|
Table of Content - Volume 13 Issue 3 - March 2020
Correlation of body mass index with change in voice
Asitama Sarkar1, Vishal K Magdum2, Shishir D Gosavi3*
1Senior Resident, 2Associate Professor, 3Professor, Department of ENT, Sanjeevan Medical Foundation, ENT PG Training Institute, Station Road, Miraj – 416410, Maharashtra, INDIA. Email: asitama_16@yahoo.com , vishalkmagdum@gmail.com, shishir3801@gmail.com
Abstract Background: Studies have recently shown that our body structure plays a key role in production of voice. The acoustic signals, which are perceived as voice, depend on the fundamental frequency and other harmonic components which in turn are determined by the built and adiposity of the person1. The aim of this study is to evaluate the influence of body structure in patients with dysphonia. Body mass index serves as the tool to measure body structure. This is a case- control study wherein 60 patients who came to the OPD with complaints of dysphonia but had no mid-membranous vocal fold lesions were included as cases and 60 persons without complaints of dysphonia nor presence of vocal fold lesions were taken as controls. 60 percent of patients who came with dysphonia had deranged BMI. Laryngo-pharyngeal reflux was found to be the most common causative factor for dysphonia in patients with the deranged BMI. This study provides with a better understanding of the causative factors by attempting to correlate body structure with voice change. This will help patients to make relevant lifestyle adjustments and avoid recurrence. It also will provide the ENT practitioner a basis for early diagnosis and prevention. Key Word: Laryngo-Pharyngeal Reflux, Dysphonia, BMI, Chronic Non-Specific Laryngitis, Voice Change.
INTRODUCTION Voice provides us with the framework on which our speech is constructed. Pathological phonation or dysphonia is associated with imbalance in the normal ratio of periodic noise components of the acoustic signal, thus resulting in poor voice quality. Two main features determining these acoustic signals include the fundamental frequency and the harmonic components. Specific factors that may potentially be responsible for voice physiology include body weight and fat volume. However, there is sparse literature available on the impact of physique on voice production and dysphonia. Da Cunha et al. investigated the difference in metrics of voice quality between non-obese and morbidly obese persons and confirmed that the obese were vocally disadvantaged2. Aaron d, Friedman et al. proved that increased adiposity is associated with decreased speaking fundamental frequency3. Further, in May 2017 De Souza and Dos Sandos found that body mass index (overweight and obese categories) influenced the average fundamental frequency4. Dysphonia is a frequently occurring symptom encountered in the OPD by the ENT practitioner. Chronic non-specific laryngitis is extremely common amidst patients who present with history of dysphonia. Other symptoms that are often associated include throat discomfort with recurrent need to clear the throat and sometimes, halitosis, throat pain and globus pharyngeus. Three most important etiological factors for non-specific laryngitis are smoking, voice abuse and most common and recently discovered gastro-esophageal reflux disease (GERD). Laryngopharyngeal reflux which occurs following gastro-esophageal reflux has been used as inter-changeable terms in this study and is of particular importance since it is a known fact that over-weight and obese persons are most prone to developing GERD. The association of GERD with chronic non-specific laryngitis, which causes dysphonia, has been studied in the past. In 1982, Ward and Berci studied that GERD caused laryngitis due to chronic throat clearing and coughing5. Deveney et al... did a more invasive cohort study wherein they showed that Nissen’s fundoplication improved non-specific laryngitis in GERD patients and thereafter, dysphonia was relieved in them6. Also, Hanson et al... found that use of proton-pump inhibitors proved beneficial for patients who came with voice change secondary to chronic laryngitis7. Considering the above available literature, the purpose of this study is to assess the different changes in voice in patients with no obvious membranous vocal fold lesions and finding out whether or not body structure has a role to play as a pre- disposing factor for these changes. Also, the idea is to find a correlation, if at all, between body mass index (used as the tool to measure body structure) and change in voice. The above information will serve to aid in the conservative management of these patients.
METHODOLOGY This is a case-control study that consists of prospective and non-interventional analysis of data. The Institutional Research Review Board and Ethical Committee approved the study design. Written informed valid consent was taken from each of the participants. No animals were involved and no humans were harmed during this study. Based upon the available literature, in our study we worked around the following hypothesis- “Production of voice is influenced by the structure of the body and a person with deranged BMI is more prone to change in voice compared to one who is within the normal BMI range”. A total of 120 individuals participated in the above study. The sample group sized 60 patients who had complaints of change in voice but had no mid-membranous vocal fold lesions. The control group consisted of 60 persons who were roughly of the same age group and gender but had no complaints of voice change. Also they did not have any vocal fold lesions. It has been established that body mass index and body fat volume relate to each other[8]. Therefore, body mass index has been used as the tool here to measure the body structure. For all the patients who came to the OPD with history of voice change, perceptual assessment of the changed voice was done after which they were subjected to a specifically designed questionnaire. This questionnaire required information about the dietary habits and alcohol intake of the participants apart from other details in order to calculate their body mass index. Thereafter, visual assessment of the vocal folds was done for all participants using a 70-degree rigid laryngoscope. The ones who were found to have mid- membranous vocal fold lesions like vocal nodules or polyps were excluded from the study. The same questionnaire was also given to the control group participants who had no complaints of dysphonia. Body mass index was calculated using the standard formula, which is body weight divided by square of the body height and expressed in kg/m2. Each participant was categorized as per the WHO classification[9] as underweight (<18.5), normal (18.5-24.9) overweight (25-29.9) and obese (>30). Thereafter, the data collected was evaluated and interpreted.
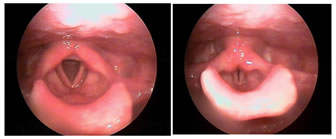
RESULTS Most of the patients who came with complaints of voice change showed features of laryngo-pharyngeal reflux on visual assessment (70-degree rigid laryngoscopy). These included presence of posterior commissure hypertrophy, erythema and thickening of the inter-arytenoid region, pachyderma and congested vocal folds[Fig.1]. The patients also showed signs of chronic laryngitis[Fig.2]. There was no evidence of any mid-membranous lesion such as vocal fold polyps or nodules in any of these patients. An objective analysis of the voice parameters revealed reduction in pitch range and maximum phonation time.
Figure 1: shows posterior commissure hypertrophy, erythema and thickening of the inter-arytenoid region, pachyderma and congested vocal folds; Figure 2: chronic laryngitis in adducted vocal folds. Of the total of 120 cases and controls, 58 were in the normal BMI range, 8 were underweight, 36 were overweight and 18 were obese. Of the total of 120 cases and controls, 58 were in the normal BMI range, 8 were underweight, 36 were overweight and 18 were obese.
The prevalence of deranged body mass index amidst the cases was 60% while that amidst the controls was 43.3%.
70.58 % of the male patients had deranged BMI while 46.15% females fell in the abnormal BMI range. Higher amount of estrogen production in the adipose tissues in women with raised body mass index can cause increased fundamental frequency of speech. But this is more commonly seen in post-menopausal women, and since the study included women of all age groups, the result obtained with respect to gender is not unusual.
60 cases were further categorized based on their alcohol consumption.
Upon interpretation of the questionnaires given to each of the participants, it was observed that most of these patients with voice change had certain dietary habits in common. 82% of them had increased intake of oily and spicy foods- chutneys, pickles on a regular basis. More than 90% of the dysphonic patients frequently consumed large quantity (more than 4-5 cups) of tea and coffee. 60% of them quantified their daily intake of sweets as roughly being equivalent to 4-5 tablespoons of sugar/day. Also, most had irregular frequency of meals and irregular meal gaps. It was noted that the time gap between their last meal of the day and sleep was lesser than approximately half hour.
DISCUSSION Change in voice in patients who do not have any mid-membranous lesions occurs almost always due to chronic non-specific laryngitis, which in turn is closely associated with chronic gastro-esophageal reflux disease. The inter-arytenoid area acts as a gutter for all the pharyngeal secretions. When there is backflow of gastric contents crossing the lower and upper oesophageal sphincters, the acid pepsin causes harm to the sensitive laryngeal mucosa and initiates an inflammatory process. It has been reported that there are reduced levels of bicarbonate producing enzyme (carbonic anhydrase subtype III) in the laryngeal epithelium of patients with laryngopharyngeal reflux10. This unprotected laryngeal mucosa when damaged causes chronic laryngitis and change in the vocal fold anatomy. It results in irregular mucosal waveform vibrations that produce an aperiodic sound. This sound is perceived as the hoarseness in the voice. The recent studies mentioned above have shown that body structure also has a strong influence on our voice. Obesity is known to reduce average maximum phonation time while fundamental frequency is directly related to the mass, elasticity and length of the vocal folds which is dependent on the built of the body. The relation between obesity and voice lies in the interference of excessive body weight on abdominal breath support during voice production.8 Obese individuals have stronger respiratory muscles owing to greater diaphragmatic motion and weight. This allows more airflow power and therefore have higher subglottal pressure in phonatory airflow parameters as studied by Solomon et al.11. In post-menopausal women not undergoing hormone treatment increased BMI has been correlated with increased fundamental frequency12. There is higher amount of estrogen production in the adipose tissue in women with higher BMI. Obese patients with hypothyroidism have hoarse, deepened pitch and slow hesitant speech. They suffer from voice fatigue and dryness of throat. On the contrary, being underweight maybe assumed to affect voice via poor blood circulation, poor physical condition, psychological distress, hyperthyroidism and sometimes decreased muscle tension/tone8. Hyperthyroidism is associated with increased hoarseness and tremors affecting the voice. The vocal folds are hypervascularised and hyperkinetic. Muscle tension dysphonia occurs secondary to poor vocal hygiene, dietary and lifestyle issues. Laryngeal muscles try to overcome this deficiency during production of voice. The differences in lung capacity of underweight as compared to normal range and obese persons might be explained by the effect of significantly less movement, weight, and strength of and hence worse performance the diaphragm in underweight persons during pulmonary testing. Good reflux control is primary for treatment of vocal cord dysfunction. A trial of routine proton pump inhibitors is recommended for minimum 8 weeks1. Following this, relief in symptoms and improvement in voice calls for ceasing drug therapy and ask the patient to follow-up with the doctor regularly on OPD basis. In cases wherein 8 weeks of proton pump inhibitor with levosulpiride therapy fails to improve the patient’s symptoms, further investigations are warranted. This includes 24-hour pH monitoring which if found to be abnormal, must be treated with another 8 weeks course of proton pump inhibitors. If pH is found to be within normal range, then higher investigations like upper gastrointestinal endoscopy maybe needed. Use of serratiopeptidase as an adjuvant may help to reduce the pachyderma in most cases. In some chronic recurrent cases, a short course of steroid therapy should be considered. Supportive therapy and adequate counseling on lifestyle modifications is of utmost importance and contributes to literally more than half of the management in these dysphonic patients. Vocal hygiene, inhalational therapy, adequate hydration is a significant primary step in conservative management of these patients. Consumption of regular balanced meals at regular intervals and avoidance of oily and spicy foods is highly recommended. It is also important that the patient maintains a time gap of minimum two hours between the last meal of the day and bedtime. Inculcating healthy habits like simple exercises, avoiding smoking and alcohol intake and coping with stress must be explained to each patient who comes in with history of dysphonia owing to non-specific laryngitis. Speech therapy can also aid to improve the quality of voice in these patients. There are certain limitations to this study. The first limitation pertains to the relatively small number of participants in each group. This leads to reduced power is establishing causality between deranged body weight and dysphonia. Owing to monetary constraints, only visual assessment was done. Other objective methods of evaluation like stroboscopy was not performed. Change in voice is assessed based on perception of patient (as a complaint) and perception of ENT practitioner (upon examination). Therefore, it is prone to human error. Also, in order to keep the study concise and simple, co-morbidities like diabetes mellitus and hypertension have not been taken into account and confounding factors like smoking also have not been considered. The above study is an attempt in understanding dysphonia in patients with no mid-membranous lesions. Patients who had deranged body mass index were found to be more prone to voice change primarily due to the increased laryngo- pharyngeal reflux in them. This study helps to recognize the significant role that body structure plays in changing voice. Further, conservative management of such patients must be more focused and stress on counseling must be taken into account by the ENT in order to improve the hoarseness in voice of such patients.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home