|
Table of Content - Volume 18 Issue 3 - June 2021
A study of structural and functional status of vocal cords with stroboscope in vocal cord pathologies
Sheetal Shelke1, Hetal Marfatia2, Nilam Sathe3, Asmita Madhavi4*
1Assistant Professor, Department of ENT, MIMSR Medical College, Latur, INDIA. 3Associate Professor, 2Professor, 4Assistant Professor, Department of ENT, Seth G.S. Medical college, Mumbai, INDIA. Email: asmitamadhavi@yahoo.co.in
Abstract Background: Voice is the main support of communication in mankind, through which feelings, emotions and culture are transmitted. The application of stroboscopy to the study of vocal fold vibration has led to dramatic advances in the understanding of vocal fold pathologies. Stroboscopy is the state-of-the-art diagnostic tool and this technique provides valuable information about the nature of the vibration and a visual image that can be used both for immediate analysis and as a permanent record for comparison of repeated examination at a later date. Aim: A study of structural and functional status of vocal cords with stroboscope in vocal cord pathologies. Material and Methods: A total of 30 cases (18-60 yrs) presented with complaints of change in voice and hoarseness of voice were examined. For structural and functional status of vocal cords the stroboscopic parameters like symmetry, amplitude of vibration, mucosal wave, glottis closure and periodicity were studied and statistically significant relationship with different vocal pathologies were obtained. Results: Vocal cord nodule was most common pathology in our study, followed by cord polyps. All patients those had vocal cord cysts (2) and polyps (6) underwent microlaryngoscopic surgery showed symmetry of vocal cords in all patients (100%). Increased in amplitude was not observed in any patient. Vocal cord mucosal wave was normal in all patients with sulcus (2), vocal cord palsy (5), spasmodic dysphonia (1) and anterior commissure web (1). All 10 patients of vocal cord nodule shows hour glass type of glottis closure. Periodic vibration was observed in all 10 cases of nodules, 2 cases of sulcus, 1 case of Reinke‘s edema and 1 case of web (100%). laryngoscopic diagnosis changed in 6 cases (20%) after examination with stroboscope. Conclusion: Stroboscopy is most useful in identifying laryngeal pathologies of the vocal fold cover. Vocal cord structural and functional pathologies can be more accurately diagnosed with stroboscope. Keywords: Vocal pathology, Stroboscopy, Structural status, Functional status.
INTRODUCTION The mobility and deformability of the vocal folds determines the ease with which vocal fold vibration can be initiated.1 Stroboscopy constitutes part of a multidimentional approach which has been adopted in the systematic study of voice disorders.2 Its clinical value has been reported to be the improved diagnosis of benign vocal fold lesions, vocal fold scars, muscle tension dysphonia and early invasive lesions.3-5 Voice disorders are common 6. In most of the cases patients are treated by non-voice specialized otolaryngologists. Diagnosis is the basis of treatment decisions. Previous studies have demonstrated a significant inter-observer variability in the diagnosis by non-voice specialists viewing laryngoscopic videos.7 This variability can be reduced by stricter definitions of diagnoses, training in voice clinics and use of improved diagnostic technology.7 Treatment of voice disorders should aim to satisfy each patient's unique vocal requirements. Severe dysphonia influences an individual's health related quality of life and effective treatment, based on the correct diagnosis, improves patients' perceptions about their quality of life.8 Videostroboscopy has evolved as the most practical and useful technique for the clinical evaluation of the viscoelastic properties of the phonatory mucosa.9 It is most useful in identifying and differentiating malignant and non-malignant vocal-fold pathologies.10The aim of this study was to evaluate the diagnostic value of stroboscopy by studying the structural and functional status of vocal cords in its pathologies.
MATERIAL AND METHODS Type of study Prospective observational study Inclusion criteria All patients between 18-60yrs of age presented to ENT OPD KEM Hospital with complaints of change in voice during first 3 months of study. Exclusion criteria Patients who fail to follow up to 9 months. Patients with mass lesion obscuring vocal cords. Patients with hyper functioning vocal cords. End point Of Study Follow up of patients Up to 9 months. Data Recording Data was recorded as in a predesigned case record form. Methods Study is carried out in 30 cases presented with complaints of change in voice and hoarseness of voice in Department of ENT, KEM Hospital Mumbai. In all patients detail history was noted. All patients underwent Indirect laryngoscopy and 700 laryngoscopy examination. Stroboscopic examination was carried for these patients. For of better visualization, a rigid stroboscopic examination was conducted with the 700 laryngoscope. 700 rigid endoscope connected to a strobe unit is used to visualize the patients larynx and video recorded will be studied for Stroboscopic parameters. Videostroboscopy was done with by seating the patient in the examination chair at a height comfortable for the examiner. The patient leans forward with the neck flexed and the head extended at the atlanto-occipital joint (Kirstein position). Once in the appropriate position, it is often helpful to apply topical anesthesia (10% lignocaine) to the posterior aspect of the anterior tongue as well as the posterior oropharynx. The examiner should ensure that the microphone is calibrated properly and have the patient hold the laryngeal diaphragm against the thyroid lamina. With mouth open and tongue protruded, the examiner retracts the tongue anteriorly and carefully inserts the rigid telescope. Optimal examination hinges on the examiner‘s attention to achieving proper focus of the vocal folds. Proper focus demonstrates clear visualization of the sub epithelial vasculature of the vocal fold. To avoid condensation on the scope, the tip of the telescope is dipped in hot water / savlon just prior to beginning the examination. Patients during examination are instructed to say-
Evaluation criteria in stroboscopic examination include symmetry, amplitude, periodicity, vocal cords closure and mucosal wave propagation of vocal cords. Depending on pathology of vocal cords patients have been treated either with conservative (speech therapy, ant reflux treatment, voice rest) or surgical management (Microlaryngoscopic surgery). After treatment patients were re-evaluated with stroboscopy at the end of 9 months follow up. All parameters of stroboscopy including symmetry, amplitude of vibration, mucosal wave, glottis closure and periodicity were observed in these patients. Stroboscope is available in ENT Department KEM Hospital, so study has been done without any extra charges to patients. Study is carried out without hampering patient‘s management.
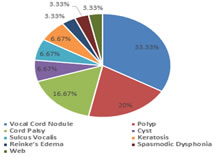
RESULTS Table 1: Vocal Cord Pathologies Distribution
Figure 1:
Table 2: Symmetry Of Vocal Cords
Table 3: Mucosal Waves of Right Vocal Cord Vibration
Table 4: Mucosal Waves of Left Vocal Cord Vibration
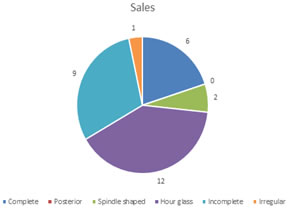
Table 5: Before Treatment Glottic Closure
Figure 2:
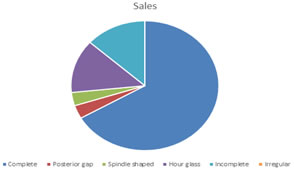
Table 6: After Treatment Glottic Closure
Figure 3: Sales Table 7: Periodicity Of Vocal Cord Vibration
Table 8: Initial And Final Diagnosis In Patients Of Dysphonia
Additional information related to vocal cord lesion was observed in 4 cases. In 2 cases of vocal cord polyp pedunculated and sessile nature of polyp was observed. In cases of keratosis one had superficial lesion not invading deep layers of vocal cord while another patient had keratosis invading deep layers of cord.
DISCUSSION Benign vocal fold disease, such as vocal polyp, vocal nodule, intracordal cyst or Reinke’s edema is one of the most common causes which deteriorate the voice.11 This study of 30 patients, 10 patients had vocal cord nodules (33.33%),6 patients had vocal cord polyps (20%), 5 had vocal cord palsy (16.67%), 2 patients had vocal cord sulcus (6.67%), 2 patients had vocal cord cyst (6.67%), 2 patients had vocal cord keratosis (6.67%),1 patient had Reinke‘s edema (3.33%),1 patient had spasmodic dysphonia (3.33%),1 patient had anterior commissure web (3.33%). Vocal cord nodule was most common pathology in our study, followed by cord polyps. In this study, 10 patients with nodules, 2 patients with sulcus, 1 with Reinke‘s edema, 1 with spasmodic dysphonia and 1 with anterior commissure web (100%) showed symmetry of vocal cords on stroboscopic examination. All 5 patients with vocal cord palsy had asymmetry of vocal cords. 1 patient with vocal cord cyst and 1 patient with keratosis (50%) had symmetrical vocal cords. While other 1 patient of cyst and keratosis showed asymmetrical of vocal cords. In cases of polyps, out of 6 patients 5 had asymmetry of vocal cords (83.33%) and remaining1 patient (16.66%) showed symmetry of cords. Symmetry in this case of polyp was due to bilateral cord involvement. All patients those had vocal cord cysts (2) and polyps (6) underwent microlaryngoscopic surgery. Reassessment of these patients after 9 months of postoperative period with stroboscopy, showed symmetry of vocal cords in all patients (100%). This is probably due to excision of lesion along glottal margin. All patients with vocal cord palsy were managed with conservative line of management. Out of 5 patients, in 1 patient symmetry of vocal cord observed after 9 months due to recovery of function, remaining 4 had asymmetry of cords. [Table 1 and 2] Also, 2 patients of keratosis, 5 of vocal cord palsy, 1 of Reinke‘s edema, 1 of spasmodic dysphonia and 1 of anterior commissure web (100%) on stroboscopic examination showed decrease in amplitude of vibration. Out of 6 patients of polyp, 4 (66.67%) had decreased amplitude of vibration. While remaining 1 patient of polyp had normal amplitude of vibration. In patients with vocal cord nodule, majority of patients that is 9 out of 10 patients (90%), decreased amplitude of vibration was observed. 1 out of 2 patients of keratosis (50%) had deceased amplitude. In our study, increased in amplitude was not observed in any patient. Decrease in amplitude was observed in 1 patient with keratosis and in another patient of keratosis amplitude of vibration was not affected probably due to superficial nature of lesion not invading lamina. This finding differed from observation by Coden D et al., that is reductions in the amplitude of vocal fold vibration was usually noted in intraepithelial atypia, despite the fact that there was no invasion into the superficial lamina propria. So reduced amplitude of vocal fold vibration and or mucosal wave propagation associated with keratosis did not reliably predict the presence of cancer or the depth of cancer invasion into the lamina propria.12 Stroboscopic examination of patients after treatment and 9 month follow up was done. In operated 6 cases of vocal cord polyp and 2 of cyst, amplitude of vibration was normal in follow up stroboscopy. This was probably due to postoperative loss of mass effect of lesion on vocal cord. Improvement in vocal cord vibration after surgery was certainly due to better approximation of vocal cord edges. In study by Noordzij Jp, Woo P. (2000); they observed complete glottic closure results in greater vocal fold contact because of a regular edge, with generation of a greater subglottic pressure and better amplitude of cord vibration.13 In case of vocal cord palsy, in 1patient (20%) amplitude improved on follow up due spontaneous recovery of function of vocal cord while remaining 4 cases showed decreased amplitude of vibration. There was no improvement in amplitude after treatment in case of keratosis. This was probably due to postoperative scarring. [Table 3 and 4] In this study, vocal cord mucosal wave was normal in all patients with sulcus (2), vocal cord palsy (5), spasmodic dysphonia (1) and anterior commissure web (1). Wave was decreased in all the 2 cases of cyst, 2 cases of keratosis, 1 case of Reinke‘s edema. In cases of polyp, 4 patients (66.67%) had decreased mucosal wave. Out of 10 Patients with nodule only 2patients (20%) had decreased mucosal wave of vibration. Increase in wave was not observed in any of the patient. All patients with polyp(6), cyst(2) who underwent surgery and patient of Reinke‘s edema who was managed with speech therapy and voice rest showed normal mucosal wave in follow up stroboscopy. This must be due to loss of mass effect of lesion on vocal cord. In study by George Thomas et.al (2007)14, they observed that mucosal wave improved to 90% on the right and 86.9% on the left vocal cord. All 10 patients of vocal cord nodule shows hour glass type of glottis closure. In cases of vocal cord polyp out of 6patients, 3 patients (50%) had incomplete closure, 2 patients (33.33%) had complete closure which was because of the polyp situated on superior surface of vocal cord with free edges and 1 case with bilateral polyp had hour glass gap. In 1case of bilateral cord cyst hour glass gap observed while another case of unilateral cyst had incomplete closure. All the 2 cases of sulcus showed spindle shaped gap. In keratosis cases, 1patient (50%) had omplete closure due to superior surface lesion another patient (50%) had incomplete closure due to large keratosis involving edges of vocal cord. All 5 cases (100%) of vocal cord palsy had incomplete closure. All cases of Reinke‘s edema (1), spasmodic dysphonia (1), web(1) had complete closure of glottis.[Table 5 and 6] Also in this study all operated patients of polyp (6) and cyst (2) complete closure was observed in postoperative follow up due to removal of lesion at vocal cord edge. After speech therapy and voice rest, in 6 cases (60%) of vocal cord nodules complete closure was observed; while remaining 4 cases hour glass insufficiency was observed. In case of keratosis both cases after surgery had incomplete closure due to tissue loss and scarring. 1case (20%) of vocal cord palsy which recovered its function had complete closure of glottis on follow up stroboscopy. These findings were similar to those shown by study of George Thomas et.al (2007)14, on outcome analysis of benign vocal cord lesions by videostroboscopy. The glottic closure which was incomplete, improved to complete closure in 96.66%. This was statistically significant (p<0.0001). The periodic vibration was observed in all 10 cases of nodules, 2 cases of sulcus, 1 case of Reinke‘s edema and 1 case of web (100%). Aperiodic vibrations were seen in patient of spasmodic dysphonia and 5 cases of palsy (100%). In cases with polyp; 5 cases (83.33%) had periodic vibrations, in rest aperiodic vibrations were observed. This was probably due to mass effect of polyp. Out of 2 cases of cyst one had periodic and another had aperiodic vibrations, similar findings were observed in cases of keratosis. After treatment stroboscopy in our study showed periodic vibrations in 10 cases (100%) of nodules, 2 cases of cyst, 6 cases of polyp, 2 cases of sulcus and 1 case of Reinke‘s edema, web and spasmodic dysphonia each. Periodicity was observed in 1 case of vocal cord palsy (20%) due to recovery of vocal cord function. In case of keratosis no improvement in periodicity was observed may be due to postoperative fibrosis of vocal cord.[Table 7] Also, laryngoscopic diagnosis changed in 6 cases (20%) after examination with stroboscope. 2 patients who were diagnosed as normal vocal cord had sulcus on stroboscopic examination. 2 cases of vocal cord cyst diagnosis changed to polyp. 1 patient had vocal cord cyst and another had polyp on stroboscopic examination which were initially diagnosed as nodule. In 2 cases (6.67%) which were diagnosed as nodule initially and later as polyp and cyst, line of management changed from conservative to surgery.[Table 8]
CONCLUSION Stroboscopy continues to be the imaging modality of choice by voice clinicians due to its historical use and ability to efficiently capture many salient vocal fold vibratory characteristics. Vocal cord structural and functional pathologies can be more accurately diagnosed with stroboscope, which were not appreciated on laryngoscopic examination.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home