 8. It can lead to a recurrence of symptoms and failure of the surgery. It was felt therefore that an endoscopic assessment be used to determine the extent of residual tissue. The results show that resection was complete by the endoscopic method. In contrast, curettage method had 10 cases in Group A where about 50% tissue was remaining. In endoscopic assisted adenoidectomies, the nasopharynx can be seen properly and remnant bits of adenoid tissue removed accurately under vision. This makes endoscopic powered adenoidectomy more complete. Collateral damage following adenoidectomy is uncommon, but there is a chance of causing scarring on Eustachian tube opening. In our study, no collateral damage was seen in either group. Adenoidectomy is a well-tolerated procedure. The six-point faces pain scale which is shown to be a simple and reliable pain scale was used 9. The post-operative pain in the conventional adenoidectomy group was statistically more significant than in the endoscopic assisted microdebrider group. The method used to measure the recovery time in this study was to let the parent / patient determine when patient felt normal. The question was asked about “How soon you returned to routine activities” following the surgery in the post-operative follow up. The time taken to recover in the debrider assisted adenoidectomy group was slightly lesser than the conventional adenoidectomy group.
CONCLUSIONThe newer method of endoscopic powered adenoidectomy was found to be a safe and useful tool for adenoidectomy. Its advantages included completeness of resection, accurate removal, lesser post-operative pain and relatively faster recovery time. Its disadvantages included increased surgical time and increased bleeding. Endoscope assisted microdebrider adenoidectomy needs to be acknowledged as a safe alternate to conventional adenoidectomy. But not all centers have the facility of using an endoscope and microdebrider. Also, the additional cost has to be borne. The use of powered adenoidectomy is technically demanding in the pediatric age group due to relative difficulty in passing both the scope and debrider blade through the nose. REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home