|
Table of Content - Volume 14 Issue 3 - June 2020
Recent trends in the management of invasive fungal rhino sinusitis
Akshay Vijay Sarode1*, Ganesh Vihapure2
1Assistant professor, Department of ENT, Government Medical College, Jalgaon, Maharashtra, INDIA. 2Assistant Professor Department of ENT, Krisna Institute of Medical Sciences, Karad, Maharashtra, INDIA. Email: drakshaysarode@gmail.com
Abstract Aims and Objectives: Even though it is acceptable that surgical debridement in combination with antifungal therapy is the main line of treatment, Still it is a subject of debate as = Which oral antifungals to prefer itraconazole/voriconazole/pasoconazole? What should be adequate dose of AmphotericinB? What should be extent of surgical debridement with intra orbital or intracranial spread? Management of intra cranial abscess -craniotomy or aspiration? Materials and Methods: A prospective study is conducted in ENT department of our hospital in collaboration with ophthalmology and neurosurgery department. The study included histology proven 14 cases of fungal rhinosinusitis between June 2010 to till date Summary: 9out of 14are cured and only 1has recurrence,2 had died of chronic renal failure. 1 had died of septicemia while 1patient lost to followup. Conclusion: Rhino-orbito-cerebral mycosis is an invasive fungal infection which occur primarily in paranasal sinuses and progress to involve orbit and brain. With the review of literature & study of similar case series published previously, we formulated our own treatment strategy. In our prospective study we found the results to be highly promising. Key Word: invasive fungal rhino sinusitis.
INTRODUCTION Rhino cerebral mycosis is a rapidly progressive opportunistic infection predominantly affecting immune compromising conditions like use of prolonged corticosteroid therapy, HIV infection, diabetes mellitus, alcoholism. The maxillary sinus is involved in 80% cases followed in order of frequency by ethmoid, frontal sinus and sphenoid sinus. As per the WHO statics India leads the world with largest number of diabetic subjects. With the increasing incidence of diabetes the associated complications like invasive Rhino-orbito-cerebral fungal infections are on the rise too. Aspergillosis and zygomycosis are mainly responsible for intracranial spread whereas candida, coccidio mycosis, histoplasma and cladosporium are the other fungi causing rhino sinusitis. In such patients response to treatment depends upon early diagnosis and initiation of antifungal treatment augmented by appropriate surgical debridement. Most of the time complete cure is rarely achieved. The purpose of this manuscript is to report the case series of our hospital wherein we found in spite of the high morbidity associated with invasive fungal rhino sinusitis if detected early and dealt in a stepwise manner then the results are promising.
MATERIALS AND METHODS Study is approved by the institutional ethical committee. A prospective study is conducted in ENT department of our hospital in collaboration with ophthalmology and neurosurgery department during June 2010 to till date. The study included 14 patients which were evaluated at presentation including a detailed history, ENT, ophthalmic and neurological examination to assess the extent of disease. Diagnostic nasal endoscopy was performed and biopsy was sent for histological examination and KOH preparation. CT scan and MRI of PNS and brain were obtained to assess the extent of disease spread. Treatment with systemic AmphotericinB was started as soon as the diagnosis of invasivefungal sinusitis was confirmed. After a test dose of 1mgAmphotericinB in 100ml 5% dextrose,1-1.5mg/kg/day of AmphotericinB was given over 4-6hours.The dose was increased slowly, monitoring serum creatinine and was continued till cumulative dose of 3to5 gm was reached. Surgical debridement was then planned according to the stage of disease. In 13 cases an endoscopic approach was used difficulty was encountered in removing the disease from the orbital apex, superior tosphenoid sinus and also when the defect in skull base was smalland the disease was extensive. In 2 patients disease was removed with help of neurologist by anterior craniotomy approach. Post op patients were subjected to regular nasal endoscopic examination with suction clearance once weekly for 4weeks and once monthly for 1year. As per the species isolated, after completion of inject able AmphotericinB patient was then started on oral antifungal like Itraconazole or voriconazole for a period of 6-7 months. Clinical Staging: Classification of signs and symptoms according to the stage of presentation:
Symptoms
Signs
No. of patients
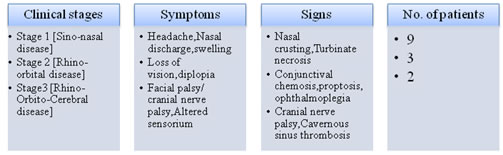
Uncontrolled diabetes was the common underlying disease in 13 out of 14 cases, 5 out of 13 were in diabetic ketoacidosis. one was HIV positive. The methodology for staging the disease was adopted from studies by Nityanand et al in 2003. Clinical Presentation Stage 1: Skinerytema with disease limited to sinuses only. Stage 2: Exension to orbit and palate Stage 3: Intracranial extension with cranial nerve palsy Treatment strategies as per the clinicaland radiological staging Stage 1
stage 2
Stage 3
Treatment Protocol: With the review of literature and study of similar case series published in our country we formulated our own a stepwise approach as DISCUSSION According to WHO, India stands to become the “Diabetes Capital of the World” by 2025. With the increasing incidence of diabetes, the associated complications like Rhino-orbito-cerebral mycosis are also on the rise. The purpose of this article is to draw attention to the clinical presentation, need for high index of suspicion for early diagnosis and a stepwise approach to the disease. Spread of disease is directly proportional to the time delay in the diagnosis. ENT surgeon are in best position for early diagnosis with endoscopy as disease always begins in nose and spreads rapidly to adjacent vital structures. DNE in patients with uncontrolled diabetes and any nasal complaint, facial edema or headache is the only way to pick them early. Any blackish discoloration or crusting in the nasal cavity should be sent for KOH staining, fungal culture and histopathology. Outcome Of Our Study: 9out of 14 are cured and only 1has recurrence of disease, 2 had died of chronic renal failure.1 had died of septicemia while 1 patient lost to follow up. With the review of literature and study of similar case series published in our country we formulated our own treatment strategy. As per the clinical stage wise approach adopted and use of organism specific antifungal, we can certainly offer far better outcome to the patient and can avoid unnecessary disfiguring surgeries like orbital excenteration in stage1 and even in stage2 also.
CONCLUSION
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home
