|
Table of Content - Volume 15 Issue 1 - July 2020
Impact of nasal surgery in allergy rhinitis
Ashish Rao1, Akshith Battula2*, Harsha Pandiyan3
1Consultant, Anand Ent and Allergy Centre, Bengaluru, Karnataka, INDIA. 2Post Graduate, 3Assistant Professor, Department of ENT, Vydehi Medical College, Bengaluru, Karnataka, INDIA. Email: ashishrao1790@gmail.com
Abstract Background: Allergic Rhinitis is a complex condition with a high incidence rate in India, Patients with allergy rhinitis may present with other nasal disorders such as deviated nasal septum, inferior turbinate hypertrophy nasal polyposis etc. Such disorders have to be treated surgically, for example septoplasty for deviated nasal septum and FESS for sinonasal polyposis. Disorders affecting inferior turbinate include compensatory hypertrophy, protrusion of the os turbinate, hyperplasia of the end of the turbinate. Medical line of management is gold standard for treatment of allergic rhinitis but nasal surgeries for other co existing nasal condition help in increasing the treatment results in theses patients Aim: To evaluate the efficacy of nasal surgeries along with medical treatment on allergic rhinitis patients. Methods & materials - We reviewed potential article which were related to our field of interest i.e allergic rhinitis and nasal surgeries from July 2019 to December 2019 in Vydehi Medical College and Anand Ent & Allergy Centre Bengaluru, Results and conclusion - After reviewing all the relevant articles we came to a conclusion that correcting other nasal pathology such as deviated nasal septum , hypertrophied turbinate , nasal polyposis etc by the means of surgery before starting medical line of treatment for allergic rhinitis gave a better improvement in patient. We conclude by saying making a better nasal air passage to breath for the patients will exponentially increase the result of the treatment for allergic rhinitis. Key Word: allergic rhinitis, inferior turbinate hypertrophy, submucosal resection. Functional endoscopic sinus surgery.
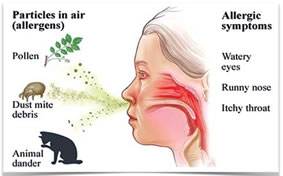
INTRODUCTION Allergy is one of the most common disease affecting 10 to 25 % of the population worldwide. Nasal obstruction and sneezing is one of the common presenting complaints to an ENT OPD1.It is defined as intolerance to a particular substance(s) and environment inducing certain reactions by the body. Allergen is a substance that causes an allergic reaction in the individual, and it could be dust, smoke and cold environment, to name a few. Allergic rhinitis is inflammation of the nasal mucosa which is manifested as itching of nose, excessive sneezing, nasal discharge and nasal obstruction when an individual is exposed to an allergen. The allergens which are considered important include dust mites, pets, pests, and some moulds and as well as seasonal pollens and moulds2 India, being a tropical and a densely populated nation, harbors about 40% of the population suffering with allergic rhinitis.
Figure 1: Different allergens and symptoms of allergic rhinitis 3
With rapid industrialization during the twenty first century, the smoke levels in the air increased alarmingly, further compounding the problem of allergy. Though pollution is a common problem of the urban area, rural population too gets affected with the problems related to allergy. Allergic rhinitis is the most commonly encountered case in ENT OPDs across the country. There have been many modalities, reported in literature, for the treatment of allergic rhinitis. Surgical intervention though not a permanent cure, but certainly has relieved the symptomatology of the patients thereby redefining the quality of life of the affected people. Patients with allergy rhinitis may present with other nasal disorders such as deviated nasal septum , inferior turbinate hypertrophy nasal polyposis etc . Such disorders have to be treated surgically , for example septoplasty for deviated nasal septum and FESS for sinonasal polyposis. Disorders affecting inferior turbinate include compensatory hypertrophy, protrusion of the os turbinate, hyperplasia of the end of the turbinate4 In this study we compare different studies on impact of nasal surgeries on patients with allergic rhinitis and the beneficial effects of these surgeries in treatment of the underlying allergic pathology.
MATERIALS AND METHOD We have reviewed varies articles from pubmed, online libraries and other sources for effect of nasal surgeries on allegory rhinitis in ENT journals. We found 12 articles which where related for our review article, out of which we selected 6 most relevant articles. We have conducted this study form July 2019 to December 2019 in Vydehi medical college and Anand ENT and Allergy centre, Bengaluru.
REVIEW OF LITERATURE A prospective clinical study conducted by Shridar reddy et al.5, which was carried out in a tertiary hospital from September 2013-2015(24 months) to see whether surgery would significantly improve in patients nasal symptoms. Patients were selected with moderate to severe allergic rhinitis who were refractory to medical management alone and with significant complications. This study was done to see if nasal surgery in these medically refractory cases with moderate-severe allergic rhinitis associated with complications like sinonasal polyposis, deviated nasal septum, chronic rhino sinusitis, and inferior turbinate hypertrophy would improve the symptoms and role of surgical management in ameliorating the allergic manifestations. Although surgery was found to be essential would not relieve of the patient from inherent allergy. So, standardization of indications for surgery in these conditions had been attempted. The majority of patients belonged to age group 11-30 with mean age of 27.84 with slightly male preponderance of 1.6:1. These patients were having mild symptoms initially and progressed to moderate to severe forms despite medical management. The reported incidence of asthma in adults with allergic rhinitis varies from 15-40%. The treatment protocol comprised of surgical management which was decided on the nature of complications. This included Sub mucosal diathermy for inferior turbinate hypertrophy, septoplasty for deviated nasal septum and FESS (Functional Endoscopic Sinus Surgery) for sinonasal polyposis and sinusitis. These patients were followed up monthly for 3 months and their daytime nasal symptom score (DTNSS) was recorded at the end of 3 months. Patients were advised to continue medical management for allergy. The daytime nasal symptom score (DTNSS) was 7.5 in pre-treatment group and was 0.24 after surgery at 3 months follow up. The ‘p’ value was less than 0.0001 which was statistically significant. In this study, it clearly demonstrated majority of patients were relieved of nasal obstruction and the incidence of allergic episodes decreased significantly and they were mild in severity. It can be concluded from this study that medical management alone is not sufficient in moderate to severe allergic rhinitis patients with complications and the symptoms of these patients significantly improve when combined with surgical management. A similar observational study conducted by MS Vishnu et al.6, involving 30 patients with nasal obstruction due to inferior turbinate hypertrophy was done at Sree Gokulam Medical College, TVM from January 2014 to June 2015. The study was done to compare the pre-operative and post-operative subjective, objective parameters, and post-operative complications of 30 patients with nasal obstruction due to inferior turbinate hypertrophy following submucosal diathermy (SMD). Patients were evaluated preoperatively. The Cold spatula test done preoperatively revealed reduced fogging in all 30 patients. Size of inferior turbinate was classified into three grades: Grade 1: Normal size inferior turbinate, not atrophic without any nasal obstruction Grade 2: Moderate sized inferior turbinate, touching the septum with nasal obstruction, responding to local decongestant Grade 3: Large mulberry turbinate touching the septum with nasal obstruction, not responding to local decongestant. In this study procedure was done for both Grades 2 and 3 patients. After decongestion, the diathermy needle was inserted into the anterior end of the inferior turbinate, which was advanced submucosally till the posterior end of the inferior turbinate was reached. The needle was then withdrawn slightly, and a current of 50 joules was applied in a triangular fashion at 3 points (superior, medial, and inferior). Postoperatively, improvement in fogging in 66.7%, 76.7%, and 86.7% patients at the end of 1 week, 1 month, and 3 months was noted. In addition, the occurrence of post-operative complications such as reactionary hemorrhage, nasal crust formation, vestibular skin burn, headache and nasal pain, synechiae formation, and atrophic rhinitis were also assessed. Nasal obstruction was evaluated at 1 week, 1 month, and 3 months postoperatively. Snoring among the study population decreased from 23.3% to 13.3% at the end of 1 month and was further reduced 6.7% at the end of 3 months. Nasal obstruction, present in all patients was reduced to 43.3%, 33.3%, and 20% at the end of 1 week, 1 month, and 3 months postoperatively and significant reduction in allergic symptoms was observed. The Remote sequelae, such as synechiae and atrophic rhinitis, were not reported in any of the patients during the assessment period. Thus the procedure was found to be an effective, safer, and less invasive technique in the management of inferior turbinate hypertrophy with less bleeding, pain, crusting and was beneficial for patients allergic symptoms. In a study conducted by vijaya kumar et al.7 was conducted due to lack of consensus has not been reached regarding the optimal reduction procedure for inferior turbinate hypertrophy in allergic rhinitis and whether such procedures result in improvement in mucosal architecture. Twenty-nine patients aged 18–45 years (mean 26.8 years), with allergic rhinitis and inferior turbinate hypertrophy not responsive to medical therapy. Patients presented with nasal obstruction due to mucosal hypertrophy of the inferior turbinate, presenting to the out-patient clinic of the ENT Department, were included in the study if they met the following criteria Age above or equal to 18 years and failure to respond to medical management with antihistamines, saline sprays. T Allergen skin testing and serum IgE estimation were done for all cases to diagnose allergic rhinitis and were on topical steroids for at least 3 months. The patients who underwent endoscopic submucosal diathermy (ESMD) (14 patients) or endoscopic submucosal resection (ESMR) (15 patients) with intraoperative and 3–6 months postoperative inferior turbinate biopsies, were included in the study. Epithelial and mucosal architecture was compared between the two groups. In both ESMD and ESMR, there is loss of mucosa and submucosa following surgery. Following ESMD, the mucosa superficial to the area that has been cauterized tends to slough off in the first week after surgery. This could account for the higher mean subjective scores for nasal obstruction after the first week in patients who underwent ESMD compared to those who underwent ESMR. The epithelium appears to be restored postoperatively by 3 months. The findings of this study suggest that both ESMD and ESMR greatly help restore histological changes that occur in patients with inferior turbinate hypertrophy caused by allergic rhinitis. This could account for the higher mean subjective scores for nasal obstruction after the first week in patients who underwent ESMD compared to those who underwent ESMR. The epithelium appears to be restored postoperatively by 3 months. This study reported that both the groups showed a significant decrease in epithelial denudation (p < 0.001), reversal of basement membrane thickening (p < 0.001) and increase in density of cilia (p < 0.001). The degree of improvement in histological characteristics between ESMD and ESMR groups was not significant. Surgical intervention for inferior turbinate hypertrophy secondary to allergic rhinitis refractory to medical management, both by endoscopic submucous diathermy as well as resection, results in the restoration of nasal mucosal epithelium on histopathological examination as early as 3 months postoperatively. There were, however, no significant differences in clinical improvement or postoperative histopathological differences between the two techniques at 3–6 months. A study done by Ritesh Mahajan8, two surgical procedures namely submucosal resection (SMR) of inferior turbinate and Powered inferior turbinectomy (PT) for the management of ITH were compared. Surgical procedures are to be analyzed in terms of results and complications by subjective and Objective assessment. This prospective study was conducted from 1st December 2011 to 1st June 2013. Subjective assessment of nasal obstruction was done by visual analogue scoring before surgery and graded into none, mild, moderate, and severe. Patients were also subjected to nasal endoscopy for objective assessment of inferior turbinate size and graded as I, II, III. A total of 60 patients were operated (30 patients in each group), patients in Group A underwent SMR and in Group B patients PT was performed. All the patients were operated under general anesthesia. SMR was performed using nasal endoscopes, the incision was made with a no 11 blade along the inferior edge of the turbinate and was carried down to bone far posteriorly up to the anterior nasal root. The mucosa was then elevated from both the medial and lateral surfaces of the turbinate bone using a Cottle’s elevator and turbinate bone was resected with the help of turbinate scissors. The flaps were cauterized and anterior nasal packing was placed for 48hours. Group B patients were subjected to the same preoperative preparation as Group A patients. An incision was made with a no 15 blade vertically in the anterior aspect of the inferior turbinate. A submucosal pocket was created with sharp dissection on the medial surface of the bony turbinate. The straight microdebrider (4-mm tip with trucut blade) was applied through the incision. The bony turbinate and some of the submucosal tissue was debrided at 3000-cps oscillating mode in a ventro-caudal (anteroposterior) manner. Debridement was performed with the blade positioned laterally from the submucosal plane. Particular attention was paid to preserve the mucosal flap. The reduction in the size of the inferior turbinate was easily recognized immediately after the procedure. Anterior nasal packs were used for 48 hours. An ideal procedure for turbinate reduction should reduce the turbinate effectively and be associated with minimal discomfort and complications. Intraoperative Complications which were noted in this study bleeding was seen in 20% of the patients in Group A and 3.3% of the patients in Group B. Mild hemorrhage is the most frequent complication associated with submucosal resection of the inferior turbinate and occurs in 2–7% of patients. Postoperatively, Nasal crust findings showed no statistically significant difference between both Groups Patients were assessed for various parameters like age, gender, laterality, intra operative and postoperative complications. Overall improvement of 66.7% in Nasal Obstruction and 76.7% in size of inferior turbinate was seen in Group A, whereas improvement of 90% in nasal Obstruction and 83.3% in size of turbinate was seen in Group B. Both SMR and PT are efficient methods for relieving nasal obstruction related to ITH. However, the results in this study confirm that PT is a safe and effective procedure in relieving nasal obstruction and enabling optimal volume reduction with preservation of function of the inferior turbinate. A comparative prospective clinical study was conducted at Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur from June 2015 to June 2017 by Balasaheb Patil et al.9. The purpose of this study was to see the Effect of Septoplasty on Quality of life in patients of Allergic Rhinitis with Deviated nasal septum. Total 100 cases were studied between the age groups of 20-40 years attending the ENT O.P.D with complaints of nasal obstruction, repeated attacks of sneezing, running nose were screened by a detailed history, clinical examination, anterior rhinoscopy and nasal endoscopy and were selected on confirmation of the diagnosis of DNS with allergic rhinitis . 50 underwent septoplasty along with conservative treatment (study group) and 50 were treated by conservative treatment only (control group). Both groups were given a questionnaire in the beginning and at the end of three months. After analyzing the results, it was concluded that septoplasty significantly improves the quality of life and hence should be considered along with conservative treatment in patients of Allergic Rhinitis with Deviated Nasal Septum. A study conducted by Neeharika Gunturu et al.10 in which the aim of the study was to evaluate the post operative outcome by both subjective and objective improvement in symptoms isolated inferior turbinate hypertrophy is one of the leading cause of nasal obstruction. Another most common cause found to be allergic rhinitis which is characterized by seasonal or perennial nasal obstruction with itchy nose, sneezing, and rhinorrhea. Patient was put in anti trendelenburg position. After achieving good nasal decongestion and giving local infiltration Using 0/30 nasal endoscope, a vertical cut was taken over anterior end of inferior turbinate with an ophthalmic keratome. Medial Muco periosteal layer of inferior turbinate elevated from bony part of turbinate with freer’s elevator through out the length and lateral flap was excised either with using turbinectomy scissors/endoscopic sinus scissors. The elevated medial flap of turbinate was reposited back upon itself, a new small and functioning turbinate which provides good nasal airway was created. Surgicele/gelfoam soaked in haemostatic solution like Tranexamic acid/Ethamsylate was placed over the raw area on IT. Septoplasty was done in patients with DNS. Final nasal packing was done with 8 cm ivalon packs. Nasal packs were placed for 48 h post operatively. External dressing was changed in case of soakage. Post operative course After gently removing nasal packs on 2nd POD, patients were observed for anterior/posterior nasal bleeding for 2 h and discharged after explaining post operative precautions. Allowed to gently blow their nose from second day onwards, to irrigate/wash nose regularly with saline, to contact immediately in case of active nasal bleeding and to apply Topical antibacterial ointment (Neosporin-H). All patients were asked to come for follow up on 1, 6, 12 and 24 weeks post operatively. Failure of swollen turbinate mucosa to shrink after application of decongestant after turbinoplasty in allergic rhinitis patients with inferior turbinate hypertrophy and in patients with isolated Inferior turbinate hypertrophy suggests the possibility that the patient may have chronic unresponsive soft tissue/bony hypertrophy, or drug induced rhinitis. Patients who were not getting improved symptomatically with medical management have undergone submucosal turbinoplasty at the institute. Hence, patients having AR with ITH and patients having isolated ITH showed benefits qualitatively after submucosal turbinopalsty done. So, In Patients who have had failed medical treatment for AR (perennial AR) the addition of submucosal turbinopalsty along with immunotherapy and pharmacotherapy greatly enhances the quality of life.
RESULTS AND CONCLUSION Allergic rhinitis is one of the most persistent disease ENT surgeons encounter in everyday practice. An effective way to treat and manage this disease is of paramount importance as it has a high incidence rate in our community. All patients with allergic rhinitis not only have only AR but also other nasal conditions such as deviated nasal septum , nasal polyposis and the most common hypertrophy of inferior turbinate. Hypertrophy of the inferior turbinate is the first sign to be seen in a allergic patient. Addressing these other conditions along with standard medical treatment of AR is most important. Surgical management of these coexisting conditions will help in giving better results for the patients. As of all the studies which we have studied and varies standard book referred we have come to a conclusion that surgical treatment of DNS by septoplasty, FESS for nasal polyposis and submucosa diathermy / inferior turbinectomy in treatment of inferior turbinate hypertrophy is of paramount importance before starting AR. So we conclude by saying that surgical treatment of coexisting conditions and medical line of management of AR go hand in hand in giving better result and satisfaction for our patients.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home