|
Table of Content - Volume 13 Issue 3 - March 2020
Inside out technique for cholesteatoma surgery: Functional and anatomical outcomes
Anchal Gupta1*, Sonika Sharma2, Padam Singh Jamwal3
1Senior Resident, 2Postgraduate, 3Professor, Department of ENT, Head & Neck Surgery, SMGS Hospital, Government Medical College, Jammu, Jammu and Kashmir, INDIA. Email: anchalsachit@gmail.com
Abstract Background: Atticotomy avoids unnecessary procedures, such as a wide (extended) mastoidectomy and provides better exposure of the sinus tympani, facial recess, and hypotympanum. It avoids the complications involved with Korner’s septum,an anterior sigmoid sinus, and a low-lying dura. Materials and methods: The present retrospective observational study was carried out in the Department of ENT and Head and Neck Surgery, S.M.G.S Hospital, Govt. Medical College, Jammu for a period of 2 years w.e.f. August 2016 to August 2018. The study involved 40 patients presenting with chronic suppurative otitis media with cholesteatoma. All of them underwent inside out mastoidectomy and were followed upon till the end of the study to evaluate the efficacy of inside out mastoidectomy in eradicating the disease from the middle ear cleft, to assess preservation of hearing and to assess cavity problems. Results: Male: female ratio of 1.35: 1 was seen. Mean age of presentation was 33+2.5 years. Commonest presenting symptom that was seen in all 40(100%) patients was ear discharge. Achievement of cholesteatoma removal was done in all 40(100%) patients. In all patients posterior canal wall reconstruction was done using conchal cartilage. On follow up 95% patients had dry self cleansing cavities and only 2(5%) patients had accumulation of wax and debris that required cleaning every 3 months. The cavity was smaller in size with, the post-op cavity problems were fewer and seen in only 3(7.5%) patients. The mean post-op air bone gap closure at 3 months was 11.55dB. Conclusion: Inside out technique is the preferred technique for cholesteatoma surgery to ensure small cavity formation. The cholesteatoma removal achievement was 100%. Keywords: cavity, cholesteatoma, surgery.
INTRODUCTION Panse1 performed a transcanal lateral atticotomy alongside the malleus and incus in order to remove a cholesteatoma in 1898, but he reported a preference for radical mastoidectomy. Chandler and Freeman2 suggested this limited and exteriorizing operation for only one hearing ear. Dingley and Zwiefach3 suggested limiting it for cholesteatoma surgery. Donald et al.1 stated that they used this technique for extirpation of a limited cholesteatoma and mobilization of the fixed ossicular chain. Fleury et al.4 also described a technique based on transcanal atticotomy. Thus far, there are only a few recent articles on atticotomy.5-7 The subject debated endlessly in the choice of surgical technique, open versus closed mastoidectomy. Generally, open techniques provide good control of excision of the cholesteatoma, but facilitate the development of infections, require regular control and entail limitations for bathing. Closed techniques generate a lower rate of infection and do not limit bathing, but result in a higher percentage of residual and recurrent cholesteatomas, whilst also requiring periodic controls.8,9
MATERIALS AND METHODS The present retrospective observational study was carried out in the Department of ENT and Head and Neck Surgery, S.M.G.S Hospital, Govt. Medical College, Jammu for a period of 2 years w.e.f. August 2016 to August 2018. The study involved 40 patients presenting with chronic suppurative otitis media with cholesteatoma. All of them underwent inside out mastoidectomy and were followed upon till the end of the study to evaluate the efficacy of inside out mastoidectomy in eradicating the disease from the middle ear cleft, to assess preservation of hearing and to assess cavity problems. Inclusion criteria
Exclusion criteria:
Surgical technique:
Inside out approach: Epitympanotomy: Bony meatus was enlarged with a 3-4 mm cutting burr to remove bone from posterior and superior walls of the external meatus at the isthmus including the Henle’s spine. Overhang was taken away from the outer bend and the meatus was straightened before removing the outer epitympanic wall. The attic was then enlarged with a 2mm burr and small curettes, working from within outwards, to expose the cholesteatoma fully. Anteriorly, bone removal was extended either beyond the limit of cholesteatoma or in flush with anterior epitympanic wall. While drilling great care was taken not to make contact with an intact ossicular chain for the fear of inducing hearing loss. Epitympanomastoidectomy: 4-5 mm cutting burr was used in circular pattern as if enlarging the meatus until the whole cholesteatoma is uncapped. The burr was used from within outwards , away from the facial canal and the depth frequently assessed. If the body of the incus was not present, the position of the facial canal was ascertained either by lifting the epitympanic portion of the cholesteatoma to see it lying within its canal or by seeking stapes remanant. Once the approximate position was known, posterior canal wall was lowered to a suitable depth. Removal of the disease: The entire cholesteatomatous matrix was carefully removed Ossicular and middle ear reconstruction: The graft was placed from anterior annulus over the middle ear space and draped over the horizontal semicircular canal. This reduced the depth of middle ear space by more than halving its depth. Hence reconstruction of the middle ear was done. Ossicular chain reconstruction was done according to the erosion of ossicular chain. Post-operative care: Mastoid compression bandage was done . Post-operative antibiotics were continued for about 10. First cavity cleaning was done at three weeks post-operatively and merocel pack was removed at this time. Steroid containing ear drops were used in patients with granulation tissue. Any superficial infection was controlled by topical antibiotics.
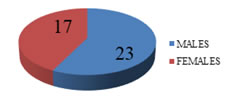
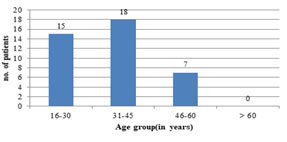
OBSERVATIONS AND RESULTS In our study we studied 40 ears with CSOM with cholestatoma on which inside out technique for cholesteatoma surgery was performed. Age and Sex distribution of patients: Out of 40 patients 23 were males and 17 females with male: female ratio of 1.35: 1[Figure 1]. Slight male preponderance was seen. 18(45%) patients were in the age group of 31-45 years. Mean age of presentation was 33+2.5 years. Figure 2 shows age wise distribution of patients
Figure 1: Genderwise distribution of patients
Figure 2: Age wise distribution of patients
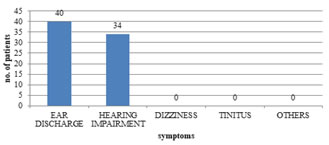
Clinical presentation of patients. Commonest presenting symptom that was seen in all 40(100%) patients was ear discharge followed by hearing impairment which was seen in 34(85%) patients.[Figure 3]
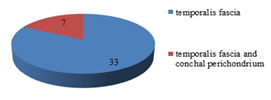
Figure 3: Distribution of patients according to presenting symptoms Type of fascia used as graft In all patients mastoidectomy was performed with inside out technique and 28 cases were performed under LA and 12 cases were performed under GA. Temporalis fascia was used as graft material in 33 patients and temporalis fascia and conchal perichondrium was used in 7 patients.[Figure 4] Figure 4: Type of graft used
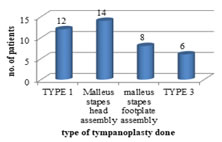
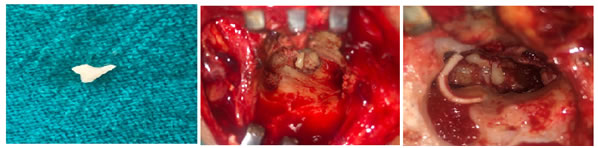
Type of ossiculoplasty done Achievement of cholesteatoma removal was done in all 40(100%) patients .[Table 1] Ossicular chain reconstruction using autologous incus was done in 16 patients and using conchal cartilage in 12 patients. The remaining 12 patients underwent type 1 tympanolasty in which all ossicles were intact and neither incus nor conchal cartilage was used for reconstruction. In all patients posterior canal wall reconstruction was done using conchal cartilage.[Figure 5-8] Type of ossiculoplasty done Achievement of cholesteatoma removal was done in all 40(100%) patients .[Table 1] Ossicular chain reconstruction using autologous incus was done in 16 patients and using conchal cartilage in 12 patients. The remaining 12 patients underwent type 1 tympanolasty in which all ossicles were intact and neither incus nor conchal cartilage was used for reconstruction. In all patients posterior canal wall reconstruction was done using conchal cartilage.[Figure 5-8]
Table 1: Cholesteatoma clearence
Figure 5: Distribution of patients according to type of tympanoplasty done.
Figure 6 Figure 7 Figure 8 Figure 6: Remodelled incus used for ossiculopasty; Figure 7: Malleus stapes head assembly; Figure 8: Atticoantrostomy with malleus stapes head assembly with posterior canal wall reconstruction using conchal cartilage
Postoperative adverse events following surgery On follow up 95% patients had dry self cleansing cavities and only 2(5%) patients had accumulation of wax and debris that required cleaning every 3 months. Post-op incision site infection was observed in 2(5%) patients and granulations in 1(2.5%) patient. The cavity was smaller in size with, the post-op cavity problems were fewer and seen in only 3(7.5%) patients.[Table 2]
Table 2: Postoperative adverse events
Air bone gap closure at 3 months The mean post-op air bone gap closure at 3 months was 11.55dB. Table 3 shows mean preoperative and postoperative air and bone conductions and air bone gap closure at 3 months. Table 3: Air bone gap closure at 3 months
DISCUSSION Anterior atticotomy enables us to avoid perforation of the tympanic membrane and disturbance of the ossicular chain in chronic otitis media without cholesteatoma. Moreover, mastoid pathologies can be addressed without mastoidectomy after visualization using an endoscope through the auditus.7,10,11 In contrast, posterior atticotomy requires a large mastoidectomy cavity. Part of the scutum should also be excised to expose and allow operation of the attic region. In our study we studied 40 ears with CSOM with cholesteatoma on which inside out technique for cholesteatoma surgery was performed Achievement of cholesteatoma removal was done in all 40(100%) patients. On follow up 95% patients had dry self cleansing cavities and only 2(5%) patients had accumulation of wax and debris that required cleaning every 3 months. Post-op incision site infection was observed in 2(5%) patients and granulations in 1(2.5%) patient. The cavity was smaller in size with, the post-op cavity problems were fewer and seen in only 3(7.5%) patients. Roth et al., performed Inside Out Mastoidectomy in 604 patients between 1992 to 2006 and noted 95% dry ears which is the same as our present series.8 Yung performed inside out mastoidectomy in 39 cases and found 74% of their cavities to be dry.12 Lailach et al. compared health related quality of life (HRQOL) after sequential cholesteatoma surgery including exclusively transcanal technique (ETC), combined transcanal transmastoidal technique (TCM) and canal wall down surgery with obliteration (CWD).13 Patients receiving ETC tended to report lower restrictions in HRQOL. Patients receiving canal wall down surgery with obliteration showed equivalent limitations in HRQOL compared to closed techniques (ETC, TCM). This is quite similar to our study where only 5% patients were affected due to debris in the ear canal.
CONCLUSION It is hence concluded on the basis of our study that Inside out technique is the preferred technique for cholesteatoma surgery to ensure small cavity formation. The cholesteatoma removal achievement was 100%. There was hearing improvement post operatively as mean air-bone gap closure was 11.55 dB. So, overall quality of life provided by this technique was good.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home